Introduction
Congenital diaphragmatic hernia (CDH) is an embryological defect or hypoplasia of the diaphragm allowing abdominal viscera to herniate into the thoracic cavity, being associated with pulmonary hypoplasia endangering the developing lungs antenatally.
Such fusion defects of the diaphragm can be unilateral or bilateral; the most common is unilateral, left posterolateral defects (Bochdalek hernia, 95%), followed by anterior retrosternal defects (Morgnagni, 4%) and the less common hiatal hernia and septum transversum defects in 1%. Among 10 to 20% have the peritoneal sac at the site of Bochdalek hernia without any muscle fibres in it.
Aim
The purpose of this study was to analyse the clinical profile and the outcome of congenital diaphragmatic hernia with a sac in neonates and children in a paediatric referral centre.
Material and methods
This observational clinical cohort study was conducted from January 2005 to December 2021 evaluating both retrospectively and prospectively, over a period of 16 years at a tertiary care neonatal paediatric centre.
Patient records were collected and critically evaluated, from a neonatal intensive care unit, paediatric surgery operative registry and a questionnaire distributed to care takers. Infants, children and neonates referred with a clinical diagnosis of left and right congenital diaphragmatic hernia with a sac were included in the study. The chest radiography and ultrasonography helped in establishing the clinical diagnosis (Figure 1).
Figure 1
A – Chest radiography of left congenital hernia with sac. B – Chest radiography of right-sided congenital diaphragmatic hernia with sac. C, D – Intra-operative picture of CDH with sac. E – Opened sac of CDH showing underlying lung. F – Repaired right CDH with a sac. G – Repaired left CDH with a sac. H – Post-operative chest radiography. I – Histopathology of the sac (low power field) – sac lined with flattened mesothelial cells with stromal hyalinisation and few inflammatory infiltrates in the background of fibrocollagenous tissue

Computed tomography contrast enhanced (CECT) and upper gastrointestinal dye studies were conducted very rarely in doubtful cases. Study subjects were grouped according to the pre-operative and intra-operative diagnosis. Group I (LCDHS) included left-sided congenital diaphragmatic hernia with sac, and group II included right-sided congenital diaphragmatic hernia with sac (RCDHS).
Neonates and children with diaphragmatic eventration and acquired diaphragmatic defects were excluded. Cases with incomplete data or non-availability of information on the type and size of the defect and presence of a hernial sac in the operative registry/notes were excluded. Cases of Morgagni hernias, pentalogy of Cantrell and those with pre-operative mortality were also excluded.
Hence all surgically repaired patients having CDH with a sac diagnosed between January 2005 and December 2021 in a tertiary care centre were included in this study.
Two-dimensional (2D) echocardiography was used to detect cardiac anomalies. Neonates and children if required were given assisted ventilation both pre- and postoperatively. The surgical procedure was performed when the general medical condition improved after initial stabilisation, which was evidenced by improved blood gas analysis and controlled primary pulmonary hypertension over at least 24 hours.
The institutional ethical committee approved this study.
Tensionless, proper closure of the diaphragmatic defect is the surgical principle, which can be accomplished by an open or minimally invasive approach; laparotomy/thoracotomy or thoracoscopic or laparoscopic approaches were implemented (Figures 1 F, G). A subcostal incision on the relevant side was made under general anaesthesia, the herniated viscera and bowel were gently reduced into the abdominal cavity, and the diaphragmatic defect was closed with interrupted non-absorbable sutures. The sac was excised in an open approach, whereas the sac was plicated with non-absorbable suture in thoracoscopic and laparoscopic repair (Figures 1 F, G). The excised sac was lined with flattened mesothelial cells with stromal hyalinisation and a few inflammatory infiltrates in the background of fibrocollagenous tissue (Figure 1 I).
None of our babies required mesh repair. Placement of an intercostal drainage tube was left to the surgeon’s decision. Five (11.6%) babies required post-operative intercostal drainage tube insertion for pneumothorax.
Statistical analysis
Gestational age in weeks, mode of delivery, birth weight in grams, age on admission, gender, the presence of cardiac malformations, primary pulmonary hypertension (PPHN), requirement for pre- and post-operative ventilation, weight at the time of surgery, modes of surgery and duration of the hospital stay among grouped subjects were assessed statistically. Continuous variables were reported using mean ± standard deviation and interquartile ranges. Frequencies and percentages were reported as categorical variables. The Student t test and χ2 test were used to evaluate their association. The statistical significance among groups was assessed by ANOVA or the Kruskal-Wallis test (Table I). SPSS software version 18.0 (IBM, New York; Routledge) was used for analysis.
