Introduction
In many centers, laparoscopic appendectomy has become the preferred surgical approach in children with appendicitis [1]. Surgical stress is a condition that triggers inflammatory responses. Studies have shown that laparoscopy triggers the inflammatory response less than the open procedure [2]. Comparisons of the inflammatory response after laparoscopy and laparotomy have been reported in adults, but few studies have compared the immune response between laparoscopy and laparotomy in children [3]. While some surgeons have argued that laparoscopic appendectomy creates less surgical trauma than open appendectomy, others have claimed that laparoscopic appendectomy is not different in terms of postoperative surgical stress. The difference between open and laparoscopic appendectomy in terms of postoperative surgical stress is therefore still a controversial issue. Inflammatory markers such as interleukins (IL) 1 (IL-1), 6 (IL-6), and 8 (IL-8) are secreted from the body in response to surgical stress [4].
Soluble urokinase plasminogen activator receptor (suPAR) is the soluble form of the membrane-bound receptor urokinase plasminogen activator receptor (uPAR) that is found in blood and other body fluids. It is involved in proliferation, adhesion, migration, angiogenesis, and in the inflammatory response. Release of suPAR is increased upon an inflammatory stimulus. Blood suPAR level reflects an individual’s level of inflammation and immune activation. It is positively correlated with inflammatory biomarkers such as C-reactive protein (CRP), IL-6, and tumor necrosis factor-α (TNF-α) [5]. Similarly to interleukins, it reflects the level of activity of the immune system in response to an inflammatory stimulus [6]. Proteases such as chymotrypsin and phospholipase, which are increased as a result of inflammation, cause the release of uPAR into the circulation and the formation of the soluble form of suPAR.
Aim
In this study, we aimed to compare open and laparoscopic appendectomies regarding suPAR for the evaluation of the inflammatory response. In line with this, we hypothesized that the inflammatory response would be milder and the increase in serum suPAR levels would be smaller for laparoscopic appendectomy.
Material and methods
Study population and perioperative care
This prospective randomized clinical trial was approved by the Local Ethics Committee (Istanbul University, Istanbul Faculty of Medicine Clinical Research Ethics Committee-2015/1810). After obtaining informed consent from their legal guardians, patients between 3 and 17 years of age who were admitted to the pediatric surgery department and scheduled for appendectomy due to acute appendicitis were enrolled in the study. Patients with perforated appendicitis, cardiovascular and pulmonary disease, previous history of abdominal surgery, allergies, and those who used anti-inflammatory drugs and antibiotics before presentation were excluded.
All patients fasted for 8 h before the operation. Cefazolin sodium 100 mg/kg was administered to all patients before anesthesia as an intravenous prophylactic antibiotic.
The operations were performed under general anesthesia. A transversus abdominis plane block was applied before the surgical incision. All patients were given 15 mg/kg paracetamol IV before surgical closure as a standard procedure. As a part of multimodal analgesia, paracetamol administration at a dose of 15 mg/kg was continued every 6 h after the operation. Acute pain was assessed by the service nurse intermittently for 24 h by using FLACC (0: relaxed and comfortable, 10: severe discomfort/pain) scores. If the patient’s FLACC scores were > 3/10 despite this routine treatment, 1 mg/kg IV tramadol was given and recorded as a rescue analgesic.
Interventions and surgical technique
The patients were randomized to receive either laparoscopic or conventional open appendectomy based on a computer-generated random list before enrollment by a researcher not involved in the surgery (https://www.graphpad. com/quick calls/randMenu/). The list was placed and sealed in sequentially numbered envelopes. The envelopes were opened by the surgeon who performed the appendectomy on the day of the operation.
In conventional open appendectomies, a McBurney incision was used. The stump was ligated twice. Laparoscopic appendectomy was performed with the standard 3 ports. The appendix stump was closed with an Endoloop suture (Endoloop Ligature, Ethicon Endo-Surgery, Somerville, NJ, USA). A 10 mm trocar was used to remove the specimen from the abdomen. Reactionary fluids were aspirated, and controlled irrigation and aspiration were performed. None of the patients had a drain placed.
Outcome measures
The primary outcome was a change in preoperative and postoperative suPAR levels. The secondary outcomes were white blood cell (WBC) count, lymphocytes, neutrophils, platelets, CRP level, appendix diameter, symptoms and symptom duration, surgical complications, percentage of patients who received rescue analgesics, hospital stay, and family satisfaction.
Collection of serum samples and analysis
For the measurement of suPAR levels, 2 ml venous blood samples were taken from the patients just before the operation and 12 h after the surgery. The blood samples were transported in dry test tubes and immediately centrifuged at 3000 rpm for 10 min. The serum part was aspirated and stored at –80°C refrigerators until the suPAR levels were analyzed. The suPAR levels were measured by the enzyme-linked immunosorbent assay (ELISA) method (BT-Lab, China). The difference between the groups was evaluated statistically.
