Introduction
The history of mediastinal tumours dates back to ancient times when they were first described by the Greek physician Hippocrates in the 5th century BC. Over the course of history, the diagnosis and treatment of mediastinal tumours have undergone significant advancements. In the 19th century, the development of thoracic surgery and the utilization of anaesthesia enabled the surgical removal of certain mediastinal tumours. In the mid-20th century, the advent of radiological imaging techniques such as X-ray and computed tomography (CT) scan greatly enhanced the ability to diagnose and stage mediastinal tumours. In the late 20th and early 21st centuries, remarkable progress was made in treating mediastinal tumours, with the introduction of minimally invasive approaches like video-assisted thoracoscopic surgery (VATS), robotic surgery, as well as the utilization of chemotherapy and radiation therapy. Today, the management of mediastinal tumours involves a multidisciplinary approach that includes radiologists, thoracic surgeons, medical oncologists, and radiation oncologists. Deeper insights into the nature of these tumours and the increasing implementation of the aforementioned techniques have resulted in improved patient outcomes, including higher survival rates and an improved quality of life.
Anatomical definitions
Before the mid-19th century, surgeons viewed opening the chest as a potentially fatal procedure due to adverse physiological effects. Dieffenbach introduced the admonition phrase “stop at the pleura” to express this belief [1]. Consequently, the realm of surgical exploration in the mediastinal space remained largely uncharted for many years. Prior to advancements in anaesthetic techniques, surgical interventions within the thoracic cavity were primarily limited to tube thoracostomy for cases involving tuberculosis or empyema [2]. The first comprehensive study on mediastinal diseases was conducted by Hare in 1888 [2], encompassing 520 cases primarily consisting of malignant tumours. Additionally, Riegel [3], Bennett [4], Eger [5], and Steven [6] also authored monographs on the subject of intrathoracic and mediastinal tumours.
Common aetiologies of an anterior mediastinal mass comprise thymoma, teratoma, thyroid disease, and lymphoma. Congenital cysts, such as foregut and pericardial cysts, predominantly manifest as masses in the middle mediastinum, whereas neurogenic tumours frequently arise in the posterior mediastinum [7, 8]. However, the mediastinum is also a frequent site for secondary tumours and manifestations of various systemic diseases [8]. Bauer and Stoffregen were able to identify more than 90 types of mediastinal tumours, and several classification systems have been proposed [9].
Thymomas comprise the majority of mediastinal tumours, followed by neurogenic tumours and benign cysts, collectively accounting for 60% of mediastinal masses [7]. Numerous classification systems have been suggested for the mediastinum, with the oldest description from Gray’s Anatomy textbook being the most commonly used. Shield’s 3-zone classification scheme is also frequently applied in clinical practice. Other traditional models include Fraser and Pare [10], Felson [11], Heitzman [12], and Whitten [13]. These models generally rely on radiographic landmarks of the mediastinum. However, in 2014, the International Thymic Malignancy Interest Group (ITMG) and the Japanese Association for Research of the Thymus (JART) proposed that mediastinal divisions should primarily be based on CT scans and operative findings to facilitate differential diagnosis and treatment strategies [14].
Diagnostic tools
The diagnosis of mediastinal lesions has always presented a multidisciplinary challenge. Before the advancements in medical imaging, the differential diagnosis of intrathoracic diseases relied primarily on clinical findings. Interestingly, the first reported case of a dermoid cyst in the mediastinum was documented by Gordon in 1823 [8]. In his report, he acknowledged that the case was initially misinterpreted as pneumonia and later as an aneurysm of the innominate artery. However, the introduction of X-ray scans in 1900 revolutionized the diagnostic approach to mediastinal diseases. Plain chest X-ray and fluoroscopic examinations of the thorax became the initial imaging modalities employed in the evaluation of intrathoracic neoplasms [14].
The initial attempts to improve radiographic imaging commenced in 1896 with the application of various elements possessing high atomic numbers, although some of them were highly toxic. The accidental discovery of iodine in 1920 facilitated the development of numerous radiocontrast agents. Danelius documented the utilization of abrodil in the mediastinal space; however, it resulted in incomplete radiographic enhancement and complications such as mediastinal fibrosis [15].
