We present a case of two perforations that occurred simultaneously during a staged percutaneous coronary intervention (PCI) on a significant bifurcation lesion. The lesion involved our patient’s ramus intermedius and one of its branches. To our knowledge, it is one of the very few cases of simultaneous coronary perforations reported in the literature [1].
Our patient was a 56-year-old diabetic man, who initially presented with a subacute, extensive, anterior-wall myocardial infarction and underwent PCI with a drug-eluting stent in the proximal left anterior descending artery (LAD). Starting the staged procedure, a severe stenosis of the left circumflex artery (LCx) was stented. Then, two straight-tip, hydrophilic workhorse guidewires were advanced in the ramus and its branch. An upfront two-stent strategy (TAP technique) was deemed appropriate for the treatment of this bifurcation lesion. A 2.75 × 20 mm drug-eluting stent (DES) was implanted in the ramus branch, Proximal Optimization Technique was performed and the guidewires were exchanged. A 2.5 × 20 mm DES was implanted in the side branch. After kissing balloon inflation was performed, wire fracture was observed in the distal part of the ramus branch. Careful contrast injection revealed perforation and extravasation (Ellis type III perforation) [2] at the site of the fractured guidewire. It also revealed simultaneous extravasation from another perforation site, distally, in the side branch. As for the reason behind the fracture, we later speculated that it happened due to possible mechanical strain on the tip of the wire during the preceding PCI of the LCx and the wire exchange (Figure 1).
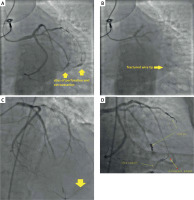
Figure 1
A – Image revealing the bifocal, simultaneous perforation in the distal ramus, and the distal part of its branch. B – In the distal ramus, the fractured guidewire’s remnants. C – No reflow phenomenon in the LAD during the primary procedure, revealing the retrograde filling of the vessel through the later “important” collateral vessel supplied from a branch of the ramus. D – Implantation of a covered stent in the distal LAD, in order to seal off an apical branch that was supplying the perforation site, through reverse recruitment of a collateral. Also visible are the pericardiocentesis catheter and the previously implanted coils
Haemodynamic instability ensued, and the cardiothoracic surgeons were notified, as mandated by the current practice in managing coronary perforations [3]. The patient was started on vasopressors and fluids. Two new guidewires were advanced in the vessels and two non-compliant balloons were advanced just proximally to the perforation sites and were inflated, in an effort to contain the extravasation. Anticoagulation was not reversed, as delivery of devices in the coronary circulation was expected to continue. Emergency pericardiocentesis was performed, resulting in temporary stabilization. Approximately 20 min later, we deflated the balloons and a new injection revealed persistent extravasation. To seal off both perforation sites, a microcatheter (Caravel, ASAHI INTECC) was employed and distal embolization of detachable coils (Ruby, Penumbra) was performed in both vessels, initially managing to control the extravasation.
Shortly thereafter, the patient began destabilizing haemodynamically and, as suspected, extravasation had recurred, this time solely from the side branch perforation site. After careful review, the reason proved to be an epicardial collateral vessel between the distal LAD and the distal part of the ramus branch, that was effectively bypassing the site of embolization. This collateral was retrogradely supplying the infarcted LAD in the primary procedure through one of the LAD’s terminal, apical branches. Interestingly, it had sealed off after restoration of flow in the LAD, and now it was “reversely” recruited following cessation of flow in the ramus branch. In order to maintain some flow to the apex and seal off the collateral vessel, a 2.5 mm covered stent was deployed from the distal LAD to the contralateral-to-the-supplying-terminal-branch. Flow to the collateral vessel stopped and the patient finally stabilized. The patient remained stable in the Coronary Care Unit, the pericardial drainage was removed the following day and he was discharged 4 days later.








