Introduction
Non-neoplastic lesions within the urinary bladder are characterised by diversity and paramount importance in precise diagnosis [1]. Endocervicosis, an extremely rare condition derived from Müllerian tissue, primarily manifests in the urinary bladder. It is distinguished by benign infiltration of endocervical glands, first described by Goodfall in 1943 [2, 3]. Bladder endocervicosis, characterised by mucinous epithelium, exhibits no cellular atypia, with only a few cases reported in the current literature. Clinical presentation varies, from incidental discovery due to persistent urinary tract symptoms, dysmenorrhoea, or chronic pelvic pain [4]. Lesions may affect diverse bladder areas, and differential diagnosis included urothelial or urachal tumours, cystitis glandularis, and urachal remnants [5]. Imaging tools and cystoscopy depict bladder wall masses without consensus on the ideal surgical approach [3, 4]. Definitive diagnosis requires comprehensive tissue analysis, revealing unique histopathological features [4].
This case of a 47-year-old woman with urinary bladder endocervicosis treated with tumour-only excision with minimal free surgical margins contributes valuable insights to the understanding of urinary bladder endocervicosis, diagnostic complexities, and evolving management strategies for this rare medical entity.
Case report
A 47-year-old woman presented to the Urology Department with a history of chronic pelvic pain, after an uneventful hysterectomy conducted 2 years prior as part of adenomyosis treatment. The patient’s surgical background included a hysterectomy and 2 previous caesarean sections. There were no reported urinary system symptoms, such as haematuria or recurrent urinary tract infections. Both the clinical examination and laboratory analyses yielded unremarkable results. Ultrasound of the urinary bladder and lower abdominal magnetic resonance imaging (MRI) scan revealed a spherical mass measuring 28.7 × 27 mm located within the dome of the urinary bladder, protruding from the moderately thickened bladder wall (Figs. 1 A–C). Additionally, cystoscopy identified a solid formation within the bladder dome, characterised by an intact urothelium at the lesion site, while the remaining urinary bladder mucosa exhibited no pathological alterations.
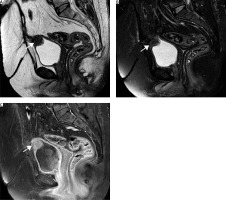
Fig. 1
A solid lesion on the bladder dome with relatively smooth margins and intraluminal protrusion shows intermediate signal in (A) T2-weighted (T2W) and (B) fat-saturated T2W sequences, as well as (C) homogenous enhanced in contrast--enhanced fat-saturated T1-weighted images
The patient received a thorough explanation that the lesion could be either malignant or benign. Additionally, the surgical options, including transurethral excision of the tumour, partial cystectomy, or excision of the lesion only, were discussed in detail. Upon thorough evaluation, it was determined that opting for a segmental cystectomy with circular tumour excision, leaving 0.5 cm of free surgical margins would ensure the thorough removal of the lesion while preserving the integrity of the bladder and avoiding extensive tissue removal. The excised mass displayed smooth contours and intact cystic mucosa. Subsequent reconstruction of the bladder involved a meticulous two-layer suturing technique. A urinary catheter was introduced postoperatively and was subsequently removed without complications one week post-surgery.
The histopathological examination of representative small sections from the aforementioned lesion revealed features consistent with endocervicosis (Figs. 2 A–F). Immunohistochemical analysis demonstrated positivity for oestrogen and progesterone receptors, as well as for markers HBME1, Ca125, CAM5.2, and CK20. Conversely, it returned negative results for CD10, mCEA, and CDX2. The overlying urothelium displayed no significant alterations.
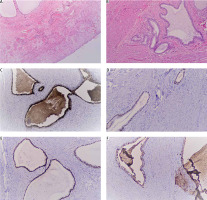
Fig. 2
Immunohistochemical results confirmed the existence of the endocervical type glands in the urinary bladder specimen (A) HE × 4, (B) HE × 10, (C) Ca125-positive marker, (D) strong expression of oestrogen receptors, (E) strong expression of progesterone receptors, (F) HBME-1 staining was detected
Throughout the 1-, 3-, and 6-month follow-up periods, no recurrence was observed in the ultrasonographic control of the urinary bladder, and the patient consistently reported a smooth postoperative course and progressive relief from her presenting symptoms.
