Unexpected life-threatening airway emergencies mandating an emergent surgical intervention, whilst rare, represent one of the most urgent decision-making scenarios in medicine [1]. When faced with respiratory instability, the primary focus is to secure the airway definitively, typically by inserting a cuffed endotracheal tube. Failure to establish a patent airway promptly can lead to severe consequences such as hypoxic brain injury or death within minutes. In adults, airway obstruction is commonly due to inflammation, infection and trauma [2, 3]. Amongst the common causes of difficulty in airway management are airway obstruction by a foreign body or tumor, angioedema, massive facial or neck trauma, burns and abnormal anatomy. The worst cases of airway compromise may end up in a life-threatening “can’t intubate, can’t oxygenate or ventilate” (CICOV) situation in which clinicians struggle to provide adequate mask ventilation or successfully intubate the trachea despite using different methods such as direct and video-assisted laryngoscopy or fiber-optic bronchoscopy. When attempts with supra-glottic airway devices prove unsuccessful, a surgical airway is indicated [4, 5].
The American Society of Anesthesiologists’ difficult airway algorithm identifies two acceptable emergency surgical definitive airways in the CICOV scenario: cricothyrotomy (CTM) and tracheostomy [5]. The Difficult Airway Society (DAS) defines both as acceptable emergency “front of neck access” (FONA) [4]. Both organizations emphasize the need for the procedure to be done as rapidly as possible and by an experienced practitioner [4, 5]. Little has been published regarding the optimal method of emergency surgical airway practices [3].
CTM is an incision made through the skin and cricothyroid membrane. Tracheostomy is performed at a lower position typically between the 2nd and 4th tracheal ring (Figure 1). Unlike CTM, which is performed only in emergency settings, tracheostomy is also performed by skilled operators in elective settings, either using an open surgical approach or a minimally invasive, needle-guided percutaneous dilatation Seldinger technique (PDT) (Figure 2).
FIGURE 1
Relevant neck anatomy. The anatomic sites of cricothyrotomy (CTM) and percutaneous dilatational tracheostomy are presented in this figure. CTM shown in arrow 6 is an incision made through the skin and cricothyroid membrane to establish a patent airway. Tracheostomy shown in arrow 7 is performed at a lower position of the neck at the level of the trachea (typically between the 2nd and 4th tracheal rings). In this figure a tracheostomy is shown at its site. The figure is adapted from Wikipedia
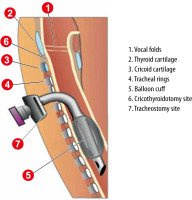
FIGURE 2
Portex Blue Line Ultra PDT kit. This PDT kit is most widely used in the author’s institution for percutaneous dilatational tracheostomy procedures. The figure was adapted from the Smith Medical ASD, Inc. Minneapolis, MN, USA website

CTM is considered easier and quicker to perform than tracheotomy, requires less manipulation of the cervical spine, is more superficial and is anatomically further from the thyroid gland and major blood vessels. It is thus thought to be associated with fewer complications, such as bleeding and surgical site infection [6]. Therefore, it is suggested as the first-line surgical method by both the DAS and ASA protocols [4, 5]. Moreover, CTM is only intended to be a temporizing measure until a long-term definitive airway can be established. Its utilization exposes the patient with a proven difficult airway to a subsequent airway manipulation. Revision is routinely performed after CTM, whilst being rarely required after PDT.
However, since the need to establish an emergency surgical airway is both unexpected and rare, there is a lack of high-quality evidence comparing the use of CTM and PDT in this setting. Therefore, we retrospectively analyzed 33 cases that occurred over a sixteen-year period in a tertiary care center where emergency surgical airways were established after less invasive airway solutions failed. In all these cases of life-threatening actual or impending CICOV, a decision was made to proceed with front of the neck surgical access.
METHODS
This retrospective observational study was performed with approval from the Helsinki Committee of the Hadassah Medical Organization (Reference number HMO-0258-22). The requirement for informed consent was waived due to the retrospective nature of the study.
Patients
All patients aged > 18 years admitted between October 2007 and September 2022 to the Hadassah – Hebrew University Medical Center, Jerusalem, Israel, a tertiary-care center, who underwent emergency surgical airway intervention, namely tracheostomy or CTM, were identified.
