Introduction
Acne vulgaris is a chronic, inflammatory skin condition affecting the sebaceous units of the skin. The pathogenesis of acne is multifactorial and involves follicular hyperkeratinization, colonization by Cutibacterium acnes, and sebum production. Additionally, neuroendocrine regulatory mechanisms, diet, as well as genetic and nongenetic factors, influence the development of acne lesions. Acne affects approximately 9% of the global population, primarily teenagers and young adults, but it can persist into late adulthood. The presence of skin lesions, mainly on the face and trunk, negatively impacts individuals’ mental health and is associated with lower self-esteem. Although acne is not a life-threatening condition, it is linked to increased anxiety, depression, and even suicidal ideation. Untreated acne lesions can result in permanent scarring. Therefore, appropriate therapy is essential [1].
Conventional acne treatments have limitations and potential adverse effects. Oral antibiotics’ effectiveness is diminished by increasing microbial resistance, observed particularly in case of erythromycin and oxytetracycline. Adverse reactions may include photosensitivity and gastrointestinal impairment. Topical retinoids can cause dry, irritated, and peeling skin and systemic ones can lead to side effects such as epistaxis, headaches, hyperlipidaemia, hepatotoxicity, and teratogenicity. Consequently, there is a significant need for alternative treatment approaches for moderate to severe acne vulgaris [2].
Photodynamic therapy (PDT) offers a non-invasive alternative treatment for acne treatment and is considered by the American Academy of Dermatology as one of the most promising light-based methods [2]. This treatment modality entails the application of a photosensitizing agent, such as aminolevulinic acid (ALA), to the affected areas of the skin. After a designated period allowing absorption by the sebaceous glands and metabolism into protoporphyrin IX (PpIX), targeted irradiation with a specific wavelength of light is administered. This illumination activates the photosensitizer, thereby instigating the production of reactive oxygen species (ROS), which in turn activates the immune system through various mechanisms, leading to apoptotic as well as non-apoptotic cell death pathways [3–5]. One notable mechanism involves the selective destruction of pilosebaceous units. This was proved by Hongcharu et al. [6] who compered the histological examination of skin biopsy before and at the end of ALA-PDT treatment, which showed complete destruction or 45% decrease in size of sebaceous glands. Another possible model of action is destroying C. acnes which sterilizes the sebaceous follicle. Pollock et al. failed to prove this conception, although they have reported a statistically significant clinical improvement in patients [7]. More studies have been conducted to prove the antimicrobial effect, but no significant reduction of C. acnes in skin biopsy has been described [8]. The third pathway of ALA-PDT effect is a reduction of follicular obstruction [9]. Whilst there is considerable evidence supporting the efficacy of PDT, further research is required to determine the optimal photosensitizer, incubation time, and light source for incorporating PDT into standard recommendations.
Aim
This study aimed to optimize PDT parameters for the treatment of acne and confirm the method’s efficacy. To achieve this goal we conducted a prospective, split-face study involving 25 patients to compare different concentrations of ALA used in PDT.
Material and methods
This study was conducted from October 2022 to February 2023 as a randomized, double-blinded, split-face study. This study was approved by the Bioethics Committee for Scientific Research at the Medical University of Gdansk. All participants provided written informed consent. Thirty-three participants (5 men and 28 women, age range: 18–27 years) with mild to severe acne on their face (Leeds grades 2–4) were recruited and screened for eligibility at the Department of Dermatology, Venereology and Allergology at the Medical University of Gdansk. Participants were excluded if they were under 18 years old, pregnant or breastfeeding, had used topical antibiotics or topical retinoids in the previous 4 weeks, had used isotretinoin in the last 6 months, had used oral antibiotics or photosensitizers 30 days prior to enrolment. Participants who had face affecting cutaneous disease (in spite of acne vulgaris), a history of photosensitivity disorders, diabetes or severe lung, renal, heart and liver diseases were also excluded. A total of thirty-three subjects were recruited, of which twenty-five met the inclusion criteria to form the study group. Subjects’ details are summarized in Table 1. Each patient was carefully assessed in terms of the number of acne lesions (at least 10) and severity of acne vulgaris [10]. The acne lesion-counting technique was used as it is an accurate method of counting which considers both inflammatory and noninflammatory lesions and is applicable to all skin tones [11]. The face was divided into five regions. In each region, the number of open and closed comedones, papules, pustules, and nodules were counted. The severity of acne was rated according to the Investigator Global Assessment (IGA) of acne, which was accepted by the American Food and Drug Administration (FDA) in 2018 [12]. Patients with a score of 3–5 were enrolled to the study, corresponding to varying degrees of acne severity, from mild to severe. Photographs were taken before the treatment was launched. Patients were randomly divided into two groups with different acid concentration: 10% ALA or 15% ALA using a computer-based block randomization (Sealed Envelope). In both groups ALA concentration was applied to the left cheek, while a placebo was applied to the right one. Neither the patients nor the investigator knew the ALA concentration.