In 1936, Professor Condorelli from the University of Bari published a series of articles on artificial pneumomediastinum in conjunction with X-ray scans [16]. This method was employed to assess the location of mediastinal tumours and their anatomical relationship to adjacent structures. In cases involving cystic tumours accompanied by pleural effusion, the introduction of air into the cystic cavity followed by X-ray examination was utilized to enhance the radiographic image [17]. Prior to the introduction of the anterior mediastinotomy technique described by Chamberlain in 1966, several other minimally invasive techniques were employed to obtain extrathoracic tissue for the diagnosis of mediastinal diseases [18].
The first invasive diagnostic approach was described by Daniels in 1949, who proposed the biopsy of non-palpable scalene lymph nodes as a means of diagnosing intrathoracic disorders [19]. However, the results were not consistently indicative of disease resectability. Other techniques utilized for the evaluation of mediastinal tumours included cervicomediastinal exploration [20], cervical mediastinotomy [21], mediastinoscopy, and biopsy, as well as various methods of aspiration and needle biopsy.
The application of tumour markers as a diagnostic tool for mediastinal tumours originated in 1973 when Braunstein reported a series of patients with non-germ cell tumours exhibiting elevated beta human chorionic gonadotropin (HCG) levels [22]. In 1977, Scardino et al. found a correlation between A fetoprotein (AFP) levels and germ cell tumours [23]. Notably, specific genetic polymorphisms have been identified in thymoma cases associated with myasthenia gravis, which have proven to be highly valuable in recognizing the clinical and serological aspects of the disease, as well as guiding treatment strategies [24].
Surgical approaches
The inaugural surgical intervention targeting a mediastinal tumour took place in 1888, performed by Nassiloff [25]. This pioneering procedure, devoid of ventilatory support, involved a posterior extrapleural oesophagectomy for suspected malignancy. Subsequently, in the late 19th century, the field of surgical therapy for mediastinal tumours witnessed notable advancements. In 1893, Bastianelli became the first to successfully excise an anterior mediastinal dermoid cyst, employing a suprasternal incision coupled with manubrial resection [26]. Similarly, in 1896, Ludwig Rehn in Frankfurt adopted a transcervical approach for the management of an anterior mediastinal mass [27]. In 1897, Milton, a principal medical officer at Casar Al Aini Hospital in Cairo and a proponent of median sternotomy, presented experimental evidence in vivo, demonstrating that artificial respiratory support facilitated successful exploration of the mediastinum and led to uncomplicated recovery in an animal model [28]. Moreover, he described the extrapleural resection of mediastinal lymph nodes in a human patient afflicted with tuberculosis [28].
Mediastinal surgery experienced significant advancements during the mid-20th century, paralleling the progress made in anaesthetic techniques for airway management and mechanical respiratory support. Prior to this era, performing thoracotomy on a patient who relied solely on spontaneous breathing posed substantial challenges for both the surgeon and the anaesthesiologist [7, 29]. Circulatory compromise and lung collapse, leading to interregional shifts of alveolar air, presented notable difficulties during the procedure. This phenomenon, known as pendelluft, was thoroughly studied and elucidated through a mechanical model proposed by Otis in 1956 [29].
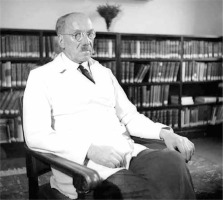
In 1904, renowned thoracic surgeon Ernst Ferdinand Sauerbruch (Figure 1) introduced a ground-breaking concept in thoracic surgery [30]. Shortly thereafter, the pneumonologist Ludolph Brauer also proposed a similar idea involving the use of a pressure-differential chamber to maintain normal respiratory function during surgical interventions within the thoracic region [31]. These methods, however, had limited clinical application, primarily serving as indications for lung infection surgeries. Unfortunately, both Sauerbruch’s negative pressure chamber and Brauer’s positive pressure chamber failed to prevent contamination of the healthy lung by the diseased one. The breakthrough came with the introduction of positive pressure ventilation through endotracheal intubation and the subsequent development of neuromuscular blockade by Harold Griffith in 1942 [32]. These advancements revolutionized the field of mediastinal surgery, enabling safer and more efficient procedures.
In 1940, George Heuer conducted a comprehensive review of over 150 cases involving mediastinal masses that had occurred during the 1920s and 1930s [33]. Most of these cases were comprised of neurogenic tumours and thymomas. Based on his analysis, Heuer proposed 3 distinct surgical approaches: anterior mediastinotomy, posterior thoracotomy, and extended posterolateral thoracotomy [33]. Notably, he did not make any reference to the utilization of median sternotomy in his recommendations.