Emergency scenario management
In accordance with the policies and procedures of the medical center, in the event of a life-threatening airway emergency, whether in an in-patient department, Emergency Department (ED) or Intensive Care Unit (ICU) an emergency team is activated. This team includes a critical care physician and is fully equipped to treat a variety of emergency scenarios, including difficult airways.
Inclusion criteria
A life-threatening airway emergency was defined as a situation where attempts to manage the airway using tracheal intubation, facemask ventilation, and supra-glottic airway device failed. This included cases with CICOV situations [4, 5, 7]. Another subset of patients included in the study was “impending CICOV”; namely patients with an imminent threat to airway patency in whom temporizing measures (either face mask, or supra-glottic airway) provided some degree of oxygenation or ventilation, but intubation was deemed to be necessary, but impossible.
Data collection
For maximal identification of target cases, screening for CICOV was performed using three methods. Initially, the institutional electronic medical record system (EMR) was searched for documented surgical airway cases, specifically those with ICD-9 codes: 31.1, 31.74, 519.02, 519.09, V44.0, V55.0. Special attention was given to the ICU and ED cases, since a significant proportion of airway emergencies are known to occur in these locations. Subsequently, data from the automated “code blue” documentation system was examined and, finally, the hospital trauma registry was examined. To validate the integrity of the number of intubations reported we compared these numbers to the amount of intubation consumables (endotracheal tubes) purchased by the institution during the study period, to provide a rough denominator.
Cases from all three data sources where there were documented airway emergencies with overt or impending CICOV scenarios were analyzed to determine whether an emergency surgical airway intervention was reported. If an emergency surgical airway intervention was reported the case was included in this study. Charts were reviewed to obtain a comprehensive medical history. The history included information regarding the patient’s background, medical status, medications, indication for admission and acute airway management. Data on post-surgical airway immediate and late neurological and respiratory outcomes as well as survival to discharge were also collected.
Statistical analysis
Descriptive statistics including frequencies and percentages are presented. Owing to the small sample size and probable skewing from the normal distribution, non-parametric statistical tests (Kruskal-Wallis rank sum test) were used to examine the differences between the patients with CTM and PDT.
RESULTS
Characteristics of patients with defined CICOV
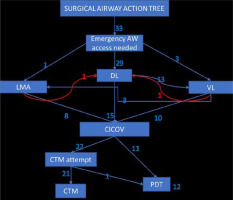
During the 16-year study period approximately 14,112 endotracheal and other airway intubations were performed outside the operating rooms in our institution. Forty-seven of the intubation events included surgical airway procedures of various types. Only 33 fulfilled the study inclusion criteria for an overt or pending CICOV that resulted in the establishment of a surgical airway. In these cases, either PDT or CTM (12 and 21 cases respectively) was performed (Figure 3).
FIGURE 3
Airway management techniques utilized in all of the analyzed cases. The surgical airway management action tree is presented in this figure. In most (29) of the 33 cases of unexpected airway difficulty later on necessitating surgical AW intervention, the operators initially tried DL and only then tried other AW modalities. In 1 case of a VL attempt and 1 case of an LMA attempt the operator decided to go back and try DL before declaring CICOV. After declaring CICOV, out of 22 CTM attempts, 1failed and a PDT was then attempted successfully; all of the PDT attempts were initially successful. Glossary: AW – airway, DL – direct laryngoscopy, VL – video laryngoscopy, LMA – laryngeal mask airway, CICOV – can’t intubate, can’t oxygenate/ventilate, PDT – percutaneous dilatational tracheostomy, CTM – cricothyrotomy
The demographics, medical background, circumstances, and indications for acute surgical airway management of the CICOV patients are summarized in Tables 1, 2 and 3.
