Recurrent respiratory papillomatosis (RRP) is a chronic and unpredictable disease, characterized by varying severity of symptoms and variable periods of remission [1–3]. Due to the lack of effective methods of treating the underlying disease, treatment is mainly based on surgery and adjuvant therapy. For this reason, patients with RRP are exposed to all kinds of complications of repeated surgical treatment in the respiratory tract, including formation of scars and adhesions in this area [1–3].
A 26-year-old patient was admitted urgently to the Department of Thoracic Surgery in Poznan due to left-sided back and chest pain, significant weakness and shortness of breath at rest. Laboratory tests showed significantly increased values of inflammatory indicators (CRP 348 mg/l, PCT 3.45 ng/ml), as well as significant leukocytosis. There was a history of recurrent papillomatosis of the respiratory tract – a condition after repeated resections of papillomas of the larynx and trachea and widening of the subglottic tracheal stenosis. Additionally, from 2021, esophageal dysphagia and recurrent esophageal strictures occurred.
At the time of admission, the patient’s general condition was average and she reported severe chest pain and an increasing feeling of shortness of breath. Chest X-ray was performed in posterior-anterior (PA) projection and left lateral projections: an extensive area of retrohilar infiltrates was noted in the left lung, as well as fluid in the left pleural cavity. A computed tomography (CT) scan of the chest with contrast revealed the presence of fluid in both pleural cavities, with an increased layer of fluid on the left side; additionally, in the left lung, infiltrative lesions in basal segments VIII-X, in the right lung, infiltrative-atelectatic lesions in segments IX, X and IV, as well as enlarged mediastinal lymph nodes. The CT scan after oral administration of contrast revealed dilatation of the esophagus at the level of the upper thoracic opening, below the dilatation, narrowing of the esophageal lumen with no visible contrast in the lumen, then dilation again. At the level of stenosis, infiltrative changes are visible near the esophagus.
A series of bacteriological tests were conducted, including blood, urine, and bronchial wash cultures. The results revealed the presence of Staphylococcus hominis in the blood and Haemophilus influenzae in the bronchial fluid, identified through multiplex PCR. Additionally, cultures performed under aerobic and anaerobic conditions did not show the presence of fungi. Due to the features of left-sided pneumonia with fluid reaction, broad-spectrum empirical antibiotic therapy was used – ceftriaxone, vancomycin, metronidazole, linezolid – and analgesic (metamizole, morphine) and antiemetic (ondansetron) treatment was implemented. Clinical and radiological improvement was achieved, mechanical dilatation of the subglottic part of the trachea was performed, and approximately 3 weeks after admission to the hospital, the patient was discharged home in good general condition.
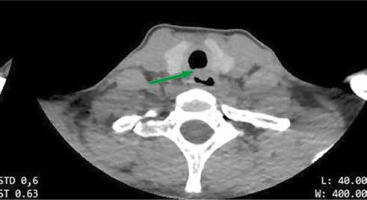
Due to frequent surgical interventions in the respiratory tract, patients with recurrent respiratory papillomatosis are particularly exposed to side effects and complications of numerous operations and procedures in this area [2, 3]. In the case of the patient described here, complications include subglottic tracheal stenosis, as well as recurrent esophageal strictures and esophageal dysphagia. Computed tomography examinations performed in 2021 and 2023 revealed infiltrative scarring lesions around the esophagus and trachea, whose height corresponds to the level of the tracheostomy undergone in childhood (Figure 1). The changes from 2021 are progressive; they highlight the posterior wall of the trachea, narrowing its lumen and modeling the esophagus. Due to the recurrent nature of esophageal strictures and their occurrence at different heights, recurrent esophageal spasms of unknown etiology (functional or scarring) were suspected. Periodically occurring esophageal dysphagia predisposes the patient to episodes of choking on food and food getting stuck in the esophagus, which is a significant risk factor for the development of aspiration pneumonia (Figure 1) [4].
Figure 1
Computed tomography scan of the neck and chest from February 2023 – thickening of the posterior tracheal wall; the lesion is remodeling the lumen of the esophagus
Due to the fact that patients with RRP often show symptoms of shortness of breath, weakness and auscultatory changes even during periods of remission, diagnosis of respiratory tract inflammation may be difficult [5, 6]. After bronchoscopy, the present patient often experienced respiratory edema, dysphonia and cough. Additionally, probably due to a tracheostomy performed in childhood, papillomas spread to the lungs – detected in 2007 in a computed tomography examination. In 2021, a chest CT scan described numerous small cysts and cavities, as well as nodular changes in the lung parenchyma, especially on the right side. This translates into numerous auscultatory changes: muting, periodic humming and whistling, as well as audible stridor [5, 6]. Therefore, monitoring this type of patient in a primary care setting may be somewhat difficult and usually requires close cooperation with the patient’s hospital physician. It should be noted that patients with RRP may experience recurrences of aspiration pneumonia, as well as community-acquired and nosocomial pneumonia [4–6]. It may be necessary to develop standards of practice to monitor this type of patient, for example by regularly performing lung ultrasound on an outpatient basis and analyzing any changes in the obtained images in comparison with the clinical picture. It seems to be an interesting alternative to X-ray and CT examinations, which are often performed in patients with papillomatosis during hospitalization.
People with RRP are a group of patients whose disease course may be either mild or aggressive, with a varying number of complications or side effects of previously used treatments. Treatment requires, above all, a multidisciplinary approach, taking into account the chronicity, individuality and unpredictability of the disease, as well as the need to take care of the patients’ quality of life. It is important to continue searching for effective forms of treatment for respiratory papillomatosis that will not involve so many (although necessary and often life-saving) procedures in the respiratory tract.