Table I
Clinical profile of congenital diaphragmatic hernia with sac
Results
Forty-three children including neonates who had CDH with a sac were included in this study. 43/43 (100%) were subjected to surgical repair of the defect. Group I (GI) included left-sided congenital hernia defects with a sac and group II (GII) included right-sided congenital hernial defects with a sac. These groups were subclassified for ease of assessment as well as to determine the prognosis among the groups and to evaluate the statistical significance of differences among them.
Group I was subclassified into GIA for neonates from 0 to 30 days, GIB included 1 month to 1 year age and GIC included age more than 1 year; group II was subclassified similarly.
Mean age at presentation in group I (left CDHS) was 385.63 ±844 (median: 45, range: 1–2920) and 322.15 ±448.76 (median: 168, range: 2–1640) in GII and in the whole group it was 366 ±741.80.
In group I, 19 (44.18%) were male and 11 (25.58%) were female, with ratio of 2 : 1. Group II had 7 (16.27%) males and 6 (13.95%) females, with a ratio of 1 : 1. There was an overall preponderance of males (60%), having a ratio of 1.5 : 1. The majority of the babies were born by full term normal vaginal delivery, 25 (58.13%), with 17 (39.35%) having full term caesarean section delivery, with an overall ratio of 1.25 : 0.5.
Gestational age in weeks in GI was 37.96 ±0.18, in GII 37.69 ±1.18, and overall 37.88 ±0.6622.
There was only 1 (2.32%) preterm baby with right-sided CDH with a sac who did not require preoperative ventilator support, but required a post-operative ventilator for 23 days and subsequently was discharged uneventfully. Mean birth weight in GI was 2.65 ±0.18 kg (median: 2.6, range: 2.5–3.33), in GII 2.57 ±0.516 kg (median: 2.5, range: 1.6–3.75) (Table I). Mean weight at the time of surgery in GI was 6.01 ±5.83 kg (median: 3, range: 2.5-26), in GII 5.20 ±2.177 kg (median: 5, range: 2.25–9) (Table I).
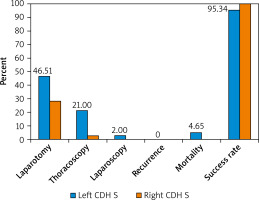
All 43 (100%) children underwent surgical intervention, 30 in the left CDH sac group and 13 (100%) in the right CDH sac group (GII). 32/43 (74.41%) babies underwent an open laparotomy approach for the repair of the CDH with sac; 9 (20.93%) in GIA, 10 (23.25%) in GIB and 1 (2.32%) in GIC. Overall, 13 (30.23%) in GII underwent surgical procedures. There were 5 (11.62%) neonates below 1 month in GIIA, 5 (11.62%) in GIIB, and 2 (6.97%) babies were more than 1 year in GIIC.
We had 9 (20.93%) neonates alone in GIA requiring open laparotomy with 3 (6.97%) neonates undergoing thoracoscopic repair; 1 (2.32%) underwent laparoscopic repair in GIC. Overall, 10 (14.28%) underwent thoracoscopic repair with one death (2.32%) in GIA.
Six (13.95%) neonates were on preoperative ventilation for an average of 3 days in GI due to PPHN and 2 babies in GII (7.31%). One baby required high frequency ventilation for 5 days and was subsequently weaned off. Four (9.30%) babies in GI in the study needed post-operative ventilation for an average of 4 days with uneventful recovery.
Overall, the duration of hospital stay in our study was 14 ±17.49; 16 ±20.28 days, with GI and in GII 11 ±5.019 days. One neonate who stayed in hospital for 4 months without a successful surgical outcome who underwent thoracoscopic repair died. In the whole study, there were 2 (4.65%) deaths: 1 (2.32%) baby in GIC after open laparotomy and 1 (2.32%) neonate in GIA died a few days after the thoracoscopic repair. Hence the success rate was 95.34% in GI and 100 % in GII. None of our babies included in the study required mesh repair. All were closed primarily without recurrence.
Discussion
The septum transversum of the mesoderm gives rise to the diaphragm. The medial ingrowth of the post-hepatic mesenchymal plate and pleuroperitoneal folds fails to fuse, resulting in the defect in the developing diaphragm causing herniation of viscera with the bowel into the thoracic cavity at around the 8th gestational week, hence compressing the developing lungs and causing their hypoplasia [1, 2]. The exact aetiology is not known. However, various genetic, environmental and nutritional factors have been proposed for CDH [1, 2].
Congenital diaphragmatic hernia can have a sac in around 14–20% of cases according to the literature. The sac, which is a non-muscularised pleura peritoneal fold, covers the herniated viscera in the thoracic cavity, hence protecting the developing lungs [1, 2]. Incomplete muscularisation of the hemidiaphragm results in congenital diaphragmatic eventration, with resultant weakened muscularised dysfunctional diaphragm, allowing the protrusion of abdominal contents into the thoracic cavity [1, 2].