TABLE 1
Characteristics of patients requiring emergency surgical airway
TABLE 2
Characteristics, cause and management of cases requiring percutaneous dilatation tracheostomy (PDT)
TABLE 3
Characteristics, cause and management of cases requiring cricothyrotomy (CTM)
CTM patients were younger than PDT patients; median (range) ages were 44 (20–88) years and 62 (27–82) years, respectively (Figure 4A). There was a male gender predominance in both groups, which was more pronounced in the CTM group (66.6% vs. 58.3%). The median SOFA scores before the procedure were similar between the PDT and CTM groups, 5 (0–7) vs. 5 (1–11) respectively, median (range), P = 0.5 – Kruskal-Wallis rank sum test (Figure 4B).
FIGURE 4
Whisker plot of age and SOFA (Severity of Organ Failure Assessment) scores. The whisker plots of age and SOFA scores are represented in plots A and B. A) Whisker plot of age. The orange line is the median; the box represents the range of the data, IQR 25–75%. B) Whiskers plot of the SOFA scores; the orange line is the median, the box represents the range of the data, IQR 25–75%

Procedures
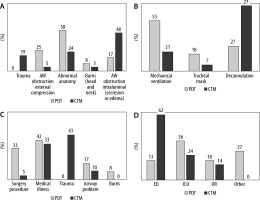
In six patients the surgical airway procedure was required while cardio-pulmonary resuscitation was being performed. Thirteen CTMs and two PDTs were performed as part of the primary trauma survey in the ED. The causes of non-surgical airway failure are detailed in Figure 5A. Overall, the most common indication for surgical airway placement (39% of the surgical interventions) was intraluminal airway obstruction (secretion or edema), followed by abnormal anatomy (33%), and airway obstruction (12%). Among the latter 4 cases, an expanding neck hematoma was the cause of airway compromise in 2 PDT and one CTM patients. Most CTM procedures were performed in trauma patients in the ED, while most PDT procedures were performed among patients with diagnoses other than trauma, either in the ICU or in patients rushed to the operating room (Figures 5C and 5D).
FIGURE 5
Descriptive data of the procedures and outcomes. A) Causes of the failure of the nonsurgical AW (airway) management categorized by the lesion limiting the feasibility of the laryngoscopy (either direct or video assisted) and tracheal intubation. The data available were insufficient to evaluate mechanical causes of the failure. B) Longterm airway outcomes of surviving patients: mechanical ventilation – long term chronic ventilation, tracheal mask – use of a tracheal mask after liberation from mechanical ventilation without decannulation, and decannulation – formal decannulation of the trachea. C) Indications for hospital admission were grouped into the following categories: admission for an elective or emergent surgical or other procedure; admission for an acute medical illness; admission for blunt or penetrating trauma; admission for an acute airway problem, e.g. upper airway edema, burns involving the head and the neck. D) Location of the procedure: ED – emergency department, OR – operating rooms, and other any location in the hospital. Data are displayed as percentages of the total number of patients in graphs A–C; data in graph D are percentages of patients surviving more than 30 days. PDT – percutaneous dilatational tracheostomy, CTM – cricothyrotomy
Successful insertion of an emergency surgical airway occurred in all patients. Two of the CTMs were performed by the acute care surgery team, two by critical care specialists or residents, three by anesthetists or anesthesia residents and twelve by ear, nose and throat (ENT) surgeons. Most of the CTM operators were residents. One CTM case failed and was converted to PDT and in an additional case an ENT surgeon performed a CTM and a decision was made to convert to PDT immediately due to inadequate oxygenation. All PDT procedures were successful and conducted by experienced practitioners (critical care medicine and anesthesia consultants with previous experience of at least 60 such procedures). Overall, 12 PDT and 19 of 23 of the CTM attempts were initially successful. No perioperative complications were reported in the PDT group, while in CTM group two initial false tracts with a successful second attempt (i.e. re-do) and three bleeding events were reported. The duration of PDT performance was reported as short, only a few minutes (3.5 minutes on average in a large series in our hospital – personal communication), as opposed to the variable duration in the CTM group, depending on the experience of the operator.
Airway management
Direct laryngoscopy (DL) was attempted and failed in the majority of the patients in both groups, PDT 11/12 and CTM 18/21. The reasons for failure and for no DL attempt in the other patients are detailed in Supplemental Digital Content Tables 1 and 2. In two CTM cases, DL was initially successful, but reintubation failed (in both cases the indication for reintubation was a tear in the endotracheal tube (ETT) cuff.
