Introduction
Most cardiac surgeries are performed through a median sternotomy. 49% of these patients experience severe pain at rest postoperatively, up to 78% on coughing [1]. Poorly controlled postoperative pain led to activation of the sympathetic nervous system. It increases stress response leading to myocardial ischemia, cardiac arrhythmias, hypercoagulability, pulmonary complications, and increased rates of delirium and wound infection [2]. Sternotomy pain occurs because of tissue injury in the skin, subcutaneous tissues, bone, and cartilage. Intercostal nerves T2-T6 arising from thoracic nerve roots innervate the sternum, ribs, and surrounding subcutaneous tissue. Regional anaesthesia techniques in cardiac surgery include central neuraxial and fascial plane blocks. Epidural anaesthesia and thoracic paravertebral block can provide adequate postoperative analgesia and improve postoperative mortality [3, 4] but may result in hematoma in anticoagulated patients, dural puncture and pneumothorax [5]. Erector spinae plane block (ESPB) is a fascial plane block that acts via blockade of the dorsal and ventral rami of the thoracic spinal nerves and sympathetic fibres [6] performed by injecting a local anaesthetic into the fascial plane deep to the erector spinae muscle overlying the transverse processes of the thoracic vertebrae [7]. This has gained popularity and has shown promising results, however, lacks the ease of positioning after the closure of the sternotomy wound. Thoracic wall blocks such as pectoral inter-fascial and transverse thoracic muscle plane blocks can also be used. Pecto-intercostal fascial block (PIFB), described by De la Torre et al. [8], blocks the anterior cutaneous branch of the intercostal nerve and is administered with the patient in the supine position.
Material and methods
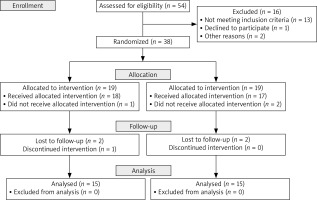
This randomised prospective study was conducted at a tertiary level teaching hospital between July 2020 and December 2020. After the Institute Ethics Committee’s approval, the trial was prospectively registered in the Clinical Trial Registry of India (CTRI/2021/06/034296). A total of 54 adult patients were assessed for eligibility, as per the inclusion and exclusion criteria (Table I), i.e., adult consenting patients, belonging to ASA-PS 2 and 3, who were planned to undergo elective cardiac surgeries through a midline sternotomy incision and extubated within 2 h. Thirty-eight consenting patients were recruited and assigned to one of the two groups using computer-generated randomization.
Table I
Inclusion and exclusion criteria
Group 1: Bilateral Pecto-intercostal fascial block (PIFB) with ropivacaine 0.2% 20 ml on each side.
Group 2: Bilateral Erector spinae plane block (ESPB) with ropivacaine 0.2% 20 ml on each side.
The patients were monitored on the day of surgery with standard ASA monitoring parameters. The proposed cardiac surgery progressed as per the standard of care, with intraoperative monitoring of hemodynamics, using invasive arterial monitoring and transesophageal echocardiography. Total opioids (fentanyl) consumed intraoperatively were noted for each patient. Soon after the closure of the sternotomy site, with all aseptic measures, bilateral ultrasound-guided PIFB or ESPB with 20 ml of 0.2% ropivacaine, was performed by a trained anaesthesiologist, as per the randomization code. The description of the block is as under, in brief. In Group 1, with the patient laying supine, a high-frequency linear probe was placed 3 cm lateral to the sternum in the parasagittal plane. Pectoralis major, intercostal muscle, pleura and ribs were identified (Figure 1). A 22G 10 cm echogenic needle was inserted between the 5th–6th rib interspace using an in-plane technique from the caudal to the cranial direction and the drug was deposited at the T5-T6 and T4-T5 interspace between the pectoralis major and intercostal muscle. Following this, the needle was inserted in the 3rd–4th rib interspace and repositioned in a cephalad direction to target the 1st–2nd rib interspace and the drug was deposited. A total of 20 ml of 0.2% ropivacaine was injected on each side. In group 2, after the closure of the surgical wound, the patient was positioned lateral, and a high-frequency linear probe was placed 3 cm lateral to the spine at T4 level in the parasagittal plane. Trapezius, rhomboids, and erector spine muscle with the tip of the transverse process of the spine were identified. A 22G 5 cm echogenic needle was inserted out-of-plane to hit the transverse process, and 20 ml of 0.2% ropivacaine was injected on each side. After completion of the respective blocks, the patients were transferred to the post-anaesthesia care unit (PACU). Both groups received Inj Fentanyl 0.3 μg/kg/h for 24-hrs and Inj Paracetamol 15 mg/kg IV 8 hourly along with one of the two regional anaesthesia techniques as a part of the multimodal analgesia approach. The patients were assessed for fast-tracking extubation criteria as per the institutional protocol and were weaned off from mechanical ventilation. Thereafter the patients were shifted to the critical care unit for overnight observation. Post-operative pain scores were assessed by an independent acute pain service (APS) team who was unaware of the block administered, at pre-defined time intervals, i.e., 2, 6, 12, 24 h post-extubation, using the numerical rating scale (NRS) at rest and with deep breathing. The pain score was specifically questioned for the surgical incision pain. Time to rescue analgesia, number of rescue doses needed, total fentanyl consumed in the 24 h and other rescue analgesics used, if any, were noted. In addition, total intraoperative opioid consumption was also noted and compared between the two groups.
