Introduction
Groin hernia is one of the most common diseases in general surgery. About 20 million patients undergo groin hernia repair annually worldwide [1]. The risk of groin hernia is reported to be 27% in men and 3% in women in lifetime [2]. Adult patients generally have no possibility of healing without operation, and the only way to achieve recovery is through surgery [3]. Reducing hernia recurrence and postoperative pain is the ultimate goal of hernia repair. Chronic Postoperative Inguinal Pain (CPIP) is defined as pain lasting more than 3 months [4]. The CPIP is one of two main complications in inguinal hernia (IH) repair. Up to 20% of patients undergoing laparoscopic IH repair suffer from CPIP [5, 6], it is associated with impaired productivity and decreased quality of life [7]. Studies have reported it to occur in 6–10% at long-term follow-ups which affected daily activities [8, 9]. Tension-free hernia repair using synthetic non-absorbable mesh is now widely used in clinical practice. Lichtenstein and laparoscopic hernia repair are best evaluated [1]. Laparoscopic transabdominal preperitoneal hernia repair (TAPP) and laparoscopic total extraperitoneal hernia repair (TEP) are both minimally invasive tension-free surgeries. TAPP has become one of routine procedures for IH repair and is recommended by various guidelines [10]. Risk factors for CPIP can be related to factors such as young age, female sex, preoperative pain, and specific genotypes [11–14]. Surgical related risk factors, such as hernia repair, protective measures for nerve, and selection of mesh materials, are also included [15, 16]. The efforts to reduce CPIP risks are crucial. Although laparoscopic IH repair can reduce postoperative pain, the reported postoperative pain varies in different institutions. The reported incidence of CPIP in laparoscopic IH repair is a serious problem. The techniques of dissection, mesh fixation, and mesh material used have been identified as being part of the problem [5]. There may be some relationship between postoperative pain and some intraoperative management by surgeons. Although monopolar instruments such as a monopolar scissor, electric hooks, ultrasound knives achieve the goal of perfect hemostasis in TAPP, they also bring about tissue energy injuries and burns to the organization. It was not found in the relevant reports that the dissection of the preperitoneal space without electrocoagulation (DPSWE) was carried throughout the process in TAPP. This study explored the effectiveness and safety of DPSWE in TAPP mainly by combining the blunt and sharp dissection by the scissors, whether it reduces postoperative pain, and whether it increases the possibility of postoperative bleeding.
Aim
This study aimed to assess the effectiveness and safety of DPSWE in TAPP throughout the whole process.
Material and methods
General data
Retrospective analysis was conducted on the surgical videos and data of 134 patients with laparoscopic transperitoneal inguinal hernia repair (TAPP) at the Shanghai Public Health Clinical Centre from January 2019 to June 2023. According to whether the electrocoagulation is used, it is divided into the electrocoagulation group (EG) and non-electrocoagulation group (NEG). In the EG the repair was mainly carried out using monopolar instruments such as a monopolar scissor, electric hooks, ultrasound knives throughout the process in TAPP, especially in areas such as pain triangle, danger triangle, death coronal, and hernia sac. In the NEG the repair was mainly carried out by DPSWE throughout the entire process. The dissection mainly relied on the open and close blade of scissors. When encountering intraoperative bleeding, arterial bleeding was sutured or clipped to stop bleeding, venous bleeding and capillary bleeding were compressed with pad, and the inguinal region was fixed and compressed postoperatively.
The EG consisted of 49 (36.5%) males and 4 (3.0%) females, with an average age of 55.6 ±16.7 years and a body mass index (BMI) of 25.6 ±4.3 kg/m2, including 17 (12.7%) cases of direct inguinal hernia, 35 (26.2%) cases of indirect inguinal hernia and 1 (0.7%) case of femoral hernia. In the EG, there were 5 (3.7%) cases who smoked for more than 1 year, 6 (4.5%) cases who suffered from diabetes mellitus, 9 (6.7%) cases who suffered from HIV infection, 35 (26.1%) cases whose defect size was less than 3 cm, and 18 (13.4%) cases whose defect size was more than 3 cm.
