Introduction
Basal cell carcinoma (BCC) stands as the most prevalent form of cancer observed in humans. Conversely, rosacea represents a common chronic inflammatory skin disorder with an unidentified aetiology that affects diverse populations [1]. Both conditions are influenced by significant risk factors such as fair skin phototype, commonly found in the Caucasian population, and exposure to ultraviolet (UV) radiation [1–3]. Additionally, both BCC and rosacea tend to manifest primarily in the central area of the face, particularly the nose [1–4]. However, rosacea primarily affects young women, typically presenting after the age of 30, while BCC is more commonly seen in elderly males, typically in their seventh or eighth decade of life [3, 5]. It is widely acknowledged that UV radiation can exacerbate rosacea, and prolonged exposure to UV radiation is the most prevalent risk factor for the development of BCC [3, 6].
Previous investigations into the association between BCC and rosacea have predominantly focused on rhinophyma. Extensive analyses of BCC cases involving rhinophyma were published in 2012, and since then, only a limited number of case studies have been presented [2, 7]. Consequently, the connection between rosacea and carcinoma remains ambiguous. The motivation for this study is rooted in our own observations and experience within dermatosurgery, where a significant number of patients have presented with both BCC and concomitant rosacea.
Material and methods
This prospective study was conducted from January 2020 to December 2021 at the Dermatosurgery Unit in a single centre. The study population consisted of patients treated surgically for suspected BCC on the face. Screening was performed to identify the presence of concomitant rosacea in these patients. An experienced dermatologist assessed the presence or absence of rosacea, determined the phenotype of rosacea according to the 2017 update by the National Rosacea Society Expert Committee [5], and evaluated its intensity using the Investigator’s Global Assessment (IGA) [8]. After histological confirmation of BCC, the following data were recorded for each lesion: patient age, patient sex, tumour morphology, and exact location. A total of 110 patients were included in the study.
Statistical analysis
To examine the differences between categorical variables, the c2 test was used. Differences between groups were determined using the Mann-Whitney U-test as analysed variables were of abnormal distribution. The Spearman’s rank correlation analysis was used to assess the strength relation between two different variables. Results with p-values less than 0.05 were treated as statistically significant. The statistical analysis was performed using Statistica 13.3 software (TIBCO Software Inc., Palo Alto, CA, U.S.).
Results
A total of 110 patients were included in the analysis, comprising 68 (61.8%) women and 42 (38.2%) men. The age of the patients ranged from 40 to 90 years, with a mean age of 70.1 ±12.2 years. All patients had Fitzpatrick skin type II. The excised tumours were clinically categorized as follows: nodular BCC in 98 subjects (89%), ulcerative in 10 (9.1%) subjects, superficial subtype in 1 (0.95%) subject, and pigmented BCC in 1 (0.95%) subject. Among the study group, 51 (46.4%) subjects were clinically diagnosed with concomitant rosacea. Detailed characteristics of BCC, including the subtype and IGA of rosacea in the study group, are presented in Table 1. No significant differences were observed in terms of sex, age, tumour location, or morphological subtype between patients with and without concomitant rosacea (detailed data not shown).
Table 1
Comparison between women and men with concomitant rosacea and basal cell carcinoma
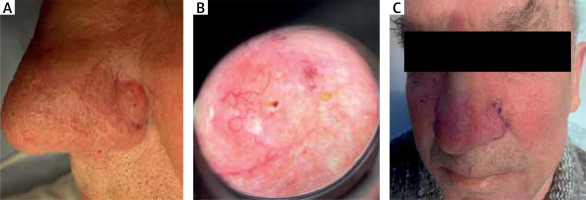
In our study group, 35.5% of women had BCC located on the cheeks, while in men, the majority of cancers were located on the nose (55%, n = 11) (Figure 1). However, this difference did not reach statistical significance (p > 0.05).
Discussion
Although in common knowledge rosacea is still known as a disease of young and middled-aged white women (30–50 years), there are not many epidemiological studies reporting prevalence of rosacea in different age groups, races and between sexes [9]. Recent wide analysis from Germany [10], which included 161,269 patients, reported the largest prevalence of rosacea which increased significantly with age with the largest prevalence in the sixth decade of life. However, in the article cited, above only 5.7% of studied older population (60–70 years) had concomitant rosacea (2.1% in general population, 2.2% of Fitzpatrick II). Unfortunately, patients were not screened for skin cancer in this study. The incidence of rosacea in our population was doubtlessly higher, comparing to the aforementioned normative population (46.4% vs. 5.7%).