Figure 1
The sonoanatomy of the PIFB with needle placement between the pectoralis major muscle (PMM) and the intercostal muscle (ICM). The underlying pleura is seen as a glistening white structure between the two ribs

Statistical analysis
The data are expressed as mean ± standard deviation, frequency, or frequency and percentage. Statistical Package for the Social Sciences version 20 (SPSS-IBM, Armonk, NY, USA) was used for statistical analysis. An independent sample t-test was used to analyse quantitative data. Qualitative data were analysed using the χ2 test. P < 0.05 was statistically significant.
Results
A total of 54 patients were assessed for eligibility, and 13 patients were excluded for not meeting the inclusion criteria, one declined to participate, one had a medical emergency post-enrolment and one opted for surgery at another centre. A total of 38 patients were randomised into two groups, out of which 35 received the intervention. The data from patients who were successfully weaned from mechanical ventilation in the PACU were collected. Data from a total of thirty patients were analysed (Figure 2). The two groups did not differ in age, weight, gender, or height (Table II). The postoperative pain scores using VAS at rest at preset time intervals of 2, 6, 12 and 24 h were not statistically different, with a p-value equal to 0.25, 0.61, 0.27, 0.63, respectively. Also, VAS at deep breathing at 2, 6, 12 and 24 h postoperatively were similar, p-value equal to 0.18, 0.05, 0.14, 0.82, respectively. Seven patients in group P and 3 patients in group E did not require any rescue analgesia in the first 24 h, and the maximum number of rescue analgesia was 5 for 1 patient in group E. No significant difference between the two groups in terms of time to use of first rescue analgesia (p = 0.4169) and the total number of rescue doses of analgesia was observed (p = 0.3170) (Figure 3). Our results recorded that the total mean amount of fentanyl used intra-operatively was similar in group P and group E, P = 0.3099 (210 ±64 μg vs. 230 ±42 μg, respectively). Total fentanyl consumed 24-hrs postoperatively was also similar with no statistical difference between both groups, p = 0.1137, Group P: 377 ±93 μg vs Group E: 435 ±100 μg (Figure 4, Table III).
Figure 3
Box and Whisker plot showing the comparison of time to rescue analgesia (A) and total rescue analgesia doses (B) between the two groups
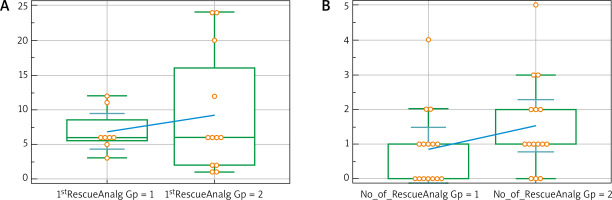
Figure 4
Box and Whisker plot showing the comparison of total fentanyl consumption in microgram per kilogram body weight between the two groups
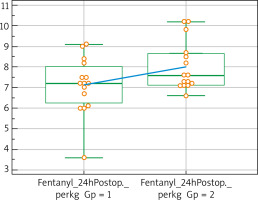
Table II
Comparison of age, weight, height and gender, between the two groups
| Parameter | Group P | Group E | P-value |
|---|---|---|---|
| Age [years] | 36.6 ±10.8 | 39.2 ±12.3 | 0.63 |
| Weight [kg] | 52.7 ±10.6 | 54.5 ±8.8 | 0.61 |
| Height [cm] | 157.6 ±7.8 | 157.3 ±6.1 | 0.3 |
| Gender (female) | 6 | 9 | 0.70 |
Table III
Comparison of total opioid (fentanyl) consumption between the two groups intra- and post-operatively, in micrograms and microgram/kilogram body weight
Discussion
Post-sternotomy pain is severe and is known to be a factor which precludes breathing movements, and effective cough thereby contributing to adverse postoperative pulmonary outcomes. Various options available to treat post-sternotomy pain are opioids, nonsteroidal anti-inflammatory drugs, neuraxial analgesia and thoracic wall blocks. Conventional perioperative pain management strategies use opioids and nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs may cause haemorrhagic complications, renal failure, and bleeding, whereas opiates can cause nausea, vomiting, oversedation, ileus, and respiratory depression [9]. The use of TEA in cardiac surgery remains controversial because of the theoretical risk of epidural hematoma, but this risk has not been substantiated [10]. Thoracic wall blocks such as pecto-intercostal fascial block, transversus thoracis muscle plane block, paravertebral block and the thoracic ESPB have gained popularity since they do not have complications associated with a TEA and have comparable analgesia. Studies have shown the benefit of incorporating regional analgesia as a part of multimodal analgesia in cardiac surgery [3, 4]. Still, there is sparse evidence demonstrating the superiority of one regional anaesthesia technique over another. So, we have compared two different thoracic wall blocks for adequate and effective analgesia in cardiac surgeries through sternotomy incision. For the ease of administration, the PIFB seemed more convenient since it could be administered soon after the skin closure without having to turn the patient lateral, which is particularly cumbersome in patients with multiple leads, and an intercostal drain attached. Our study recorded the opioid (fentanyl) consumption intraoperatively and postoperatively up to 24 h after cardiac surgery, pain at rest, pain with deep breathing, time to rescue analgesia and total rescue analgesia demanded during the 24 h.
