Transvenous lead extraction (TLE) is commonly performed to manage complications in pacemaker and defibrillator leads, including malfunction or infection. While generally considered safe, TLE carries risks of severe complications, such as cardiac tamponade, that demand rapid and well-coordinated response. This case report describes a scenario in which prompt surgical intervention was essential in managing tamponade during TLE, emphasizing the importance of readiness and access to hybrid operating room (OR) facilities when handling high-risk extractions.
A 61-year-old male patient was admitted for elective TLE due to increasing impedance in the right ventricular (RV) lead of his dual-chamber pacemaker. The patient had a history of sick sinus syndrome, diagnosed in 2010 following episodes of severe sinus bradycardia, documented at approximately 30 beats per minute during nighttime Holter monitoring. A dual-chamber pacemaker (Medtronic Relia DDD) was implanted, and his symptoms subsequently improved. In 2022, the pacemaker required an upgrade to a Vitatron due to an end-of-service indication (ERI), although the RV lead continued to show rising impedance.
The patient’s medical background was complex, with comorbidities including hypertension, type 2 diabetes, obesity (body mass index (BMI) 37.97 kg/m2), and bilateral hip osteoarthritis. Although the patient attended regular follow-ups, he did not fully adhere to activity restrictions for his left shoulder, potentially impacting device function. Given the ongoing issues with lead impedance and stimulation thresholds, options were discussed, and the patient ultimately chose TLE over adding a new lead. The TLE was conducted in a hybrid operating room to enable rapid transition to surgery if necessary. The RV lead was removed using an 11 Fr Evolution mechanical rotational sheath, which offers high control during extractions (Figure 1).
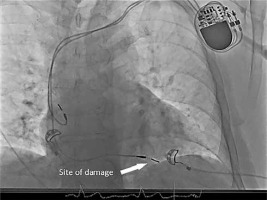
Figure 1
Placement of the electrode in the right ventricle, illustrating the site of perforation during transvenous lead extraction (TLE)
Shortly after removal, transesophageal echocardiography (TEE) detected rapid pericardial effusion, indicative of cardiac tamponade. Recognizing the urgency of the situation, the surgical team performed an emergency sternotomy. Upon opening the pericardium, active hemorrhage from the right ventricular (RV) apex – likely related to the previous lead’s fixation site – was identified and controlled using direct monofilament sutures. From the detection of cardiac tamponade to skin incision, only 5 minutes elapsed, enabling immediate surgical preparation. Following the skin incision, an additional 6 minutes passed before extracorporeal circulation (ECC) was initiated. During this interval, the patient experienced sudden cardiac arrest (SCA), necessitating urgent resuscitation and emergency ECC connection to stabilize his condition.
Postoperatively, the patient was transferred, intubated, to the cardiothoracic intensive care unit (ICU). Although his recovery was complicated by transient delirium and a right upper extremity embolism on postoperative day 7, both issues were effectively managed. The embolic event was treated with embolectomy in vascular surgery, and the patient was discharged in a stable condition on day 11.
These critical interventions were executed in an exceptionally brief timeframe, underscoring the indispensable role of having immediate cardiothoracic surgical support in high-risk TLE procedures. Achieving such an expedited response would be unfeasible in centers lacking on-site cardiac surgery expertise.
This case illustrates the importance of swift decision-making and rapid action in managing complications associated with TLE. Cardiac tamponade, while a rare outcome of TLE (with reported rates of approximately 0.3% in high-volume centers), presents an immediate threat to life that necessitates urgent surgical intervention [1, 2]. The literature highlights that a delay of even minutes in detecting and managing tamponade can drastically worsen patient outcomes, making a swift transition to open surgery a critical factor in survival [3, 4].
Hybrid operating rooms, equipped for both minimally invasive and open surgical procedures, offer a substantial advantage in high-risk cases, allowing a rapid response to unforeseen complications. This setting enables a multidisciplinary approach, with cardiothoracic surgeons and interventional cardiologists prepared to take immediate action. In this case, the 10-minute timeframe from detection of effusion to sternotomy exemplifies the best practices in TLE management. Studies suggest that hybrid ORs, combined with prompt detection using real-time imaging such as TEE, reduce mortality associated with cardiac tamponade during high-risk procedures [5].
Moreover, the presence of TEE as an intraoperative monitoring tool was indispensable in this case. TEE allowed real-time, precise visualization, facilitating early recognition of the tamponade and enabling the surgical team to act without delay. Evidence supports the integration of TEE in high-risk TLE cases, particularly in hybrid OR settings, where immediate intervention can be provided [6].
This case also reinforces the necessity of having robust protocols for high-risk TLE cases. Hybrid OR setups, access to a skilled multidisciplinary team, and adherence to intraoperative monitoring protocols (e.g., TEE) were pivotal to the successful outcome. Given the patient’s positive recovery, the protocol used aligns with current recommendations that emphasize swift action and seamless transition to surgical intervention when complications arise during TLE [7].
This case report underscores the life-saving potential of a rapid response and structured protocols in managing severe complications during TLE. With the growing volume of TLE procedures globally, establishing robust protocols that ensure access to hybrid ORs and a multidisciplinary team ready for emergency intervention is essential. Such protocols not only improve patient safety but also enhance procedural outcomes, particularly in cases with an elevated risk of complications.