Discussion
In 1943, Goodfall introduced the term “endocervicosis” to describe cases marked by deep infiltration of cervical and paracervical tissues with apparently benign endocervical glands [2]. This rare condition, sharing a Müllerian origin with endometriosis and endosalpingiosis, exhibits distinct endocervical differentiation. Endocervicosis is the rarest among Müllerian lesions, probably originating from pelvic or retroperitoneal tissues [3]. While primarily found in the bladder, sporadic cases involve axillary lymph nodes, rectum, vagina, small intestine, and mesosalpinx [3, 6]. Bladder endocervicosis features mucinous epithelium in the bladder wall, possibly with cystic dilation, lacking cellular atypia [3, 7]. Despite the benign nature of bladder endocervicosis, a recent case of adenocarcinoma associated with bladder endocervicosis has been reported by Nakaguro et al. [7]. The literature documents fewer than 40 ca- ses [4].
Debates on endocervicosis’ origin centre on 2 theories, primarily in reproductive-age women. The implantation theory suggests cell migration post-surgery, which is common after procedures like caesarean sections or pelvic surgeries, as in this instance. Conversely, the metaplastic theory proposes cell transformation from the posterior peritoneum due to hormonal influences [7–9]. While some lesions are incidental findings, patients typically present with symptoms such as urinary frequency, dysuria, and chronic pelvic pain. Most lesions are located on the posterior bladder wall or dome, with some causing bladder adhesions or involving the bladder neck or trigone. Reported lesion sizes range 1–6 cm, averaging 3.2 cm [4].
The differential diagnosis should encompass potential considerations such as urothelial or urachal tumours, cystitis glandularis, or urachal remnants [5]. Despite the importance of preoperative diagnosis, there is a lack of established and precise diagnostic tools for cervical endocervicosis. The diagnostic challenge arises due to the existence of numerous glandular lesions, both pseudoneoplastic and neoplastic, requiring careful differentiation [3]. Various imaging studies, including computed tomography, sonography, and, in specific instances, MRI, depict a solitary small mass within the bladder wall [3, 10]. Urethrocystoscopy findings typically indicate a mural lesion, primarily situated on the posterior bladder wall and covered by normal bladder mucosa [9, 10].
Therefore, physicians must maintain a heightened level of awareness and suspicion when evaluating a woman with abdominal or pelvic pain, recognising the intricate nature of potential underlying conditions. This necessitates thorough investigation, including abdominal and pelvic ultrasonography, as well as advanced imaging techniques like MRI or computed tomography. While tumour markers such as CA-125 can aid in distinguishing between benign and malignant conditions, their sensitivity and specificity for malignancy are limited, underscoring the importance of integrating multiple diagnostic modalities for accurate assessment and timely intervention [11–13].
Optimal surgical management for bladder endocervicosis remains debatable, contingent upon tumour size, location, and number. Transurethral resection, serving both diagnostic and therapeutic purposes, is commonly employed. In select cases, partial cystectomy, whether open, laparoscopic, or robotic, offers complete resection albeit with increased complexity [3, 4]. However, to ensure comprehensive excision of the lesion while preserving bladder function, segmental cystectomy with minimal free surgical margins, as in this case, emerges as the ideal approach. This not only guarantees lesion removal but also safeguards bladder integrity, reducing the likelihood of postoperative complications.
A definitive diagnosis is confirmed through a comprehensive analysis of tissue pathology, relying on the examination of cellular structure and cytological observations [7, 9]. Histopathological examination reveals a seamless presence of ciliated and non-ciliated epithelium juxtaposed with the bladder’s transitional epithelium. Tubular structures, exhibiting mucin-secreting properties and branching patterns akin to mucinous adenomas, dominate. The stromal component is less pronounced [4]. Notably, endocervicosis glands demonstrate heightened expression of uterine-reactive antibodies, notably HBME-1, oestrogen receptor, and progesterone receptors [14].
Conclusions
The rarity of this Mullerian-derived condition, marked by benign endocervical gland infiltration, underscores the need for thorough understanding and management. Differential diagnosis complexities require careful preoperative evaluation. Despite its usually benign nature, recent cases hint at adenocarcinoma association, emphasising meticulous management. Accurate diagnosis crucially informs surgical intervention, with transurethral resection and partial cystectomy common choices. Opting for tumour-only excision with free surgical margins ensures the thorough removal of the lesion, reducing the probability of re-operation and preventing the removal of a significant portion of the urinary bladder.











