Introduction
Pressure ulcer (PU) is caused by long-term pressure on the skin of the body, which affects blood circulation, resulting in injury, ulcer, and even necrosis due to a lack of nutrition in the skin and subcutaneous tissue [1, 2]. It is more likely to occur in the stressed bones, such as the sacrococcygeal bone, ankle, heel, hip, etc. [3]. PU is a catastrophic comorbidity of bedridden and elderly patients, characterized clinically by chronic wounds that are difficult to heal. In different health care institutions around the world, especially intensive care units (ICU), PU is a common and costly health problem, which is considered to continuously affect patients’ health status, quality of life, and health care resources, as well as a major problem of overuse of medical expenses [4]. PU will bring a series of harm, increase the pain of patients, aggravate the underlying condition, prolong the course of disease, and even cause sepsis and is life-threatening. The formation of PU is a complex process, which is caused by deformation and necrosis of skin tissue caused by local and systemic factors. PU tends to occur in stressed bone protrusions [5, 6]. Early pressure skin may appear as a colour change, mild oedema. With the progression of the disease blisters, ulcers can appear, severe cases can deepen to the muscle, bone or joint, the formation of necrosis, secondary infection can cause sepsis. Among them, stage III PU is a shallow ulcer stage, in which the damage has reached the deep skin, and subcutaneous fat can be observed from the wound site, but muscles, tendons, bones, etc., have not been exposed [7]. Stage IV PU is the stage of deep ulcer, at which the injury is deeper, with exposed muscles, tendons, bones, etc., rotting flesh may also appear at the bottom of the wound, osteomyelitis may also be complicated, and the symptoms of systemic high fever, chills, pus flow, fracture of the diseased bone, and discharge of bone fragments may occur [8, 9].
At present, topical ointment is often used to care for PU in the clinic, but the care of PU is not accomplished overnight. Besides basic wound care and treatment, family members must also do well in daily care work, and the key points of PU care in different stages are slightly different [10]. Vacuum sealing drainage (VSD) refers to the sealing drainage of the skin or soft tissue defect with a polyethylene alcohol hydrate algal salt foam dressing containing a drainage tube, sealing it with a bio-permeable membrane to make it a sealed space, and finally connecting the drainage tube to the negative pressure source [11, 12]. It is a brand-new treatment method to promote wound healing through controllable negative pressure [13]. Platelet-rich plasma (PRP) refers to concentrations of platelets that are extracted from autologous blood by centrifugation. Because PRP can promote the repair of bone and soft tissue, and comes from the body, no immune rejection, simple production, little damage to the body occur. In recent 20 years, PRP has been applied in a variety of disciplines, such as orthopaedics, oral and maxillofacial surgery, cardiothoracic surgery, neurosurgery, obstetrics and gynaecology, ophthalmology, otolaryngology, general surgery, plastic and aesthetic surgery, etc., especially in European and American countries [14, 15]. A large number of clinical studies have reported that the application of PRP can accelerate fracture healing, promote wound repair, reduce intraoperative anaesthetic dose, reduce intraoperative bleeding and postoperative wound exudation, relieve pain, reduce postoperative complications, shorten hospital stay, and promote postoperative functional recovery, etc. [16].
In summary, the selection of treatment plans for PU patients is still a hot topic of clinical concern. In this work, 110 PU patients admitted to our hospital from January 2021 to January 2023 were included as research objects, and were randomly divided into an experimental group (Exp group) and a control group (Ctrl group) by blind selection, with 55 cases in each group. Patients in the Ctrl group received surgical debridement + VSD, while those in the Exp group received Bikerui disinfectant + VSD + PRP. Inflammatory response (IR) score, PU healing (PUH) score, healing time, dressing change frequency (DCF), dressing interval time (DIT), and scar recovery (SR) score of patients in different groups were compared to investigate the effect of Bikerui disinfectant + VSD + PRP on patients with stage III–IV PU.
Material and methods
Research objects
As mentioned above, 110 PU patients treated in The Second Affiliated Hospital of Xingtai Medical College from January 2021 to January 2023 were selected and randomly divided into an Exp group and a Ctrl group by a blind selection method, with 55 cases in each group. The subjects agreed to sign an informed consent form with the consent of their family members. The implementation of the study has been approved by The Second Affiliated Hospital of Xingtai Medical College (ethical number is SAHXMC23613). Pairwise comparison of age, male-female ratio, number of PU, area of PU, PU location, PU source, and average course of disease (COD) of patients in various groups showed no great significance (p > 0.05), as listed in Table 1.