Statistical analysis
Sample size analysis: Assuming higher levels in open surgery compared to laparoscopic techniques and based on a prediction of an approximate 15% increase in suPAR (3.7 ng/ml to 4.2 ng/ml), 19 patients per group were calculated when the a was 0.5 with a power of 90% (G*Power 3.1). Considering a possible 5% drop-out, a minimum of 40 patients were planned to be enrolled in the study.
The SPSS 22 program was used in the analysis of the data collected within the scope of the research (SPSS, Chicago, IL, USA). Shapiro-Wilk test values were examined to determine the conformity of the data with a normal distribution. Parametric analyses were used for data with a normal distribution, and nonparametric analyses were used for data without a normal distribution. The independent samples t test and Mann-Whitney U test were used to compare quantitative (numerical) data between the groups, while χ2 analysis was used to compare qualitative (categorical) data between the groups. The Wilcoxon test was used to compare suPAR measurements of the groups before and after the operation. The Spearman test, which is a nonparametric test, was used to evaluate the correlation between CPR and suPAR within the group. P-values < 0.05 were considered statistically significant.
Results
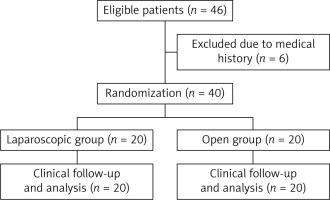
A total of 46 children were enrolled in the study and randomized to the laparoscopic and open groups. Six patients who did not give consent to participate in the study or were found to have perforated appendicitis were excluded from the study. The patients were divided into two groups according to laparoscopic (n = 20) and open appendectomy (n = 20), leaving an equal number of patients in each group (Figure 1).
The mean age of the patients undergoing laparoscopic appendectomy was 10.55 ±2.743 (3–17) years. The mean age of the patients undergoing open appendectomy was 11.40 ±3.515 (3–17) years. No conversion to open surgery was recorded. The demographic findings of the patients are shown in Table I.
Table I
Comparison of demographic characteristics of patients. Data are presented as median (minimum–maximum), mean ± SD, n (%)
Based on Table I, there was no statistically significant difference in age, sex, WBC count, neutrophil proportion, lymphocyte proportion, platelets, CRP, appendix diameter, symptoms, or symptom duration.
Table II shows that there was no significant difference in the preoperative and postoperative suPAR measurements in the laparoscopic group (p = 0.14), but there was a significant increase from the preoperative to the postoperative suPAR measurements in the open group (p = 0.04).
Table II
Comparison of suPAR measurements between the groups before and after the operation. Data are expressed as the median (minimum–maximum). *P ≤ 0.05 was considered significant
In the intergroup comparison, a 5.7% difference was found in the preoperative values in laparoscopic and open operations. When the preoperative suPAR values between the two groups were compared, no statistically significant difference was found (p = 0.82). A change of 11.5.7% was found in the postoperative values in laparoscopic and open operations. When the postoperative suPAR values between the two groups were compared, a statistically significant difference was found (p = 0.048).
As shown in Table III, the operation time in the laparoscopic group was significantly shorter than that in the open group (p = 0.004). The hospital stay in the laparoscopic group was also significantly shorter than that in the open group (p = 0.047). The number of patients receiving rescue analgesics and parent satisfaction were similar between the groups (p = 0.4, p = 0.3).
Table III
Comparison of operative time and length of hospital stay between the two groups. Data are presented as median (minimum–maximum), mean ± SD, n (%). *P ≤ 0.05 was considered significant
In the laparoscopic appendectomy group, one patient had a port-side infection, and 2 patients in the open appendectomy group had wound infection.
Discussion
Many authors have suggested that laparoscopic appendectomy creates less surgical stress than open appendectomy, thus causing less postoperative pain and a rapid recovery. In our study, we found that laparoscopic appendectomy produces less postoperative surgical stress than open appendectomy using suPAR measurements, which is a new biomarker that provides information about both inflammatory cells and the level of proteases formed during inflammation [6, 7].
In many centers, laparoscopic appendectomy has become the preferred approach for appendectomy in pediatric patients in the last decade. Since it is a minimally invasive technique, it has gained popularity in a short time due to its association with decreased hospital stay, early recovery, less wound infection, and good cosmetic results. Mulita et al. demonstrated the advantages of laparoscopic appendectomy, such as short hospital stay and early return to activity, in a large study with 1809 appendectomy patients [8].
Due to its less traumatic nature, it may be associated with reduced surgical stress, but this remains a debated issue. Various authors have investigated a spectrum of markers, such as CPR, IL-6, and IL-8, to evaluate the inflammatory response of laparoscopic appendectomy over open appendectomy [9, 10]. In the present study, we investigated the effects of laparoscopic appendectomy on the stress inflammatory response compared with open appendectomy regarding a new biomarker of systemic inflammation.