The ESPB is being used extensively in thoracic and abdominal surgeries, and chronic pain conditions of the chest wall with promising results. The proposed mechanism of action for erector spinae plane block is blockade of the dorsal and ventral rami of the thoracic spinal nerves, the local anaesthetic deposited is seen to spread both cranially and caudally to cover multiple dermatomal levels [11, 12]. ESPB is relatively superficial and easy to place, carrying a lower risk of significant complications such as dural puncture and pneumothorax, given the paucity of important structures near the injection site and clear ultrasonographic landmarks [13]. In a prospective, randomised control trial by Nagaraja et al. of 50 patients comparing continuous catheter TEAs with ESPBs for cardiac surgeries requiring sternotomy, patients who received ESPBs reported improved pain scores at rest and during coughing for up to 48 h postoperatively [14]. In a study by Krishna et al., 106 adult patients undergoing elective cardiac surgery with CPB reported significantly lower pain scores up to 12 h post-extubation than patients receiving ESPB [15]. Macaire et al. compared a historical group of 20 consecutive open cardiac surgery patients matched with a prospective group of 47 consecutive patients receiving continuous bilateral ESPB after general anaesthesia induction. The control group received intravenous (IV) morphine, 0.5 mg/h, and IV nefopam, 100 mg/24 h. Times to chest tube removal, first mobilization, pain (Visual Analogue Scale) values 2 h after chest tube removal, pain values at rest 1 month after surgery, and postoperative adverse events were significantly decreased in the ESPB group [16]. In our study of 2 patients, VAS was more than four at 2 h, three at 6 h, two at 12 h, and three at 24 h in the ESPB group. A randomised controlled trial by Dogan Bakı et al., using a parasternal block with chest drain site infiltration in 90 patients undergoing CABG, showed a significant decrease in tramadol consumption compared with the control group [17]. In a randomised, double-blind study of adult cardiac patients undergoing sternotomy, patients receiving parasternal blocks consumed less morphine in the initial 4 h after surgery. They were better oxygenated at time of extubation, suggesting that this block may facilitate early extubation [18].
The pectoral-intercostal fascial plane block (PIFB) is a relatively newer thoracic wall block, first described for breast surgeries in 2014. Chaudhary et al. randomised 30 paediatric patients undergoing cardiac surgery into two groups: one group was given ropivacaine and another saline in the parasternal intercostal space, between the pectoralis major and intercostal muscles. They found that time to extubation was significantly lower in patients who were administered the parasternal blocks with ropivacaine than in the control group; the mean values were 2.66 h and 5.31 h, respectively (p < 0.001). The pain scores were lower in the ropivacaine group compared with the saline group; mean values were 2.20 for the ropivacaine group and 4.83 for the saline group on a scale of 10. The cumulative fentanyl dose requirement over 24 h was higher in the saline group than in the ropivacaine group (p < 0.001) [19]. Also, in a prospective RCT of 40 patients, Kumar et al. [20] found PIFB to be an easy and efficient technique to reduce postoperative pain after cardiac surgery. In our study VAS of four or less in the PIFB group at 0 h, 2 h and was more than 4 in 3–6 h, one at 12 h and one at 24 h.
In our study, fentanyl consumption in the ESPB group was 8.0 μg/kg in the first 24 h after performing the block, slightly higher than in the PIFB group at 7.11 μg/kg. Three patients in the ESPB group and seven out of 15 patients in the PIFB group did not require rescue analgesia. However, this difference was not significant statistically. Based on the findings, it is reasonable to believe that the duration and quality of analgesia between the PIFB and ESPB are comparable. Hence, it may be prudent to consider PIFB in patients undergoing cardiac surgeries through the mid-sternotomy incision, for its ease of administration and positioning.
Limitation: Cardiac surgeries requiring mid-sternotomy comprise numerous indications, such as valve replacements, vascular repair, and CABGs. The hemodynamic fluctuations are hence seemingly variable in different patients. Hence pain assessment tools may often become difficult in hemodynamically unstable patients. Owing to the varied spectrum of surgeries, the pain assessment may not be applicable universally to all patients and remains a limitation. Hence relatively a lesser sample size and lack of subgroup analysis is the limitation of our study.
Conclusions
Regional anaesthesia techniques as a part of multimodal analgesia are known to provide superior pain control and reduce opioid consumption. Both PIFB and ESPB showed good analgesia and decreased opioid requirement in patients undergoing cardiac surgeries through a mid-sternotomy incision. However, there was an insignificant difference between pain scores, time to rescue analgesia and total opioid consumption between the patients receiving PIFB and ESPB.