Table 1
General data of patients before they were treated differently
Criteria based on which the patients were enrolled were as follows: 1) the duration of PU was longer than 2 months; 2) the recovery effect after conventional treatment was not good; 3) patients who did not want to receive skin grafting or flap surgery; 4) haemostasis still failed after conventional treatment; and 5) no immunosuppressive agents and hormones had been applied.
Based on the following criteria the patients were enrolled: 1) with severe malnutrition; 2) combined with haematological diseases; 3) combined with mental diseases; 4) without relevant baseline data; and 5) with shorter hospital stay.
Treatment schemes
All patients were given basic treatment, assisted in turning over, skin cleaning, and nutritional support. To understand the psychological state of patients, psychological counselling was provided for patients with anxiety and tension.
In the Ctrl group, surgical debridement + VSD was applied. Local wound debridement was performed firstly. After cleaning with 0.9% isotonic saline, foam dressing was affixed to the wound surface, sealed, and suction cups and suction tubes were connected for continuous negative pressure suction at a pressure level of about 100 mm Hg. It was rinsed regularly with isotonic saline and hydrogen peroxide, and the dressing was changed once a week. Treatment was stopped when new granulation appeared on the wound.
For the Exp group patients, the Bikerui disinfectant + VSD + PRP technology was given. Firstly, Bikerui disinfectant was employed to continuously clean the wound surface of the patient, and the skin folds could be opened by hand to complete the cleaning. After the cleaning was completed, the foam dressing was affixed to the wound surface, sealed, and the suction cup and suction tube were connected for continuous negative pressure suction at a pressure level of about 100 mm Hg. It was rinsed regularly with isotonic saline and hydrogen peroxide, and the dressing was changed once a week. The negative pressure treatment was stopped when new granulation appeared on the wound. The gel prepared with PRP was applied externally to the patient’s wound and changed every 3 days while routine dressing changes were performed.
Observed indicators
1) The Pressure Ulcer Scale for Healing (PUSH) was selected to evaluate the wound healing effect of the two groups. The scale included three parts: wound area, 24-hour exudation volume, and wound tissue type. The highest score was 10 points for wound area, 3 points for 24-hour exudation volume, and 4 points for wound tissue type. The total score was 0–17 points. The higher the score, the more serious the PU wound state.
2) The average healing time, average DIT, average DCF, and total treatment cost of patients treated with different methods were recorded.
3) The wound secretions of the two groups were collected before and after treatment (before treatment, 1 week, and 2 weeks after treatment), and bacterial culture was performed to calculate the incidence of positive bacteria in the patients.
4) Wound IR scale was employed to evaluate the degree of wound inflammation in the two groups, including the red and purple range, pain degree, swelling degree within 2 cm of the skin margin, and skin temperature, with a total score of 18.
5) The clinical efficacy of patients was assessed as cured (wound healing, scab, shedding, and pain relief), markedly effective (the wound was greatly reduced, the new granulation grew well, and the pain was significantly relieved), effective (the wound was obviously reduced, the new granulation grew, there was still a small amount of exudation, and the pain was somewhat relieved), and ineffective (wound surface did not improve obviously, granulation tissue growth was not obvious, there was a lot of exudation and purulent secretions, the pain was aggravated). The total effective rate (TER) = (Cured + Markedly effective + Effective)/(Total cases) × 100%.
6) The scar recovery of the two groups was evaluated by the Vancouver Scar Scale (VSS), which is a universal scar assessment method in the world. This scale did not require special equipment, but only relied on the naked eye observation of the tester and palpation of the patient’s scar with bare hands, and was measured in four aspects: colour, thickness, blood vessel distribution, and softness. The total score was 15, with a higher score indicating more severe scar hyperplasia.
Statistical analysis
The research data processing was implemented using SPSS19.0, measurement data were expressed using the mean ± standard deviation (x ± s), and the count data were expressed as a percentage (%). The relevant indicators were compared by repeated measure analysis of variance. By bilateral test, p < 0.05 was statistically significant.
Results
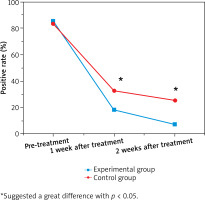
Comparison of the positive rate of bacterial culture of wound secretions
The positive rate of bacterial culture of wound secretions was compared in Figure 1 below. The positive rate of bacterial culture of wound secretions in the Exp group was 85.45% before treatment, 18.18% 1 week after the treatment, and 7.27% 2 weeks after the treatment. It was 83.64%, 32.73%, and 25.45% in the Ctrl group at the above three time points, respectively. It suggested that the positive rate of bacterial culture of wound secretions for patients before they were treated showed no great difference (p > 0.05) but that for patients receiving the Bikerui disinfectant + VSD + PRP was observably lower than that for those treated with surgical debridement + VSD 1 and 2 weeks after they were treated (p < 0.05).