The concept of thoracoscopy was initially introduced by Jacobeus in 1910 as a treatment method for pleural adhesions in tuberculosis cases [34]. However, it took several years of advancements and refinement for thoracoscopy to gain recognition as an established alternative approach to conventional surgery for benign mediastinal tumours and thymomas.
Thymus surgery
The first recorded case of symptomatic hypertrophy of the thymus gland was documented by Swiss physician Phelix Platter in 1614 [35]. Platter observed a case involving a 5-month-old infant who succumbed to respiratory failure. Intriguingly, Platter noted that 2 brothers had previously died under similar circumstances. Subsequent autopsy findings revealed compression of the trachea and cervical blood vessels caused by an enlarged thymus [35].
The connection between myasthenia and thymus hypertrophy came to light in 1889 when German neurologist Hermann Oppenheim published a report detailing the autopsy of a 40-year-old woman [36]. The autopsy revealed thymus hypertrophy alongside myocardial atrophy, highlighting the association between these 2 conditions. This marked a significant step in understanding the relationship between myasthenia and thymic pathology [35]. Further advancements in this field were made in 1901 when Carl Weigerl, Professor of Pathology in Frankfurt, observed thymus hyperplasia during the autopsy of a young man with myasthenia who had died due to respiratory failure [37]. This observation led Weigerl to propose a potential association between myasthenia gravis and thymic pathology [37].
In 1911, Sauerbruch performed a transcervical approach to remove a 49-g thymus gland from a young woman diagnosed with myasthenia gravis, hyperthyroidism, and radiographic evidence of thymus hyperplasia [30]. Subsequently, in 1930, he conducted a thoracotomy to excise a malignant thymoma. While the first patient experienced symptom relief from myasthenia, both patients ultimately succumbed to mediastinal infections [35].
The ground-breaking discovery made by Oppenheim in 1889 served as a catalyst for Alfred Blalock (Figure 2) to perform the first successful transsternal total thymectomy in 1936 [38]. Blalock carried out the procedure on a 19-year-old girl with cystic thymoma and myasthenia gravis, who had experienced relapses despite preoperative radiation and Prostigmine administration. The patient underwent a smooth recovery and achieved long-term remission from the disease [38]. Building upon this success, Blalock presented a series of 20 patients in 1944 who exhibited prolonged clinical benefit after thymectomy, despite the absence of apparent thymus pathology [39]. Consequently, Blalock concluded that thymectomy could be considered a standard treatment for cases of myasthenia gravis with a short duration of symptoms [39].
Subsequent reports by Keynes (1946), Harvey (1948), and Viets (1950) supported these findings, corroborating the positive outcomes of thymectomy in myasthenia gravis patients [40, 41]. However, Eaton and Clagett challenged these results in 1950, citing potential selection bias in the studies [42]. Later on, their argument was retracted due to inaccuracies in their data analysis [42]. In 1982, Douglas Gracey proposed a less invasive approach to thymectomy, involving the resection of the manubrium instead of sternotomy. In 1987, Papatestas published pertinent data from a large series of thymomas treated with transcervical thymectomy, a technique based on blunt dissection of the anterior mediastinum [43]. Although this technique was initially reported by Ludwig Rehn in 1896 as an approach to anterior mediastinal masses, it had limitations in achieving complete thymoma resection compared to median sternotomy. The advent of thoracoscopic thymectomy in 1993, as first reported by Sugarbaker [44] and a Belgian group [45], marked a significant milestone in the development of minimally invasive approaches for thymic disease. Subsequently, robotic surgery emerged, with the first description of robotic thymectomy by Ashton et al. in 2003 [46].
The diversity in structure and cytology of thymomas has sparked considerable debate among various classification systems regarding their prognostic value. In 1962, Bernartz divided thymomas into 4 categories based on microscopic tumour characteristics [47], while in 1985, Marino and Muller-Hermelink (MMH) proposed a pathology-based classification [48]. However, neither system offered efficient contributions to prognosis. In 1981, the Masaoka classification system was developed, integrating preoperative and histopathological tumour characteristics. Since its inception, this classification system has gained widespread adoption in clinical practice due to its favourable predictive value [49].