The NEG consisted of 73 (54.5%) males and 8 (6.0%) females, with an average age of 56.0 ±16.9 years and BMI of 26.4 ±4.1 kg/m2. There were 23 (17.2%) cases of direct inguinal hernia, 56 (41.8%) cases of indirect inguinal hernia and 2 (1.5%) cases of femoral hernia. There was no statistically significant difference in general information between the two groups of patients (p > 0.05). In the NEG, 6 (4.5%) cases had smoked for more than 1 year, 8 (5.9%) cases had diabetes mellitus, 12 (9.0%) cases had HIV infection, 56 (41.8%) cases had defects smaller than 3 cm, and 25 (18.7%) cases had defects larger than 3 cm.
Inclusion criteria: (1) Patients with primary IH; (2) Adult patients aged 19–88.
Exclusion criteria: (1) Patients with systemic diseases such as infectious, autoimmune, and hematological diseases are excluded; (2) Strangulated hernia; (3) Those with a previous history of lower abdominal surgery; (4) Those without contraindications for general anesthesia; (5) Those that have not been adjusted properly with warfarin usage, valvular heart disease, atrial fibrillation, hypertension. Clinical data (p > 0.05) were observed, as shown in Table I.
Table I
The general information between the EG and the NEG
Methods
Standard anatomy of EG
The patients were positioned supine with arms close to the trunk. Under general anesthesia, the patient’s head was placed in a low position and an incision of approximately 12 mm in length was made at the upper edge of the umbilicus. The pressure of pneumoperitoneum was 10 mm Hg (1 mm Hg = 0.133 kPa). Each insertion trocar (5 mm) was placed parallel to the outer edge of the rectus abdominal muscle. The abdominal cavity was explored. The monopolar instruments such as electric hook were dissected in the preperitoneal space, and the energy of the coagulation with a monopolar hook was delivered at 30 W. The dissected point started from the outside of the internal ring. The preperitoneal space was dissected. Electrocoagulation was carried out when encountering bleeding. The distal part of the hernia sac was dissected as much as possible. The peritoneum was held in the left hand and a certain tension was maintained, while the tissue was separated in the right hand with electrocoagulation. The hernia sac of direct hernia and smaller oblique hernia was completely peeled off and returned to the preperitoneal space. Pubic symphysis, cooper ligament and the spermatic cord were fully exposed. The patch (ProGrip Self-Gripping Polyester Mesh, Covidien, Trevoux, PP1509, 15×9 cm, China) was placed on the preperitoneal space to completely cover the myopectineal orifice. The transversalis fascia (TF) was sutured as much as possible and the defect of the hernia was closed when the defect was larger than 3 cm [17]. The peritoneum was sutured with 1-0 absorbable thread (synthetical suture, Johnson & Johnson, J358G, 90 cm, China).