Table 1
Demographic data of the subjects
Study design
The study was conducted over 5 months and consisted of an initial visit, three ALA-PDT sessions with 7–10 days’ intervals and follow-up visit at 4 and 8 weeks after the last session.
The ALA agents (10% and 15%) used in this study were prepared by dissolving ALA hydrochloride powder (MagnaPharm Poland sp. z o. o.) in a cream formulation obtaining the modality containing: Aqua, Petrolatum, Aminolevulinic Acid HCl, Cetearyl Alcohol, Paraffin, Lanolin, PEG-100 Stearate, Glyceryl Stearate, Glycerine, Canola Oil, Disodium EDTA, Isostearyl Isostearate, Hydrogenated Coco-Glycerides, Dicaprylyl Carbonate, Glyceryl Stearates, Panthenol, Helianthus Annuus Seed Oil, Zea Mays Oil, Sesamum Indicum Seed Oil, Macadamia Integrifolia Seed Oil, Olea Europaea Fruit Oil, Tocopheryl Acetate, Allantoin, Melaleuca Alternifolia Leaf Oil, PEG-8, Tocopherol, Ascorbyl Palmitate, Ascorbic Acid, Citric Acid, BHT, Phenoxyethanol, Ethylhexylglycerin, and Limonene. Participants had acne lesions counted and documented by taking photographs before each treatment. Each patient had their face thoroughly cleaned with gel cleanser (containing Glycerine, Sodium Lauroyl, Cocamidopropyl hydroxysultaine and Ceramides). ALA gel was applied on the left side of the face and placebo (containing Aqua, Petrolatum, Cetearyl Alcohol, Paraffin, Lanolin, PEG-100 Stearate, Glyceryl Stearate, Glycerine, Canola Oil, Disodium EDTA, Isostearyl Isostearate, Hydrogenated Coco-Glycerides, Dicaprylyl Carbonate, Glyceryl Stearates, Panthenol, Helianthus Annuus Seed Oil, Zea Mays Oil, Sesamum Indicum Seed Oil, Macadamia Integrifolia Seed Oil, Olea Europaea Fruit Oil, Tocopheryl Acetate, Allantoin, Melaleuca Alternifolia Leaf Oil, PEG-8, Tocopherol, Ascorbyl Palmitate, Ascorbic Acid, Citric Acid, BHT, Phenoxyethanol, Ethylhexylglycerin, Limonene) was applied to the right side of the face. Face was covered with plastic, non-transparent, occlusive foil, for 1.5 h. Red light emitted from the LED lamp (wavelength, 633 ±10 nm) at a light dose of 96 J/cm2, irradiated the whole face of each participant for 8 min from the distance of 8–10 cm. Eyes were covered with protective glasses. Participants were treated in the afternoon sessions and instructed to avoid sun exposure afterwards and apply sunscreen (min. SPF 50) in the following 10 days.
Lesion counts and analysis
All types of acne lesions (comedones, papules, pustules, nodules and cysts) were counted at baseline, before each treatment, 4 and 8 weeks after the last PDT treatment. The treatment group allocation was blinded to the counting operator.