Bronchogenic cysts
Bronchogenic cysts have become a more frequent finding following the establishment of thoracotomy as a common surgical procedure. The first successful excision of a bronchogenic cyst was accomplished by Maier in 1948, who subsequently proposed a topographical classification system for bronchogenic cysts that remains widely used today [50]. The earliest reported case of a bronchogenic cyst was documented by Blackater and Evans in 1911, involving a 9-month-old patient who died due to tracheal compression [7]. Meyer also reported a case of a mediastinal cyst with bronchial communication in 1859 [2].
Mediastinal dermoid cysts are rare and often present with unusual clinical manifestations associated with complications. As a result, the differential diagnosis of chronic haemoptysis rarely considers the possibility of a dermoid cyst. An illustrative example is the case of a Chinese woman, operated on by Eloesser in 1933, who had spent 2 years in a sanatorium due to recurrent haemoptysis attributed to a presumed small tuberculous focus at the hilum. The diagnosis was suspected after her husband observed occasional hair expectoration in her sputum [51].
In 1928, Kerr and Warfield reported 138 cases of mediastinal dermoid cysts in the literature, although some may not have been pure intrathoracic dermoids [52]. In 1944, Lloyd Rusby conducted an extensive review of dermoid cysts and mediastinal teratomas, encompassing relevant literature published between 1827 and 1939. The review identified 245 confirmed cases, and the author added 6 more cases to the compilation. It appears that the first resection of a mediastinal dermoid cyst was performed by Senn in 1905 [52].
Other mediastinal tumours
Mediastinal germ cell tumours were first described 50 years ago and were initially considered as secondary manifestations of gonadal malignancies. In 1986, Mullen and Richardson proposed a classification system for mediastinal germ cell tumours, categorizing them into benign germ cell tumours, seminomas, and nonseminomatous germ cell tumours, which are also referred to as malignant teratomas [53]. The most common type among them, teratoma, was first defined by Willis in 1935 as a true tumour composed of multiple tissues foreign to the part in which the tumour is found. The frequent association of mediastinal germ cell tumours with Kleinfelter’s syndrome provided initial evidence of an increased coincidence between mediastinal germ cell tumours and other rare diseases [53].
Intrathoracic benign lipomas are extremely rare, characterized by slow growth and the potential to attain significant size. The first reported case of a giant lipoma occupying the entire hemithorax was documented by Heuer and Andrus in a comprehensive review in 1933 [54]. They also identified 3 anatomical types of intrathoracic lipomas: hour-glass tumours, in which part of the tumour lies within the thorax and the remaining portion penetrates the intercostal structures to present subcutaneously; superior mediastinal lipomas located at the root of the neck; and entirely intrathoracic lipomas [54]. For the latter type, Walker suggested in 1936 that exploratory needle aspiration could aid in the differential diagnosis of such tumours.
The first reported case of mediastinal haemangioma dates back to 1914, as documented by Shannon. Haemangiomas in the mediastinum are rare, and they may be associated with Rendu-Osler syndrome [55].
The surgical removal of mediastinal parathyroid adenoma was first performed by Churchill and Cope at the General Hospital of Massachusetts in 1932 [56]. The notable patient in this case was a sea captain who had undergone 6 previous surgical interventions for persistent hyperparathyroidism. Due to his concerns, the patient extensively studied the available literature at that time and insisted that his doctors consider the possibility of an intrathoracic location for the tumour [56].
In 1908, Weber reported a tumour described as mediastinal lymphadenoma [57]. Twenty years ago, mediastinal lymphomas were designated as primary mediastinal B-cell lymphomas [58]. These tumours, derived from B-cells in the thymus, constitute approximately 5% of all non-Hodgkin lymphomas (NHL) and exhibit specific molecular characteristics. Recent gene expression profiling studies have confirmed certain shared biological characteristics between some B-cell lymphomas and the nodular type of classical Hodgkin lymphoma. Today, these tumours, previously known as anaplastic large cell lymphoma, are categorized as “mediastinal gray zone lymphomas” and are considered very rare [58].
Conclusions
The history of mediastinal tumours represents a remarkable journey of progress and advancements, driven by the continuous evolution of technology and medical knowledge. Over time, these advancements have facilitated earlier and more precise diagnosis, leading to improved treatment strategies. Although managing mediastinal tumours remains a complex and demanding field in medicine, the future appears promising as ongoing research and development endeavours strive to further enhance patient outcomes in the face of these clinical entities. Through dedicated efforts and a multidisciplinary approach, the medical community is poised to provide even greater advancements and solutions for individuals affected by mediastinal tumours.