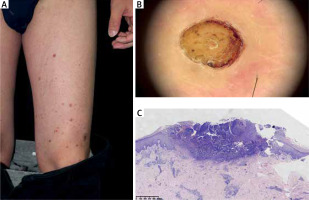
We report a rare case of acquired reactive perforating collagenosis (ARPC) in a 38-year-old male who developed multiple papules with central crusts, mostly asymptomatic but occasionally mildly pruritic, on his left thigh 3 weeks after recovering from COVID-19 infection (Figure 1 A). He had no history of renal impairment, diabetes mellitus, or other systemic diseases. Dermoscopy revealed yellow homogeneous structures, red dots, crust, and collar-like structures (Figure 1 B). Histopathology confirmed the diagnosis of ARPC and showed transepidermal elimination of collagen bundles surrounded by inflammatory cells (Figure 1 C). He was treated with topical corticosteroids for 1 month without significant improvement and was lost to follow-up.
Figure 1
A – Multiple papules with central crusts on the left thigh. B – Dermoscopy revealed yellow homogeneous structures, red dots, crust, and collar-like structures. C – Histopathology showing transepidermal elimination of collagen bundles surrounded by inflammatory cells (H&E stain)
ARPC is a rare cutaneous disorder characterized by transepidermal elimination of altered collagen fibres through the epidermis. There are many factors potentially inducing ARPC, with the majority of cases being associated with diabetes mellitus and chronic renal failure. There have also been reports of tumours, thyroid dysfunction, infectious diseases, sclerosing cholangitis, lung fibrosis, and other coexisting diseases [1]. However, some cases of ARPC have been reported in patients without any underlying diseases [2].
A remarkable feature of our case is that the patient had only unilateral involvement of his left thigh. This is unusual for ARPC, which typically affects both sides symmetrically. There have been reports of unilateral ARPC occurring after herpes zoster, which may be a form of Wolf’s isotopic response [3]. In our case, the site of ARPC had no preexisting dermatosis, which differs from the Wolf’s isotopic response. It has been reported that a 32-year-old male presented with unilateral blurring of vision 2 weeks after COVID-19 infection as the effect of microvasculopathy [4]. The pathogenesis of ARPC is unclear, but it is hypothesized that microvasculopathy and the resultant hypoxic state in the dermis may be a predisposing factor of ARPC [5]. We speculate that COVID-19 infection may have triggered microvasculopathy and the resultant hypoxic state that resulted in collagen degeneration and extrusion in our patient. COVID-19 is a novel coronavirus disease that can cause various cutaneous manifestations, such as maculopapular rash, urticaria, vesicles, chilblains-like lesions, livedo reticularis, and vasculitis [6]. However, to our knowledge, there is no report of ARPC associated with COVID-19 infection in the literature.
The diagnosis of ARPC is based on the characteristic histopathological features of transepidermal elimination of collagen fibres. Dermoscopy can also aid in the diagnosis. Under dermoscopy, ARPC typically presents with a central yellow-to-brown structureless area surrounded by a white rim and collarette of scale, with the periphery potentially exhibiting a pinkish structureless area, dotted vessels, and brown reticular lines [7]. The treatment of ARPC is challenging and often unsatisfactory. There is no standard therapy for ARPC and various modalities have been tried with variable results. These include antihistamines, topical keratolytics, corticosteroids, tretinoin, oral drugs such as allopurinol or antibiotics, and phototherapy or photochemotherapy, along with treatment of any underlying diseases if present [8]. In our case, the patient did not respond to topical corticosteroids and was lost to follow-up.
We report a rare case of unilateral ARPC in a 38-year-old male who developed the skin lesions 3 weeks after recovering from COVID-19 infection. This is the first report of ARPC associated with COVID-19 infection in the literature. The pathogenic link between COVID-19 infection and ARPC is unclear and needs further investigation. The treatment of ARPC is difficult and often ineffective. More studies are needed to find the optimal therapy for this rare condition.