DPSWE in NEG
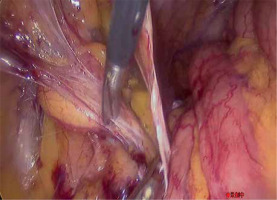
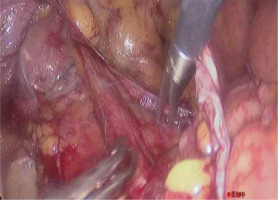
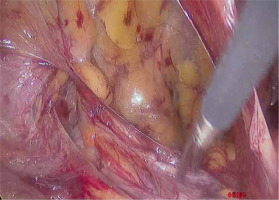
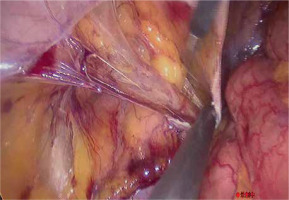
The scissors were slightly opened, and the peritoneum was peeled off by the unfolded blades. The blunt dissection was performed by using the tip of the scissors, and the sharp dissection was performed by using the blades of the scissors, which includes both blunt and sharp dissection. The peeling of the opened scissors was involved partially blunt dissection. The closure of the scissors was purely blunt dissection. When the peritoneum was cut open at the upper edge of the internal ring, attention was paid to the possibility of hemorrhage of the inferior epigastric artery branches. The left hand maintained a certain tension on the tissue to reduce the possibility of hemorrhage (Photo 1). The scissors were used to dissect the preperitoneal space and the forceps were peeled in the opposite direction to gradually separate the Retzius and Bogros space without energy injuries (Photo 2). The scissors were used to dissect the spermatic cord from the hernia sac. When encountering dense adhesion between the hernia sac and the spermatic cord, scissors were cut open to separate the tight connection in the preperitoneal space (Photo 3). The scissors disconnected from the middle of the large hernia sac when it was relatively large. The peritoneum was also separated from the preperitoneal space mainly relying on slightly opened scissors. The scissors were gently and slowly peeled off along the preperitoneal plane. The peritoneum and spermatic cord were completely peeled off with 2–3 times (Photo 4). When separating the dangerous triangle and the pain triangle, scissors were also used to peel off the peritoneal tissue with sharp and blunt dissection. At the vas deferens level, the scissors were slightly opened and gently moved to prevent the damage to the vas deferens (Photo 5). The death coronal was separated with closed scissors. Venous bleeding was compressed through pad, arterial bleeding was stopped through suturing or clipping. The peritoneum was continuously sutured with 1-0 absorbable thread afterwards (Video,  ).
).
Photo 1
Certain tension of the tissue was maintained with the left hand to reduce the possibility of bleeding

Photo 2
The separation of Bogros space was achieved through the closed scissors, sometimes using an aspirator or non-damaging forceps for separation
Postoperative treatment
The hernia sac was disconnected as close as possible to the scrotum to prevent seroma formation. The patch was flattened, reducing the wrinkles, and glue and nail was not used. The elastic bandage was used postoperatively with conventional pressure in two groups. Enhanced recovery after surgery (ERAS) was implemented postoperatively.
Observation indicators
The patients were followed up for at least 3 months. The VAS score, the operation time, hospitalization expenses, hospitalization expenses, scrotal seroma, rupture of hernia sac, vas deferens injury, intraoperative bleeding (> 20 ml), intestinal injury, postoperative bleeding, surgical site infection, length of hospital stay, urinary retention, hernia recurrence were recorded.
Results
The VAS scores in the NEG were lower than those in the EG (p < 0.05). The NEG had no case of CPIP and the EG had 3 cases with early postoperative pain. The EG had 1 case of CPIP. Those can be seen in Table II.
Table II
The VAS scores between the EG and the NEG
| Parameter | EG (n = 53) | NEG (n = 81) | χ2 | P-value |
|---|---|---|---|---|
| Preoperative | 1.21 ±1.45 | 1.12 ±1.63 | 0.067 | 0.219 |
| 24 h after surgery | 3.73 ±2.87 | 1.06 ±2.09 | 5.161 | 0.004 |
| 3 months after surgery | 1.47 ±1.36 | 0.39 ±0.27 | 3.128 | 0.005 |
The operation time in the NEG was shorter than those in the EG (p < 0.05). Hospitalization expenses, scrotal seroma formation, and rupture of hernia sac in the NEG were lower than those in the EG with a statistical significance (p < 0.05). The intraoperative bleeding volume above 20 ml in the NEG was higher than that in the EG. There was no significant difference in the incidence of postoperative bleeding, vas deferens injury, intestinal injury, surgical site infection, length of hospital stay, abdominal wall vascular injury, urinary retention and hernia recurrence in the NEG and the EG (p > 0.05). There was one AIDS patient that had umbilical infection. There was no significant difference in the incidence of surgical site infections (SSIs) in the NEG and the EG. We encountered 2 cases of inferior epigastric artery branches and 1 case of inferior epigastric vein trunk injury with hemorrhage in the NEG. It is more reliable to directly suture the inferior epigastric artery and vein trunk or clamp it for hemostasis. Those can be seen in Table III.