Overall mortality of 30% to 50% has been reported due to CDH. Pulmonary hypertension and hypoplasia are the most common causes of mortality and morbidity. The beneficial effects of presence of the sac are due to its protective covering of the abdominal viscera, hence protecting the developing lungs.
The pleuroperitoneal fold, which is closed in both situations, as a weak hernial sac or with little muscularisation in the case of eventration, may be caused by different embryological events [1–4]. The antenatal detection rate of CDH varies from 10 to 70% according to the published literature, whereas in our cohort there were 6/43 (13.95%), which were detected at 32 to 35 weeks, just before delivery [1–4].
Four (9.30%) were in left-sided and 2 (4.65%) in right-sided CDH. None of our babies had a history of polyhydramnios. According to the literature, the antenatal detection rate of right-sided CDH is lower than that of left CDH [1, 2].
Respiratory distress immediately after birth, auscultation of bowel sounds in the chest and resultant mediastinal shift on chest radiography (Figures 1 A, B) are the most common presenting signs and symptoms of CDH. However, some cases can present with chronic respiratory issues such as recurrent bronchopneumonia. Cases of CDH with sacs have varied presentations; in our series, we had 18/43 (41.86%) presenting at neonatal age.
Since surgical intervention is the definitive treatment in CDH, it should be done only after cardiorespiratory function is stabilised. Gentle ventilation followed by surgery usually yields better results. On preoperative evaluation we found only 1 baby, 1/43 (2.32%), with an anterior ectopic anus (ARM), which was managed successfully by primary posterior sagittal anorectoplasty. Only 2 (4.65%) babies had cardiac anomalies, i.e. patent ductus arteriosus in GII and trivial tricuspid regurgitation in GI. None of our babies had lethal cyanotic heart disease or any associated syndromes. No lethal associated syndromes including cyanotic heart diseases were seen in any of our babies.
Contrast-enhanced chest tomography and upper gastrointestinal contrast study were used only rarely in doubtful cases. Thoracoscopic repairs result in minimal post-operative pain and hence hasten recovery [1–6].
Minimal access surgery such as thoracoscopic or laparoscopic plication of the defect was planned in stable babies. However, technically difficult cases or in medically unstable condition for a long time were converted to open procedures. The overall survival rate in our study was 95.34%. Though higher recurrence rates following the thoracoscopic approach have been documented in the literature, our study proves just the opposite (Figure 2) [2, 7–9].
Behaviour of the CDH with a sac is different when compared to classic CDH patients. Mortality rates of CDH have varied from 3 to 32% in the literature [1–5]. Ours was low, at 4.65% (Tables I and II, Figure 2).
Table II
Clinical profile of each group and subgroups
Since ours is a tertiary care, exclusively neonatal and paediatric centre in southern India, only referred cases are managed. The overall good birth weight of 2.63 ±0.3164 kg as well as surgical weight 5.73 ±5.522 kg in our study, neither of which was statistically significant, highlights the importance of early suspicion and early referral (Tables I and II).
CDH with a sac has been noted to have higher survival and early recovery rates [4, 5, 8].
According to Spaggiari et al., visible evidence of presence of a sac could suggest that this embryological event occurred late in the development, hence having a protective effect on developing lung buds [5]. Bagłaj stated that CDH cases presenting late may be associated with a hernial sac in up to 33% of cases. If existence of a sac is missed or goes undetected, it can lead to recurrence as well as prolonged morbidity and even mortality [8].
Gander et al. and Tiryaki et al. noted higher recurrence in the thoracoscopic approach [2, 9]. In our study, 18 (41.86%) were neonates presenting early to the NICU, and 9 (20.93%) presented after 1 year of age. In this study, we did not encounter any surgical site infections or recurrences, with exceptionally excellent survival rates. None of our babies had surgical site infections or recurrences, with excellent survival rates. In this study we had the highest number of neonates treated early with a good prognosis and right-sided CDH, and excellent prognosis without any mortality, managed in a tertiary care centre in southern India.
This study had certain limitations; e.g., antenatal ultrasonographic findings (lung head ratio, liver up, stomach up), initial oxygenation indices (OI) values and APGAR scores were not available in all records. It is because ours is the only tertiary care referral centre exclusively for children and neonates in southern India.
Conclusions
Mere awareness of the existence of such a rare entity as a ‘sac’, in association with congenital diaphragmatic hernia, by the attending clinician can greatly help reduce to morbidity.
Congenital diaphragmatic hernia with a sac is a rare embryological anomaly to diagnose clinically; however, such cases have excellent survival if referred early and hence managed early in a nearby neonatal and paediatric tertiary care centre.