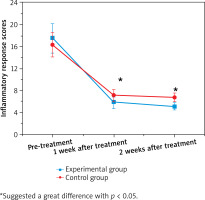
IR scores of patients in various groups
Figure 2 illustrated the IR scores of patients in different groups. As demonstrated, the IR scores in the Exp group and Ctrl group were 17.51 ±2.66 and 5.82 ±1.04, respectively before they were treated, showing no obvious difference (p > 0.05). After treatment, the IR scores in the Exp and Ctrl groups were 5.82 ±1.04 and 7.08 ±1.14 1 week later and 5.11 ±0.72 and 6.73 ±0.85 2 weeks later, respectively, exhibiting a remarkable difference (p < 0.05).
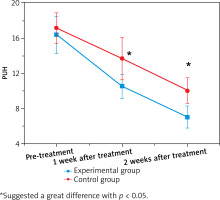
PUH score of patients after they were treated with different methods
The PUH scores of patients before and after they were treated were compared in Figure 3. Before they were treated, the PUH score in the Exp group was 16.34 ±2.08 and showed a great difference compared to that in the Ctrl group (13.66 ±2.38) (p > 0.05). After they were treated for 1 week, the PUH score was 10.52 ±1.34 in the Exp group and 13.66 ±2.38 in the Ctrl group, showing a great difference with p < 0.05. After the patients were treated with different methods, the PUH score in the Exp group was 7.04 ±1.25, which was much lower than that in the Ctrl group (10.02 ±1.44), showing a remarkable difference (p < 0.05).
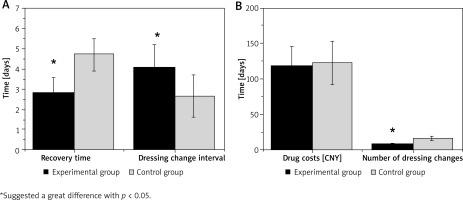
Healing time, DIT, DCF, and drug cost of patients
The healing time, DIT, drug cost, and DCF in the Exp group were 2.81 ±0.75 days, 4.07 ±1.1 days, 118.42 ±27.85 CNY, and 8.52 ±1.43 times, respectively; while those in the Ctrl group were 4.73 ±0.48 days, 2.66 ±1.05 days, 122.81 ±30.46 CNY, and 16.13 ±2.77 times, respectively. It suggested that the healing time, DIT, and DCF showed great differences with p < 0.05 and the drug cost exhibited no obvious difference (p > 0.05). The above results were specified in Figure 4.
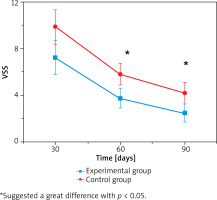
Scar recovery scores of patients after they were treated
The scar recovery scores 30, 60, and 90 days after the patients were treated were 7.21 ±1.44, 3.72 ±0.83, and 2.49 ±0.76 in the Exp group, respectively; while those in the Ctrl group were 9.84 ±1.51, 5.79 ±0.93, and 4.18 ±0.89, respectively. It indicated that the scar recovery scores for patients receiving Bikerui disinfectant + VSD + PRP were much lower than those for patients with surgical debridement + VSD, showing great differences with p < 0.05. The above results were illustrated in Figure 5.
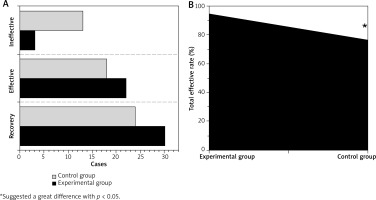
Clinical efficacies of patients with different treatment methods
As demonstrated in Figure 6 A, 30, 22, and 3 patients were cured, effectively treated, and ineffectively treated in the Exp group; while the numbers of patients with cured, effective, and ineffective efficacy in the Ctrl group were 24, 18, and 13, respectively. Figure 6 B illustrated that the TER of patients receiving the Bikerui disinfectant + VSD + PRP (94.55%) was much higher than that for patients receiving the surgical debridement + VSD (76.36%), showing an obvious difference with p < 0.05.