Table III
Comparison of intraoperative and postoperative conditions and complications
Discussion
Exploration of the DPSWE in TAPP
Laparoscopic inguinal hernia surgery achieves very optimistic results. Postoperative pain is relatively mild [18], and the recurrence rate is low. It is being accepted by more and more patients. Laparoscopic inguinal hernia repair (LIHR) requires a high level of professional expertise because of the complexity of the surgery. TAPP is one of very commonly used LIHR. TAPP enters the abdominal cavity first, and the treatment effect for bilateral hernia and occult hernia is significant [19]. Acute postoperative pain, hematoma, and surgical site infection are the risk factors for CPIP, whether it is open hernia repair surgery or LIHR [20]. Olsson suggests that improving surgical techniques can reduce CPIP [20]. We also believe that improvements in surgical techniques may reduce tissue damage and minimize CPIP. The application of DPSWE is also a coincidence. The operating department discovered that the scissors were too fast and lost their sharpness. Our inguinal hernia repair group was required to use scissors without electrocoagulation. The use of non-electric dissecting scissors was gradually increasing, while the use of electric hooks and ultrasound knives for replacement was gradually decreasing. Gradually the use of DPSWE has emerged throughout the process.
Essential prerequisites for DPSWE
(1) Embryological planes provided convenience for DPSWE. The embryological plane has been widely applied in minimally invasive surgery for colorectal cancer [21]. There are few large blood vessels in the anatomy of an avascular embryonic plane, reducing the possibility of hemorrhage. The application of embryonic plane can also reduce hemorrhage in TAPP. Surgeons can clearly dissect the embryological plane with non-electric scissors, which may reduce the possibility of electrocoagulation leading to entering into the incorrect anatomical level. Rapid dissection of the preperitoneal space resulted in minimal bleeding during IH repair, reducing the frequency of replacing hemostatic tools such as monopolar hooks. Even if the hemorrhage occurs, the bleeding was gradually stopped for a while. It made the surgery time faster. Although the intraoperative bleeding volume above 20 ml in the NEG was higher than that in the EG, the operation time of the NEG with DPSWE was shorter. (2) The DPSWE requires proficient use of scissors: the non-electric scissors do not cause thermal damage to the tissue. The technique of using slightly open scissors to dissect loose connective tissue is commonly used in the dissection of the axillary lymph nodes for breast cancer, as well as for separating extensive intestinal adhesions in the abdominal cavity during open surgery. The scissors were gently opened and were kept in a fixed state. This technology requires short-term training, but there are still some difficulties. Some common techniques need to be mastered: A. We need to keep the blade of the scissors slightly in an open and fixed state; B. The key is to gently peel off the loose connective tissue on the uneven preperitoneal plane with the scissor blades. C. This technique combines the blunt and sharp dissection. The dissection of scissors in the closed state was completely blunt dissection and the dissection of scissors with the open blades was partly sharp dissection. Loose connective tissue should be dissected in the closed state. For example, the dissection of the Bogros space from the preperitoneal tissue can be achieved through scissors in a closed state. D. This technology is used to separate different tissues in different open states. When the adhesion with the tissue is tight, the scissors should be slightly opened. For example, the separating tissue between the peritoneum and iliac blood vessels can achieve the desired effect with the slightly opened blades of the scissors. The scissors should be larger when separating the hernia sac from the spermatic cord and surrounding tissues of the vas deferens because the adhesion of tissue is tight. E. The surgeon should maintain a certain traction tension on the left hand to reduce the possibility of hemorrhage. F. The sharpness of each scissor blade varies and can only be adjusted during actual operation because the sharpness of each pair of scissors blade varies. (3) Accidental hemorrhage required a complete set of hemostatic techniques. For critical arterial bleeding, clamping the artery to control bleeding is crucial. The key is to clamp the bleeding vessel with the left hand and keep it under control. When holding the clamp in the right hand, it can be quickly and accurately clipped and the bleeding stops.