Statistical analysis
An analysis was performed using Shapiro-Wilk normality tests which showed that the distribution of the acne lesions followed a normal distribution in both study groups. Student t test was used to compare the difference in the acne reduction number between two groups. A p-value of less than 0.05 was considered statistically significant.
Results
Twenty-five eligible participants were enrolled in the study and twenty-two completed the study. After the first session two participants withdrew from the study due to moderate erythema, while another one experienced eye pain. All side effects resolved spontaneously. Following this, the examination proceeded with the remaining 22 participants. The initial analysis aimed to assess the effects of ALA-PDT on inflammatory acne lesions compared to placebo (simple red light treatment). For patients treated with 10% ALA, the median reduction rate in inflammatory acne lesions was 27.36% (SD = 17.85), while for the placebo side, it was 12.64% (SD = 13.17). Similarly, with a 15% ALA concentration, the median reduction was 40.45% (SD = 11.07), whereas the placebo side showed a reduction of 13.41% (SD = 5.03). Significant differences were observed with both 10% ALA (p = 0.04) and 15% ALA treatment (p < 0.01). Notably, both groups exhibited a more pronounced reduction in acne lesions on the ALA treatment side, with greater disparities observed for the 15% ALA concentration.
In contrast, ALA-PDT treatment of non-inflammatory acne lesions indicated no statistically significant difference (p > 0.05) in the percentage reduction between the placebo side and the treatment side. For patients treated with 10% ALA, the reduction in non-inflammatory acne lesions was 12% (SD = 10.12), and for placebo it was 11.27% (SD = 11.79). For those treated with 15% ALA, the reduction was 11.27% (SD = 11.79), while for placebo it was 9.91% (SD = 6.94). The results of this analysis are presented in Tables 2 and 3.
Table 2
Results of Student’s t-test analyses for independent samples for comparison of percentage of inflammatory acne lesion reduction between treated and placebo sides in patient groups
| Inflammatory | M | SD | t | p | d |
|---|---|---|---|---|---|
| 10% ALA | 27.36 | 17.85 | 2.20 | 0.040 | 0.94 |
| Placebo | 12.64 | 13.17 | |||
| 15% ALA | 40.45 | 11.07 | 7.38 | < 0.01 | 3.14 |
| Placebo | 13.41 | 5.03 |
Table 3
Results of Student’s t-test analyses for independent samples for comparison of percentage of non-inflammatory acne lesion reduction between treated and placebo sides in patient groups
| Non-inflammatory | M | SD | t | p | d |
|---|---|---|---|---|---|
| 10% ALA | 12.00 | 10.12 | 0.16 | 0.878 | 0.07 |
| Placebo | 11.27 | 11.79 | |||
| 15% ALA | 11.27 | 11.79 | 0.33 | 0.745 | 0.14 |
| Placebo | 9.91 | 6.94 |
Furthermore, results indicated no statistically significant difference between 10% and 15% ALA in the percentage reduction of both inflammatory (p = 0.052) and non-inflammatory (p = 0.878) acne treatment. Detailed findings are presented in Tables 4 and 5. Figure 1 presents a summary of the findings in graphical form. Representative clinical photographs showing acne improvement are shown in Figures 2 and 3.Treatment tolerance
Table 4
Results of Student’s t-test analyses for independent samples for comparison of percentage of inflammatory acne lesion reduction between 10% ALA and 15% ALA groups
| Inflammatory | M | SD | t | p | d | |
|---|---|---|---|---|---|---|
| Placebo | 10% ALA | 12.64 | 13.17 | 0.18 | 0.858 | 0.08 |
| 15% ALA | 13.41 | 5.03 | ||||
| ALA | 10% ALA | 27.36 | 17.85 | 2.07 | 0.052 | 0.88 |
| 15% ALA | 40.45 | 11.07 | ||||
Table 5