Discussion
PU tends to occur in people who have been bedridden for a long time or have difficulty in mobility, and it mostly occurs in the parts of bone protrusion. Long-term pressure on local tissues of the body leads to blood circulation disorders, and often causes lesions such as ulcers, blisters, and even rotting flesh [17]. With the continuous improvement of clinical cognition of PU, patients with stage III and IV PU have more serious diseases. Conventional treatment has been unable to achieve good clinical effects, and may lead to the exacerbation of the disease and the prolongation of the course of the disease [18]. Patients need long-term dressing changes, which brings adverse effects on their physical and mental health and quality of life [19, 20]. In this study, 110 PU patients admitted to our hospital from January 2021 to January 2023 were included as research objects, and were randomly divided into the Exp group and the Ctrl group by blind selection, with 55 cases in each group. Patients in the Ctrl group received surgical debridement + VSD, while those in the Exp group received Bikerui disinfectant + VSD + PRP. From/As compared to baseline data, pairwise comparison of age, male to female ratio, PU number, PU area, PU location, PU source and average course of disease between the two groups was not statistically significantly different (p > 0.05). The principle of equilibrium means that in addition to different treatment factors, other factors affecting the observation results should be consistent as far as possible. The equilibrium of baseline data between groups is to ensure the comparability between groups of the observation results of response variables so as to investigate the real impact of treatment factors on the observation results under similar baseline conditions [21]. Therefore, the above results provide feasibility for the inter-group comparison of relevant indicators.
Bacterial culture in this work showed that the positive rate of bacterial culture of wound secretion in the Exp group was much lower than that in the Ctrl group at week 1 and 2 after treatment (p < 0.05). This is similar to previous reports on the anti-inflammatory and bacteriostatic effects of PRP, indicating that Bikerui disinfectant + VSD + PRP treatment can effectively reduce the possibility of bacterial infection in PU patients [22]. IR is an important immune defence mechanism in the body. When the tissue is damaged or infected by toxins or bacteria, damaged by heat or other causes, it will enter the normal state of self-protection and damage repair. Therefore, IR is also a defensive response of human body to stimuli [23, 24]. It was found that IR score in the Exp group was much lower than that in the Ctrl group at week 1 and 2 after treatment, and the difference was statistically significant (p < 0.05). It indicated that Bikerui disinfectant + VSD + PRP treatment could effectively improve IR in PU patients. The PUH score in the Exp group 1 and 2 weeks after treatment was much lower than that in the Ctrl group (p < 0.05). It was indicated that Bikerui disinfectant + VSD + PRP treatment could effectively promote wound repair and growth of new granulation tissue in patients. The average healing time and DCF in the Exp group were visibly lower than those in the Ctrl group, while DIT was observably higher than that in the Ctrl group, showing great differences (p < 0.05). This indicated that Bikerui disinfectant + VSD + PRP treatment could effectively shorten the healing time of patients’ wounds and reduce the DCF given by doctors. Scar is a natural product in the process of human wound repair. Skin wounds that affect the epidermis only can be healed by simple epithelium formation, and the appearance and function of the skin can be completely recovered after repair, while injuries that reach deep dermis and subcutaneous tissue must be repaired by scar [25]. It was found that scar recovery scores in the Exp group at 30, 60, and 90 days after treatment were much lower than those in the Ctrl group (p < 0.05). It indicated that Bikerui disinfectant + VSD + PRP treatment exerted a significant promoting effect on scar recovery in PU patients. Further analysis of clinical efficacy showed that the TER in the Exp group (94.55%) was higher than that in the Ctrl group (76.36%), exhibiting a visible difference (p < 0.05). It indicated that Bikerui disinfectant + VSD + PRP treatment effectively improved the clinical efficacy of PU patients.
Conclusions
110 PU patients admitted to our hospital from January 2021 to January 2023 were included in this work. All patients were randomly divided into the Exp group and the Ctrl group by blind selection, 55 cases in each group. Patients in the Ctrl group received surgical debridement + VSD treatment, while those in the Exp group received Bikerui disinfectant + VSD + PRP treatment. The IR score, PUH score, healing time, DCF, DIT, and scar recovery scores of patients in different groups were compared. The results revealed that Bikerui disinfectant + VSD + PRP treatment could effectively improve the inflammatory degree of PU patients, promote the wound repair and scar recovery, and obviously improve the clinical efficacy of PU patients. However, this work had some potential limitations, including a small sample size, a short follow-up period, and no long-term data collection of patients after treatment. Therefore, in the later period, clinical data of some PU patients will be collected to further clarify the clinical effect of Bikerui disinfectant and VSD combined with PRP. In conclusion, this work offered a theoretical basis for PU treatment in the clinic.