Advantages of DPSWE
(1) DPSWE does not have thermal damage. The energy of electrolytic dissection can lead to thermal damage, abdominal organ perforation, and even a risk of death [22, 23]. There is no thermal damage to the tissues in DPSWE. Although there were no cases of intestinal perforation among these 53 patients in the EG, there is a possibility of intestinal heat injury in the future as the data increase. (2) DPSWE may have less postoperative pain. The VAS scores in the NEG were lower than those in the EG (p < 0.05). The NEG had no case of CPIP and the EG had 3 patients with early postoperative pain. And the EG had 1 case of CPIP. The patient of CPIP gradually returned to normal work after 6 months of pain management. Electrocoagulation of preperitoneal tissue may lead to tissue necrosis, with necrotic tissue gradually absorbing, and tissue reconstruction and repair. The process of dissolution, absorption, and reconstruction may produce inflammatory mediators that cause pain in patients. DPSWE may reduce tissue necrosis, reduce postoperative tissue inflammatory response, reduce nerve thermal damage, and reduce tissue wound repair, which may be an important aspect of reducing postoperative pain. DPSWE may be a better method to dissect the preperitoneal space. We did not use tails and glue to reduce the interference caused by patch fixation intraoperatively. These two groups did not routinely use painkillers after surgery to reduce interference factors caused by medication factors. There are also some important risk factors that are not related to surgical techniques and can lead to CPIP, such as coagulation disorders, congestive liver disease, and heart failure [24]. Because our hospital was also a key treatment unit for liver diseases, some patients with liver cirrhosis were accompanied by inguinal hernia, and even a large amount of ascites is formed in the scrotum. Inguinal hernia with a large amount of ascites is a complex surgery. They were referred to our hospital for open hernia repair mainly under local or general anesthesia, which is not included in the statistics. The defect of inguinal hernia larger than 3 cm was routinely sutured to close the defect area of the transverse fascia [17]. After more than 3 months of postoperative follow-up, no recurrence cases were found. No postoperative pain related cases occurred due to recurrence. CPIP is one of the most significant long-term complications after IH repair [20]. As the data gradually increase, the results of this study may achieve better results. Furthermore, the inability to design this study as a double-blind controlled study is also a drawback. (3) The operation time was significantly shortened and this had statistical significance. It may be related to the combination of blunt and sharp dissection with the scissors. The slightly opened blade of scissors significantly increased the separation speed of the preperitoneal space, especially the adhesion between the peritoneum and the danger triangle, pain triangle, and vas deferens, which quickly dissociates within a few seconds. (4) The reduction in hospitalization costs may be related to a significant reduction in surgical time. During surgery, it was found that most cases did not require the addition of a second dose of muscle relaxants, which requires further clinical confirmation [17]. (5) The significant reduction in scrotal seroma and less tissue damage may be related to the rapid adhesion of the two layers of tissue, maximizing the release of seroma of the hernia sac during surgery. (6) There is a significant statistical significance in the comparison between the NEG and the EG in terms of the decrease in the rupture of hernia sac. The blunt separation with scissors may reduce the risk of the rupture of peritoneum in the NEG. The peritoneal tissue is prone to rupture with electrocoagulation. Vas deferens injury was not encountered in the NEG, while 4 cases were encountered in the EG. Although not statistically significant, further confirmation is needed in the increasing amount of data. (7) DPSWE emphasizes the role of mild compression of elastic inguinal bandages after covering the inguinal area with pads postoperatively. The hematoma caused by postoperative bleeding may be related to surgical techniques and postoperative pressure bandages. This was the same as the skin grafting of limbs that the recipient site and graft fixation method were the primary influences in early postoperative full-thickness skin graft complications and successful graft take [25]. Local pressure bandaging in the inguinal area and non-necrotic tissue on the wound surface may promote tissue adhesion, reduce local bleeding and scrotal seroma and tissues. (8) The probability of infection may be very low when using DPSWE theoretically. Necrotizing tissue may lead to bacterial proliferation [26]. The devitalized tissue provides a suitable culture medium for bacterial growth, and wounds containing necrotic tissue are therefore at risk of becoming clinically infected [27]. But no patch-related peripheral tissue infections were observed in both EG and NEG, and further confirmation is needed in future large amounts of data. Our hospital is also a designated hospital for AIDS patients in Shanghai city. These patients with IH have taken highly effective antiviral drugs for a long time. For immunosuppressed patients with AIDS, diabetes, and obesity, perioperative antibiotic prophylaxis is not commonly used due to the short operation time [28], and no infections caused by the implantation of patches in the preperitoneal space were encountered, which may be related to the small number of cases and require further cases verification. We had 1 case of the umbilical puncture trocar infection who was an AIDS patient in the EG, and the wound dressing change showed that the umbilical puncture point walked too long along the subcutaneous tissue, and the subcutaneous fat tissue infection was the main reason. After half a month of dressing change, the umbilical infection was cured, which was not likely to be related to whether electrocoagulation dissection was used during surgery. (9) DPSWE does not damage TF. It may maximize the protection of nerves in the pain triangle, reducing pain triangle nerve damage, and protect the external iliac artery and vein below from damage.
