INTRODUCTION
Cataract surgery is one of the most commonly performed operations worldwide, with approximately 20 million procedures performed globally each year [1]. As a result of longer lifespan and the use of devices such as smartphones, tablets or laptops, patients’ demands regarding intermediate and near visual acuity have grown. The new extended depth-of-focus (EDOF) intraocular lens (IOL) technology represents a compromise between monofocal lenses, which provide good distance acuity, and multifocal lenses, which allow patients to see far, intermediate and close distances, but induce more adverse effects such as halo and glare, and have lower contrast sensitivity compared to EDOF IOLs [2, 3]. Patients show an increasing desire to become spectacle independent.
Unlike multifocal lenses, EDOF IOLs generate a single elongated focal point rather than several foci, thus providing patients with clear distance vision, intermediate distance vision and useful close-distance visual acuity.
AcrySof IQ Vivity IOLs (Alcon Inc., USA) belong to the group of non-diffractive, hydrophobic extended depth-of-focus IOLs with an ultraviolet and blue light filter. The optical part of the lens has a diameter of 6 mm, and the combined haptic/optical dimension is 13 mm. The refractive index of the implant is 1.55. It provides patients with good far distance and intermediate vision acuity, as well as relatively good near vision acuity.
MATERIAL AND METHODS
The paper presents a retrospective analysis of subjective and objective clinical parameters in patients before and 3 months after Acrysof IQ Vivity IOL implantation during surgical removal of the patient’s own lens. Surgical procedures and all visits took place at the Laser Clinic in the period from January 1, 2021 to March 31, 2022. The study was conducted in accordance with the principles of the Helsinki Declaration, and the patients gave their written consent to use their medical data in the study.
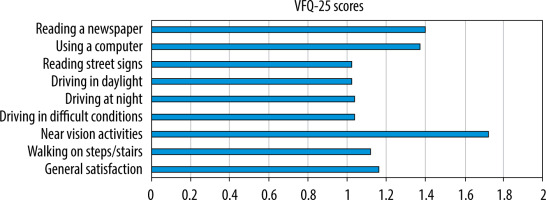
All patients were assessed for uncorrected distance visual acuity and best corrected visual acuity (UDVA, CDVA) for 5 m, uncorrected and corrected intermediate distance visual acuity for 66 cm (UIVA, DCIVA), as well as uncorrected and corrected close distance visual acuity for 30 cm (UNVA, DCNVA) using ETDRS tables (Early Treatment of Diabetic Retinopathy Study), with the results expressed on the logMAR scale, assessing the anterior and posterior segment of the eyeball with a slit lamp, preoperative refraction, spherical equivalent before surgery and 3 months after the surgery. Preoperative biometry was performed with IOL Master 700 (Carl Zeiss Meditec AG, Jena, Germany). The Barrett Universal II method was used for lens power calculation, with target refraction planned for emmetropia. All patients completed the modified VFQ-25 questionnaire. They self-reported difficulties in performing a given activity by using a 5-point scale, where: 1 = no difficulties, 2 = very mild difficulties, 3 = mild difficulties, 4 = moderate difficulties, 5 = serious difficulties. The participants were asked about undesirable dysphotopic phenomena such as halo, glare, starburst and diplopia. They were also asked to report their use of spectacles for far, intermediate and near distances. Spectacle dependent individuals chose 1 out of 4 answers on how often they need glasses for a given daily activity and received percentage scores for their answers:
The score obtained by the patient indicated the degree of spectacle dependence.
The EDOF Alcon Vivity IOL implantation exclusion criteria included total corneal astigmatism > 0.75 D, irregular astigmatism, corneal conditions such as keratoconus, pellucid marginal degeneration, corneal dystrophies, macular conditions, advanced glaucoma, and suspected inability to neuroadapt after the surgery.
Microsoft Excel 365 and Statistica 13 were used for statistical calculations and charts. The Wilcoxon matched-pairs test was used to determine statistical significance.
RESULTS
A total of 45 patients (71 eyes) who had Acrysof Alcon Vivity implanted were included in the study.
Preoperative demographics are presented in Table I.
Table I
Preoperative data
No intra- or postoperative complications were observed in any of the patients.
Mean uncorrected distance visual acuity (UDVA) improved from 0.51 ±0.21 to 0.1 ±0.11 logMAR, while mean corrected distance visual acuity (CDVA) improved from 0.33 ±0.19 to 0.03 ±0.05 logMAR at 3 months after surgery compared to baseline.
The mean uncorrected intermediate visual acuity (UIVA) was –0.02 ±0.04 logMAR, and corrected intermediate visual acuity (DCIVA) was –0.09 ±0.00 logMAR at 3 months after the surgery.
The mean uncorrected near visual acuity (UNVA) was 0.02 ±0.14 and the mean corrected near visual acuity (DCNVA) was –0.01 ±0.00 logMAR at 3 months after the surgery. The mean spherical equivalent was –1.24 ±0.53 D at baseline and –0.42 ±0.37 D at 3 months postoperatively. These values were not statistically significant (p = 0.24).
Figure 1 presents the patients’ responses to the questions contained in the modified VFQ-25 questionnaire (Scale 1-5; where: 1 – no difficulty, and 5 – significant difficulty in performing a given activity).
