Intussusception is a rare occurrence in adults, constituting only 1% of all cases of intestinal obstructions and 5% of all instances of intussusceptions. This condition manifests when a proximal segment of the bowel, along with its associated mesentery, telescopes into the lumen of the adjacent distal segment [1, 2]. A 69-year-old male patient presented to the emergency department with diffuse severe abdominal pain, emesis, and suppression of the passage of gases and faeces persisting for the past 3 days. Upon clinical examination, the patient presented with widespread abdominal tenderness accompanied by signs of resistance and spasms. White blood cell (WBC) count was recorded at 5.68, with polymorphonuclear neutrophils (PMNs) constituting 59%. No hernia was observed. The patient had not undergone surgery in the past. An X-ray examination of the patient revealed the presence of air-fluid levels and discernible distension within the bowel loops (Figure 1). Abdominal computed tomography (CT) scan revealed small bowel obstruction with the diagnosis of ileocolic intussusception (Figure 2). Subsequently, the patient underwent segmental small bowel resection.
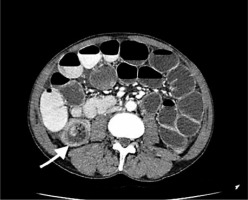
Figure 2
CT-scan identified dilated bowel loops and the site of intussusception (white arrow) with subsequent wall thickening
Intraoperative findings established the diagnosis of ileocolic intussusception (Figure 3). A segmental small bowel resection with simultaneous anastomosis was performed. The histopathological examination revealed focal necrotic changes and haemorrhagic areas within the affected bowel segment. Notably, no evidence of neoplastic transformation was identified. Following surgery, the patient remained hospitalised for 7 days with no major postoperative complications and was then discharged. Intussusception, defined as the telescoping of one portion of the intestine into another, is a primary cause of bowel obstruction in infants; its occurrence in adults, particularly the elderly, is rare. Adult intussusception manifests in 3 distinct types: enteric, ileo-colic, and colo-colic [1]. Clinical indicators of mechanically induced intestinal blockage encompass nausea, vomiting, and abdominal cramping. Diagnosis of adult intussusception necessitates a heightened clinical suspicion, a comprehensive medical history review, and a thorough physical examination. The considerable heterogeneity in both clinical presentation and imaging findings poses challenges for the preoperative identification of intussusception. Reijnen et al. reported a relatively high preoperative diagnosis rate at 50%, while Eisen et al. documented a diagnostic rate of 40.7% [2, 3]. Initial diagnostic measures often involve plain abdominal X-ray due to the prevalent presentation of obstructive symptoms, offering insights into the location of the obstruction [4]. Barium enema examinations may contribute to intussusception detection, revealing a distinctive “cup-shaped” filling defect [5, 6]. Additionally, upper gastrointestinal contrast series may exhibit a characteristic “stacked coin” appearance. Gupta et al. reported that Ileocolic intussusception accounts for 32% of documented adult intussusception [7]. Abdominal CT scan stands out as the diagnostic modality with the highest sensitivity for intussusception, exhibiting a range of 58% to 100% effectiveness [8, 9]. Characteristic radiological features include the visualisation of a target sign or a sausage-shaped soft tissue mass with a layering effect, often accompanied by the presence of mesenteric vessels lining the bowel lumen [10]. Crucially, the CT scan serves as a valuable tool in distinguishing between lead point and non-lead point intussusceptions. In instances of sub-acute or chronic large bowel obstruction, flexible lower gastrointestinal endoscopy assumes significance for confirming the intussusception diagnosis, pinpointing its location, and identifying any underlying lesions that may offer treatment options [10]. The recommended treatment for adult intussusception is definitive surgical resection, a choice driven by the significant prevalence of structural causes and the relatively high incidence of malignancy. Preoperative reduction with barium or air is discouraged as a definitive treatment due to the large proportion of cases with structural causes, and untreated lesions pose a risk of recurrence [11–13]. Theoretically, performing reduction during surgery before resection could allow for a more limited resection, but this approach is discouraged. The risk of potential intra-luminal seeding or venous tumour dissemination during the manipulation of a malignant lesion outweighs the potential benefits of reduction [12]. Intussusceptions in the adult population are infrequent, and the diverse array of presenting symptoms poses challenges for diagnosis. Non-invasive imaging techniques have become indispensable for achieving a preoperative diagnosis and offering insights into the potential malignancy of the condition. Surgery stands as the first-line treatment modality, with a mandatory exploration to identify the underlying cause.