Results of Student’s t-test analyses for independent samples for comparison of percentage of non-inflammatory acne lesion reduction between 10% ALA and 15% ALA groups
| Non-inflammatory | M | SD | t | p | d | |
|---|---|---|---|---|---|---|
| Placebo | 10% ALA | 4.91 | 4.18 | 2.05 | 0.057 | 0.87 |
| 15% ALA | 9.91 | 6.94 | ||||
| ALA | 10% ALA | 12.00 | 10.12 | 0.16 | 0.878 | 0.07 |
| 15% ALA | 11.27 | 11.79 | ||||
Figure 1
Difference in percentage reduction of inflammatory and non-inflammatory acne lesions in patients treated with 10% and 15% concentration of aminolevulinic acid (ALA)
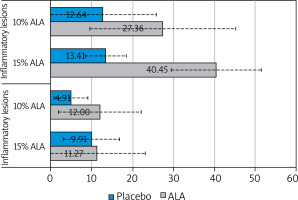
Figure 2
Improvement of acne lesions. Clinical images depict the forehead of a female patient from (A) baseline to (B) 8-week follow-up after the third treatment. The patient received treatment with 15% ALA-PDT on the left side of the face and single red light therapy on the right side
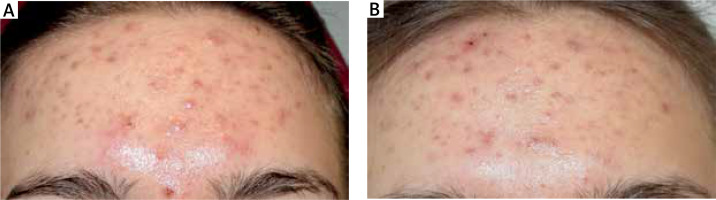
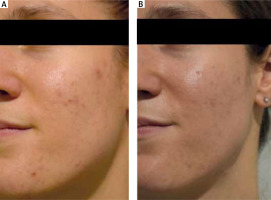
Figure 3
Improvement of acne lesions. Clinical image of a female patient from (A) baseline to (B) 8-week follow-up after the third treatment. The patient received treatment with 15% ALA-PDT on the left side of the face and single red light therapy on the right side
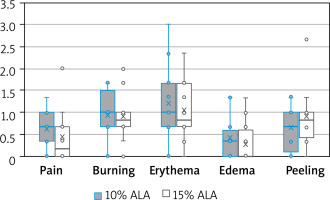
All side effects were subjectively rated by participants using a numeric scale ranging from 0 to 3. A score of 0 indicated no side effects, while a score of 3 indicated a severe side effect, affecting normal daily activities or sleep. Five side effects: pain, burning, erythema, oedema, and peeling were evaluated by the patients. The average side effect scores after each treatment are presented in Table 6.
Table 6
The average side effect scores rated in a numeric scale after each treatment both in 10% and 15% ALA groups
[i] 0 – the side effect does not occur, 1 – mild (the side effect occurs, but is not disruptive), 2 – moderate (the side effect is noticeable and somewhat bothersome, but does not interfere with normal daily activity or sleep), 3 – severe (the side effect is pronounced and significantly interferes with normal daily activities or disrupts sleep).
With the exception of peeling, all reactions were most intensive 24 h after treatment. Skin exfoliation, on the other hand, occurred on the 4th and 5th days after PDT. Comparisons between groups in terms of the severity of side effects of ALA treatment were made using Student’s t-test for independent samples. No significant differences in side effects were observed between the two groups (10% and 15% ALA), which means that the distribution of side effect severity followed a normal distribution in both groups of subjects. Of the side effects, respondents rated the occurrence of erythema highest (1.19 points in the 10% ALA group and 1.06 points in the 15% ALA group), followed by a burning sensation (0.92 points in the 10% ALA group and 0.89 points in the 15% ALA group), peeling (0.64 points in the 10% ALA group and 0.89 points in the 15% ALA group), pain (0.61 points in the 10% ALA group and 0.44 points in the 15% ALA group) and the lowest – swelling (0.42 points in the 10% ALA group and 0.28 points in the 15% ALA group). The summarized findings are presented in Figure 4 and Table 7. We observed that the side effects were dependent on the participants’ skin phototype. Six out of 25 participants had Fitzpatrick skin types IV or V, and did not report any side effects. In contrast, all participants with Fitzpatrick skin type I noticed erythema, tingling, and pain, with some rating them as severe (3/3) on our numeric scale. One patient with Fitzpatrick skin type IV exhibited mild hyperpigmentation, which resolved by the follow-up visit that was conducted 4 weeks after treatment.
