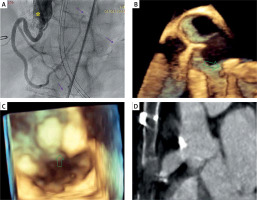
An 81-year-old female patient with a previous history of surgical ligation of a right coronary to right atrium fistula, in her forties, was found unconscious at home. She was transferred directly to our catheterization laboratory after resuscitation for an ECG which suggested inferior ST-elevation myocardial infarction (STEMI). Apart from the previously mentioned intervention, she was suffering from mild arterial hypertension and dyslipidemia and had no history of coronary artery disease. She was not taking any antiplatelet therapy. Upon parametric monitoring, the patient presented sinus rhythm and normal pressure wave but neurological status could not be assessed (as mechanical ventilation through oro-tracheal intubation had already been started). Coronary angiography revealed distal embolic occlusion of two right posterolateral branches and the right posterior descending artery (violet arrows in Figure 1 A), which we considered to be in need of medical therapy (continuous infusion of unfractionated heparin and double platelet inhibition with ticagrelor and aspirin). The right coronary artery angiogram also showed marked elongation and fusiform dilatation of the right coronary sinus (RCS) at the level of prior fistula ligation, with evidence of on site minus image, indicating thrombosis (asterisk in Figure 1 A). Transesophageal 3D echocardiography through long and short axis views (Figures 1 B, C) confirmed the abnormal RCS remodeling with two eccentric para-ostial calcifications (green arrows) as detected also in the multi-projection reconstruction (MPR) CT-scan images (Figure 1 D). The patient ultimately died due to neurological complications (prolonged cerebral hypoxia) 15 days after admission.
Figure 1
A – Right coronary angiography showing right coronary artery (RCA) originating from the fundus of a fusiform, pouch-like right coronary sinus (RCS), possibly the site of fistula ligation (asterisk); note the presence of nonhomogeneous material inside the sinus, and the embolic occlusion of two right postero-lateral (RPL) branches and of the right posterior descending (RPD) artery (violet arrows). B – 3D long axis TE imaging confirming dilated RCS and the presence of two nodules on the roof of the right sinus of Valsalva (green arrow). C – 3D short axis TE view magnification of the nodular structures (green arrow) and inflow of the fusiform pouch. D – multi-projection-reconstruction (MPR) CT scan view showing the calcified origin and the anatomy of the pouch-like RCS
Coronary artery fistula (CAF) is a very rare disease, with an incidence of 0.2–0.6% in the literature [1]. The small number of post-closure follow-up evaluations (surgical or percutaneous) has led to a poor understanding of resulting outcomes [2]. CAF draining to the coronary sinus, advanced age at diagnosis, smoking, diabetes, hypertension, and hyperlipidemia have all been proposed as predictors of an adverse result [3].
This case illustrates a very late (over 40 years) post-surgical closure complication of a CAF presenting as acute coronary syndrome (inferior-STEMI). The occurrence of such a thromboembolic event after CAF ligation is reported in the literature, but it usually takes place in the perioperative period. Complications after further time have been reported, but they are even rarer than the disease itself [4].
Integrated multimodality analysis of the present case reveals the anatomical complexity of this rare disorder. A differential diagnosis with other possible causes of coronary embolization (such as atrial fibrillation, mitral stenosis, endocarditis, left ventricle aneurysm) should always be performed. A sequential combined approach (angiography, transesophageal echocardiography and CT scan) is recommendable. This report suggests the need for further future research into this topic, particularly in long-term clinical follow-up and pharmacological management.