Li et al. [11] performed a comprehensive analysis of 75,088 white women in the US and studied the association between personal history of rosacea and risk of cancers during a follow-up of 20 years. A personal history of rosacea was significantly associated with an increased risk of incident BCC only (HR = 1.50, 95% CI: 1.35–1.67), but not for melanoma or squamous cell carcinoma. The researchers suggested that possible association between UV exposure at early ages might confer an elevated risk of BCC. According to the nationwide cohort study of the Danish population [12], a higher incidence of non-melanoma skin cancer (NMSC) was also reported in patients with rosacea. Talghini et al. [13] have not found any association between Demodex folliculorum infestation and basal cell carcinoma. Li et al. [14] have explored the role of tetracycline treatment (common systemic drug for rosacea) and risk of BCC based on 213,536 participants from the Nurses’ Health Study (NHS), NHS2, and Health Professionals Follow-up Study. Tetracycline use was associated with a modestly increased risk of BCC (the study group comprised of 36,377 cases), with a pooled hazard ratio (HR) of 1.11 (95% confidence interval (CI): 1.02–1.21, p-trend= 0.05 by duration of use).
Higher incidence of rosacea in our group should be taken with caution as most of the studies regarding potential association of BCC and rosacea are based on national registries and compromise of the treated cases, while in our group, during the admission to the hospital a trained dermatologist assessed the skin of the patients. Most of our patients have not been treated for rosacea before. However, due to the fact that both rosacea and BCC share the same risk factors – UV exposure, the potential association should not be neglected. According to recent studies, BCC may cause also itching of the skin [15], a symptom which was previously linked mostly to inflammatory skin conditions, such as rosacea [16]. What is worth noticing, most of the BCC in men in our group were located on the nose, which is also a typical location of rhinophyma. In women, most cases were located on the cheeks, which is also a typical location of rosacea.
Haber et al. [17] conducted an analysis regarding comorbidities in patients with rosacea. They found a relationship between the occurrence of rosacea and higher incidence of migraines, which is not surprising considering that vascular abnormalities are part of the pathogenesis of both conditions, and triggers such as stress and alcohol may contribute to the onset of both migraines and rosacea. Egeberg et al. [12] also observed increased activation and expression of matrix metalloproteinases (MMPs) in skin areas affected by rosacea, as well as in other conditions such as Parkinson’s disease, Alzheimer’s disease, and gliomas, which could explain the increased risk of glioma in patients with rosacea.
Chronic inflammation in rosacea may have a systemic impact, and therefore, rosacea has been linked to cardiovascular disease risk factors. Interestingly, recent studies have shown a reduced risk of vascular events in patients with coexisting rosacea who were treated with tetracycline. Additionally, gastrointestinal disorders such as celiac disease and irritable bowel disease occur more frequently in patients with rosacea. Li et al. [11] observed an increased frequency of thyroid cancer and BCC among patients with rosacea, although the pathogenesis is not fully understood and may be related to increased exposure to ultraviolet radiation, as mentioned earlier.
Additionally, there has been an observed increase in vitamin D levels in rosacea, which may be a result of UV exposure, and may play a role in the immune activation in rosacea. Moreover, vitamin D is produced to a lesser extent in pigmented skin, which is considered less susceptible to rosacea. Active smoking appears to reduce the risk of rosacea, although the mechanism is unknown, and vasoconstriction may be involved.
Comorbidities of rosacea share common innate and adaptive inflammatory elements with rosacea, such as increased activity of macrophages and macrophage-derived mediators, ROS, keratinocytes, mast cells, fibroblasts, neutrophils, B cells, Th1 and Th17 cells, vascular endothelium, matrix metalloproteinases, IL-1β, tumor necrosis factor, and increased levels of C-reactive protein [18].
Therefore, during our research, we have raised the suspicion that perhaps it is not just rosacea itself but the inflammatory state that increases the risk of carcinogenesis and BCC. However, personal experience as well as literature show that inflammation, especially induced by cryosurgery, electrodessication and wound healing after resection, has an anti-cancer effect and could remove remaining BCC cells. The use of immunomodulating substances such as imiquimod, especially in combination with cryosurgery, has also shown positive effects [19–21].
On the other hand, studies have shown a preventive effect on skin squamous photocarcinogenesis when nonsteroidal anti-inflammatory drugs (NSAIDs) were used. Tang et al. [22] also observed a similar effect with oral celecoxib (a COX2-specific inhibitor) treatment as chemoprevention, inhibiting BCC carcinogenesis in genetically predisposed PTCH1+/- humans and mice [22].
This illustrates the varied and uncertain pathogenesis of the co-occurrence of BCC and rosacea, thus their relationship requires further research.
This study has several limitations: firstly, it was a single-centre study, and the population included was a relatively small group. Prospective studies including a larger number of subjects and analysing factors such as: sun exposure and drugs, are in need. Regardless of that, we suggest that elderly subjects with rosacea should be screened for the presence of concomitant BCC. We acknowledge also that our study has limitations as it focused on patients predominantly with Fitzpatrick skin type II, which is the prevailing demographic in our region.