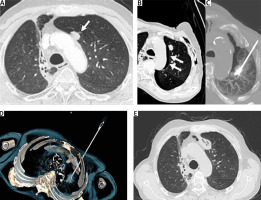
A male patient in his early 60s with lung adenocarcinoma was treated successfully with immunotherapy (durvalumab) and radiotherapy. In the 24-month follow-up computed tomography (CT) scan, the patient developed a single biopsy-proven metastasis in the contralateral lung abutting the mediastinum (Figure 1 A) and was admitted to our hospital for further management. The case was discussed in our local medical multidisciplinary team with the decision of loco-regional treatment of the single lung metastasis with thermal ablation. Artificial pneumothorax was created using a 22-G puncture needle to separate the lesion from the mediastinal structures (Figure 1 B). The metastatic lesion was separated and microwave ablation was performed successfully (Figures 1 C–E).
Figure 1
A – Preoperative computed tomography (CT). Metastatic lung lesion in the left upper lobe (arrow) abutting the mediastinum close to the aortic arch. Radiotherapy changes in the right upper lobe. B – Small iatrogenic pneumothorax (arrows) to separate the metastatic lung lesion from the mediastinal structures. C – Microwave ablation of the left upper lobe metastatic lesion. Intraprocedural axial CT image with maximum intensity projection reconstruction demonstrates the correct probe position. D – 3D reconstruction of the probe position within the metastatic lesion. E – Postprocedural CT shows the ablation zone of the left metastatic lesion
Surgical resection is the established treatment in oligometastatic disease, especially for lung lesions contiguous with the mediastinum [1, 2]. However, complete surgical metastasectomy is not always feasible, leading to the use of less invasive alternative therapeutic options such as radiotherapy and imaging-guided thermal ablation. While radiotherapy is an option for the treatment of lung metastasis, it cannot be safely delivered in central metastatic lesions abutting the mediastinum [3]. Image-guided percutaneous thermal lung ablation has been widely used for the treatment of pulmonary oligometastatic disease [4]. However, thermal ablation of paramediastinal lesions remains challenging and of high risk. Iguchi et al. found that the primary technical effectiveness of thermal ablation was only 43% at the 6-month follow-up scan for the treatment of lung tumors contiguous to the mediastinal structures [5]. The use of artificial pneumothorax has been shown to be effective prior to the thermal ablation for lesions contiguous with the mediastinum, improving the outcome and technical success of the procedure [6]. Similarly, artificial pneumothorax has also been used successfully to exclude chest wall invasion and in the ablative treatment of peripheral lung lesions to reduce procedural and post-procedural pain [7, 8]. In these complex cases of oligometastatic disease, medical multidisciplinary team discussion is always necessary to guide individualized management of pulmonary metastasis in view of the challenging location of the lesion.