Video laryngoscopy (VL) with a hyper-angulated blade was attempted in 8/12 PDT and in 9/21 CTM patients (Table 1). In 6/8 of PDT cases VL failed to visualize the larynx. In another case it was impossible to exchange an ETT with a ruptured balloon and in the other it was impossible to advance the tube into the trachea despite visualization of the trachea.
Either facemask (FM) ventilation or a supra- glottic airway device, namely a laryngeal mask airway (LMA), was used as a rescue method. This method was attempted in 5/12 of the PDT group patients and proved to be a successful bridge to definitive airway in 3/5 cases. In the CTM group it was attempted in only 4/21 patients and did not provide adequate ventilation in either case. In the PDT group, FM ventilation was adequate in 2 cases and difficult in 1 case. All attempts to achieve airway control are detailed in Figure 1.
Outcome
Twenty-one of the 37 CICOV patients (60.6%) survived to hospital discharge: 7 (58.33%) PDT and 14 (66.66%) CTM cases. Thirty-day-survival occurred in 22 patients: 8 PDT and 14 CTM patients (Figure 6). Of the PDT patients who survived 30 days, one did not survive to hospital discharge. All of the 14 CTM patients who survived the first 24 hours were alive upon hospital discharge.
FIGURE 6
KaplanMeier survival curves for both groups. Due to the low number of patients, the model was used only to present the data in a graphical manner, and statistical significance was not assessed. Of note, the increased early mortality (namely within the first 24 hours) in the CTM group can be attributed both to the severity of the primary injury that may have been augmented by a greater degree of anoxic damage during the primary resuscitation, until a patent airway was established
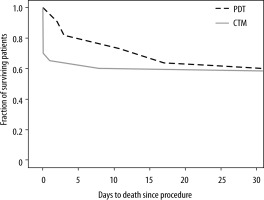
Immediate mortality (within the first 24 hours) was reported in 5 CTM patients. In three immediate mortality cases, the failure to establish a non-surgical airway contributed to the cause of death. In the remaining two cases, the presenting mechanism of injury was the major contributor to failure of resuscitation: severe traumatic brain injury (TBI) and cardiac contusion. Immediate mortality was not observed in the PDT group (Figure 4).
Eventual successful liberation from mechanical ventilation occurred in 6/12 of PDT and 11/21 of CTM patients. Of the 21 CTM cases, all 16 patients who survived the initial CICOV emergency underwent subsequent tracheostomy. De-cannulation of the trachea was done in 4/12 PDT and 10/21 CTM. Favorable immediate neurological outcome according to the Glasgow Coma Scale (GCS ≥ 11T) was observed in 8/12 PDT and 8/21 of CTM patients, 3 PDT remained sedated until death and 7 CTM patients died within the first 72 hours.
DISCUSSION
This retrospective analysis presents 33 cases of life-threatening airway emergencies successfully managed by either percutaneous tracheostomy or CTM. This analysis demonstrates that these emergency procedures are very rare. In the in-hospital setting of a tertiary trauma center with the right equipment and expert staff, PDT was a safe, efficient, and reliable technique for the emergent management of the patient’s airway in a CICOV scenario.
CTM is considered easier and quicker to perform than tracheotomy. Several case series of emergency surgical CTM have reported success rates approaching 100% with complication rates of 5–14%. However, difficulties related to the procedure, including excessive time to secure the airway, are not accurately captured by these retrospective series [7, 8]. Moreover, the identification of the crico-thyroid membrane is frequently difficult, especially in female patients [9]. Our current study revealed similar complication rates and difficulties with CTM.