Disadvantages of DPSWE
The intraoperative bleeding above 20 ml significantly increases. The intraoperative bleeding requires perfect hemostasis, and the postoperative bleeding did not significantly increase. The drawbacks of DPSWE can be summarized in four aspects: (1) The hemorrhage comes from the branches of the inferior epigastric vessels. We encountered 2 cases of the branches of the inferior epigastric arteries and 1 case of the inferior epigastric venous trunk injury in the NEG. Hemostasis is more reliable after the suture the inferior epigastric vessels. After the avascular peritoneum was cutting through outside the internal ring, the scissors can effectively avoid damaging the branches of the inferior epigastric vessels by evenly and forcefully pulling the peritoneum with the left hand towards the spinal side and maintaining sufficient tension. The peritoneum was pulled away from the inferior epigastric vessels. (2) We encountered one case of DPSWE with obturator hemorrhage. The scissors in a closed state come into contact with the obturator vein on the pubis, and the wound is compressed for 5 min before stopping. (3) No external iliac blood vessel bleeding was found. (4) We often encountered small vessel bleeding in DPSWE. When dissecting the triangular pain, vas deferens, the spermatic cord, the hernia sac and the adhesion between the peritoneum and transverse fascia, the peritoneum were gently peel off the transverse fascia. The peritoneum was pulled and tension was maintained with the left hand, and the severe hemorrhage was rarely encountered. It was the exudation of venous and capillary intraoperative. The hemorrhage stops quickly. The gauze can be compressed to stop bleeding. The groin was bandaged with a pad by the abdominal band postoperatively. Although there was an increased tendency for bleeding intraoperatively, obvious hemorrhage was not found postoperatively. However, due to the lack of more sufficient data, the difference in bleeding rates between the NEG and the EG at the surgical site needs to be further confirmed through extensive data.
Conclusions
DPSWE may have good safety in the treatment of IH. Compared to electrolytic dissection in TAPP, it may shorten surgical time, reduce scrotal seroma, reduce postoperative pain, promote postoperative recovery of IH patients, and reduce hospitalization costs. Proficient use of scissors results in mild tissue damage, minimal vascular damage, and fast surgical time. The surgical effect may vary among different doctors depending on the level of proficiency in using scissors. Therefore, in the clinical treatment of IH, the selection of DPSWE should be based on the proficient use of scissors by skilled surgeons. Further observation is needed in future data to determine whether the extensive use of scissors increases damage to other tissues. However, DPSWE needs to be further determined through multicenter, large-scale comparative studies in clinical practice with a double-blind experiment. Sharp and blunt dissection with scissors in TAPP allows surgeons to operate in the preperitoneal bloodless space, thereby significantly reducing the possibility of damage to blood vessels, peritoneum, and other tissues. It may be beneficial to patients and doctors, and may be worthy of clinical promotion.