The questionnaire on difficulties in performing daily activities showed that looking at closely located objects and reading a newspaper without spectacle correction were most problematic for our patients.
Dysphotopsia
Table II shows the number and percentage of eyes implanted with Acrysof Alcon Vivity IOLs with undesirable dysphotopsia symptoms, such as halo, glare, starburst or double vision.
Spectacle independence
The patients were also asked about their spectacle independence status. A total of 100% of patients were completely independent, and needed no glasses for long and intermediate distances. 57% of patients reported that they only sometimes required glasses, e.g. when reading fine print, sewing or performing other precise activities in poor lighting conditions. The mean near add was 0.4 D ±0.52 D.
DISCUSSION
Acrysof IQ Vivity is a relatively new IOL characterized by modern, non-diffractive technology. The choice of this lens and other types of EDOF IOLs is dictated by the patients’ lifestyle [4]. EDOF IOLs ensure very good visual acuity for far distances and intermediate distances and useful visual acuity for close distances. As for the precision when looking at close distances, trifocal lenses are more useful, as they provide better visual acuity at close distances, thus greater spectacle independence, but lower contrast sensitivity and more dysphotopsia [5].
The patient’s personality and mental state are of great importance when choosing the type of lens implanted during cataract surgery. It was shown that individuals with neurotic disorders, who were more prone to anxiety, depressed mood or crying, showed worse subjective outcomes after Premium lens implantation [6]. These patients were more likely to experience halo and glare effects, decreased contrast sensitivity, worse assessment of the distance from a given object or problems with neuroadaptation [6]. It therefore seems advisable to screen candidates for EDOF or other Premium type IOLs for mental disorders using e.g. the FFI questionnaire, which was introduced by Lew Goldberg [7].
Our study showed very good outcomes for far, intermediate and near distance visual acuity; however, some patients needed near vision correction.
The obtained results of visual acuity at 3 months postoperatively are promising. In our analysis, UDVA improved to 0.1 ±0.11 logMAR, as also reported by Arrigo et al. (0.1 ±0.04 logMAR), who however obtained a slightly better CDVA in their patients at 3 months after the procedure (0.0 ±0.03 logMAR) compared to our study group (0.03 ±0.05 logMAR) [4]. Our patients achieved a slightly lower monocular CDVA (0.03 ±0.05 logMAR) compared to the data obtained by Arrigo et al., US FDA and Newsom and associates (0.0 ±0.05 logMAR, 0.016 logMAR and 0.02 ±0.07 logMAR, respectively) [4, 8, 9]. We obtained higher UIVA and UNVA values compared to previous studies [4, 8, 9]. The Vivity IOL ensured better far, intermediate and near distance visual acuity than other EDOF lenses as well as extended depth of focus monofocal lenses [10-12].
Candidates for EDOF Acrysof Alcon Vivity IOL implantation should be aware that they will need minor spectacle correction for precise near-distance activities. In our study, vision correction was not needed in 57% of the eyes, while in other patients this correction was sometimes used to perform precise activities in poor light. Rementeria-Capelo et al. reported 40% independence from near vision spectacle correction, while Kohnen et al. reported 38% spectacle independence among patients [13, 14].
Dysphotopsia was less common in our patients compared to other publications. Halo was reported in 21.1%, glare in 18.3%, and starburst in 0% of patients. Newsom et al. reported halo, glare and starburst phenomena in 45%, 42% and 61% patients, respectively [9], while Kohnen et al. reported halo and glare in 25% of patients [14]. Good outcomes in terms of dysphotopsia are largely related to the modern non-diffractive X-wave technology, as many studies report that more undesirable dysphotopsia was experienced by patients with diffractive lenses. Nowik et al. reported halo and glare phenomena in 40% and 3% of patients with a different model of non-diffractive Mini Well IOL implanted, respectively; worse outcomes were observed in patients with diffractive EDOF Symfony IOLs, with halo and glare occurring in 65.6% and 24% of patients, respectively [15]. It can be assumed that undesirable dysphotopic phenomena would be reduced if patients were asked about their occurrence over a period longer than 3 months. This is the minimum period of neuroadaptation [16].
In our study, patients were asked to complete a modified VFQ-25 questionnaire to report their difficulties in performing daily activities and their general satisfaction with implanted Vivity IOLs. The results showed that patients experienced overall satisfaction and satisfaction with EDOF Alcon Vivity IOL implantation. When asked in the questionnaire, the participants reported that they found reading fine print in poor lighting most problematic. Lubiński et al. reported that patients who had trifocal AtLisa tri 839 MP lenses implanted had fewer difficulties in performing this activity, while more problems with reading small print were reported by patients implanted with diffractive EDOF IOLs (Symphony) [17]. Therefore, candidates for Acrysof Alcon Vivity IOL implantation should be informed preoperatively that they will probably need low power spectacles for more precise close-distance activities.
We are aware that our study has some limitations. First of all, the study group should include at least 100 patients, as in accordance with the recommendations of the American Academy of Ophthalmology [18]. Secondly, the evaluation of halo and glare phenomena was based on the subjective patient responses rather than, for example, using a simulator or under real conditions. Thirdly, a follow-up period longer than 3 months would be needed as this is only the minimum period for neuroadaptation.

 ENGLISH
ENGLISH