Tracheostomy is a common procedure. Over the past several decades, the utilization of tracheo-stomy has increased in the world. The proportion of PDT versus surgical tracheostomy is increasing in the population of critical care patients due to PDT’s lower cost and higher availability at the bedside [8]. Additionally, current percutaneous tracheostomy kits are relatively easy and safe to use. PDT as an emergency procedure in airway management has been previously reported: several case reports and short series in different scenarios such as angioedema, severe burns and inhalational injury, distorted airway anatomy secondary to spinal muscular atrophy, complete airway obstruction due to an expanding neck hematoma and a series of four cases where intubation either failed or was considered impossible [10–13]. A retrospective analysis reported 18 patients in whom airway edema, anaphylaxis, or traumatic reasons precluded tracheal intubation [14]. Another study reported 10 trauma patients with failed intubation due to either cranio-facial injury or burns successfully salvaged by emergency PDT [15]. Yet, the majority of the previously published cases did not meet the criteria for impending or overt CICOV, whilst meeting the criteria of failed intubation. In the current retrospective study, all cases were impending or overt CICOV. Therefore, this report describes the efficacy of the PDT procedure specifically during CICOV situations, when performed by practitioners experienced in the technique due to frequent exposure and practice in the intensive care unit.
A recent systematic review analyzed mostly retrospective data comparing tracheostomy and CTM in the emergent setting [13]. This analysis did not differentiate the percutaneous from the surgical approach in the tracheostomy group. The main findings were that the early, minor, and major complications profile was similar between the tracheo-stomy and the CTM groups, while there were more late complications in the tracheostomy group [16]. In our survey all PDT procedures were initially successful, with no peri-operative complications. However, all CTM patients had to undergo a subsequent definitive airway procedure.
In the present study, comparison between the PDT and the CTM patients is limited since patient groups differed in age, underlying diseases, the cause of CICOV, the location where the procedure was done and the operators. However, we found that in cases where the operators were trained in PDT, they preferred to perform a PDT. Furthermore, the current study demonstrates several advantages to performing PDT over CTM: firstly, PDT is performed on a regular basis in the intensive care unit. Therefore, during an emergency the well-trained staff felt safer when performing a familiar procedure (PDT), rather than a simpler yet by far rarer one (CTM). This is the likely reason the PDT outcomes were better in terms of morbidity, immediate mortality, and feasibility, than CTM in general, and also when CTM failed. It could also be that the choice of technique in our study was affected by the urgency of the situation, i.e. impending versus overt CICOV, with CTM being favored in the impending situation.
Secondly, unlike CTM, PDT establishes a long-term definitive airway. CTM provides only a short-term airway solution, since it requires conversion to a more permanent airway solution, usually a surgical tracheostomy. Therefore, we see a possible safety benefit to PDT, as it avoids additional manipulation of a proven difficult airway.
Lastly, during cardio-pulmonary resuscitation (CPR), CTM might require the cessation of resuscitation efforts until the completion of the procedure, as opposed to PDT, which can be performed in a stepwise manner using a modified Seldinger’s technique; this allows the continuation of chest compressions during management of the airway.
This study has several limitations. Firstly, it is retrospective in nature since it focuses on emergency scenarios. Also, it includes small subgroups of patients since the occurrence of CICOV is very rare. Secondly, all PDTs were well recorded by the operators; however, some CTM cases may have been misreported, especially in the ED when CPR was unsuccessful. Lastly, as previously described, the differences between the groups were significant in several aspects: The CTM patients were younger, mostly trauma victims who needed an immediate airway solution provided by the available surgical residents in the ER, while the PDT patients were hospitalized, older, heterogeneous, and mostly dealt with in a “code blue” scenario by senior anesthesia and critical care representatives who were trained in PDT.
CONCLUSIONS
In summary, the findings of this study demonstrate that within the hospital, with the proper equipment and experienced staff, PDT could be a valid and an efficient method of emergency airway management in the overt or pending CICOV scenario. To confirm these observations, a prospective multi-center observational study comparing PDT to CTM is needed.
Many PDTs are performed in a controlled and planned manner every week in a busy ICU, providing good training opportunities for medical staff who may need to perform the procedure in emergency situations in the CICOV setting. CTM is taught in theory and may be practiced on manikins and then only rarely encountered in the “real world” when it may need to be performed in a high-stress environment. Our results encourage the expansion of PDT training in order to increase its accessibility to patients with CICOV, at sites other than the intensive care unit, such as the emergency department. The study findings do not detract from the notion that the operator should use whatever technique he is familiar with when FONA is required in an emergency, CTM, PDT or open/surgical tracheostomy.