Soluble urokinase plasminogen activator receptor (suPAR) was first described in the 1990s as a biomarker of cancer progression and infectious diseases. Since then, suPAR has been studied in different diseases for clinical, diagnostic, and prognostic purposes as an indicator of inflammation [11]. suPAR is the soluble form of the urokinase-type plasminogen activator receptor (uPAR), which is a glycosyl-phosphatidylinositol-linked membrane protein. In its membrane-bound form, uPAR is found in a variety of cells, including monocytes, activated T-lymphocytes, endothelial cells, keratinocytes, macrophages, smooth muscle cells, fibroblasts, and megakaryocytes, and the soluble form results from the release of membrane-bound uPAR. suPAR is detected in different concentrations in the plasma, urine, blood, serum, and cerebrospinal fluid according to the degree of activation of the immune system [12]. Akın et al. reported that suPAR is a biomarker that can be used successfully in the diagnosis and determination of the degree of appendicitis [6]. Therefore, we planned to use suPAR to compare the immune response between patients undergoing open and laparoscopic appendectomies, as it very accurately reveals immune system activation and has not been evaluated before.
Various studies have focused on the difference in the inflammatory response between patients undergoing open appendicitis and laparoscopic appendectomy. Almagor et al. [13] studied preoperative and postoperative IL-6 in patients with acute appendicitis and found no significant difference between the open and laparoscopic groups. Additionally, Simon et al. compared 20 patients in the open and laparoscopic groups in terms of inflammatory parameters (TNF-α, sTNF-R, IL-1Ra, s IL-2R, IL-8) [2]. Both groups of authors found no inflammatory difference between the two groups and reported that the laparoscopic group was discharged more easily. We believe that suPAR is a more sensitive marker compared to previous ones in distinguishing surgical stress in open and laparoscopic procedures. We feel that this marker is essential to prove the superiority of laparoscopic appendectomy. Other markers in the past have produced mixed results.
The inflammatory response and its consequences have been challenging for surgeons in the last decade. Some authors claim that elevated intra-abdominal pressure during laparoscopy may promote a systemic inflammatory response. Previously, Serour et al. reported postlaparoscopy appendectomy complications (PLAC), which are observed in uneventfully discharged children who have had laparoscopic appendectomies and are characterized by lower quadrant pain, subfebrile temperature, leukocytosis, and abdominal ultrasonography findings [14]. In their next study, they reported that the cytokines sP-selectin, MCP-1, and sVCAM-1 may play a role in possible postappendectomy cytokine activation after laparoscopic appendicitis, and this phenomenon is more evident after laparoscopic appendectomy than after open appendectomy [15]. They found that cytokine values did not differ significantly according to the surgical approach. As they stated, more studies are needed to investigate the inflammatory response after laparoscopic appendectomy. Inflammatory comparison of laparoscopic appendectomy and open appendectomy in children is also important for PLAC evaluation. We conducted this study and believe suPAR to be one of the most valuable biomarkers in determining this difference.
Li et al. published one of the largest series with 160 children that compared open and laparoscopic appendectomies regarding the inflammatory response [16]. They monitored IL-6 and CPR levels before surgery and 12 h after surgery to evaluate the magnitude of surgical trauma and observed that the increase (preoperative vs. postoperative) in IL-6 and CPR in the laparoscopic group was remarkably lower than that in the open group. They concluded that laparoscopic appendectomy was safe and efficient, creating fewer postoperative complications, with shorter operating time and less surgical trauma. Similarly, Schietroma et al. performed 147 appendectomies, compared the acute phase response and immunologic status from the laparoscopic and open approaches, and found that open appendectomy was associated with a higher level of systemic inflammation compared with laparoscopic appendectomy [17]. Similarly to their results, we found a significant increase in the suPAR levels from the preoperative to postoperative samples. We believe that suPAR is an effective biomarker in demonstrating the inflammatory change between open and laparoscopic appendectomy.
Previously, the duration of laparoscopic appendectomy was found to be longer than that of open appendectomy [18, 19]. However, as in our study, more recent investigations have reported that laparoscopic appendectomy can be performed in a shorter time than open appendectomy. This is because the learning curve of laparoscopic appendectomy has flattened. At the same time, the length of hospital stay was significantly shorter in the laparoscopic group.
In our study, we observed that, although not statistically significant, in children who were operated on laparoscopically there was less need for postoperative rescue and analgesia and higher parental satisfaction.
The main limitation of our study is the limited number of patients in each group in terms of the evaluation of surgical complications. Second, other inflammatory markers, such as IL-1 and IL-6, could be examined at the same time to determine their correlation with suPAR.
Conclusions
Surgical intervention causes trauma in the body and triggers the systemic inflammatory response. Laparoscopic appendectomy is associated with a shorter operative time and a shorter hospital stay, as well as less of an inflammatory response caused by surgical stress than open appendectomy. suPAR is an effective marker for comparing postoperative inflammatory stress between open and closed appendectomies.