Table 7
Results of Student’s t test analyses for independent samples for comparison of side effects between patient groups
Figure 4
Assessment of side effects in patients treated with 10% and 15% concentrations of ALA: the box plot visually presents key statistical measures. The median value, denoted by a line inside the box, represents the midpoint of the data. The box itself illustrates the interquartile range, encapsulating the central 50% of the data. Whiskers extend to indicate the full range of the data, excluding outliers. An ‘X’ marker signifies the mean value of percentage of acne lesion reduction
Discussion
Photodynamic therapy paired with aminolevulinic acid is a promising method of treatment of acne vulgaris, due to its fast and long-lasting clinical effect and low risk of generating bacterial resistance [6, 13]. According to the latest European Dermatology Forum guidelines on topical photodynamic therapy, PDT may emerge as an alternative to conventional treatment for inflammatory acne of moderate severity (Strength of Recommendation B, Quality of Evidence I) [14].
Therapy protocols (including type and concentration of the photosensitizer, incubation time, light source, and irradiation time) are yet to be standardized [14]. Various types of photosensitizers and several concentrations have been studied in PDT for treatment of acne to help standardize the protocols. Our goal was to identify an effective medication while minimizing adverse reactions. Literature reviews show that photodynamic therapy can be also paired with ester derivatives of ALA, such as methyl aminolevulinate (MAL). According to the current knowledge, MAL used with high-dose conditions (long incubation time, high fluence red light exposure) showed similar effects to ALA-PDT for acne treatment [13]. Hongcharu et al. first reported this type of therapy as a possible therapy for acne patients. The study investigated the impact of PDT therapy followed by red light emission on acne vulgaris located on the back. Topical 20% ALA was applied with 3-hour occlusion, the area was irradiated with 550–700 nm light. Half of the participants received one session, while the other half underwent four sessions. Significant improvement in the PDT-treated area was observed. Patients who received four PDT treatment sessions showed 50% reduction of acne, while one PDT treatment session resulted in 30% reduction of acne. Histological examination revealed a significant decrease in follicular bacteria and sebum rate. Clinical improvement was closely correlated with sebum production suppression [6]. Zhang et al. conducted a study comparing the effectiveness of acne lesion reduction using 5% and 10% ALA PDT. A greater decrease in inflammatory lesions was observed with a higher ALA concentration, with no significant difference in pain scores between groups [15]. To our knowledge, a study comparing 10% and 15% ALA-PDT in acne treatment has not been conducted yet. This is the first study to assess the efficacy and safety of 10% ALA compared with 15% ALA PDT for acne vulgaris.
Despite choosing the optimal type and concentration of the photosensitizer, an adequate light source is necessary to produce therapeutic effect in case of ALA-PDT. ALA has a maximum absorption band in the blue light spectrum (405–415 nm), but this wavelength poorly penetrates the dermis. Weaker absorption bands are located in the green (506–540 nm), yellow (572–582 nm) and red spectra (628–635 nm) [13]. Studies suggest that red light sources yield the best long-term results due to deep penetration through skin layers and the highest porphyrin absorption [16]. Although a study by Zhang et al. indicates that intensive pulsed light (IPL) may be associated with fewer adverse reactions, we have decided to choose the red light emission as more studies have been conducted using red light illumination and is known for better efficiency through more effective photobleaching of protoporphyrin IX [17].
Determining precise conclusions regarding fluence rates and energy density presents a significant challenge due to variations between light-emitting devices, lesion types, and differences in the distance between the light source and the target area [18]. In clinical trials, the energy density of the typical red light source typically ranges from 60 to 200 J/cm2 [19]. In our study, this parameter was set at 96 J/cm2, reflecting the specifications of the light device employed. However, refining the ideal treatment parameters is an ongoing process with continuous efforts focused on investigation and optimization.
In our study, we observed a rapid and significant reduction in inflammatory acne lesions using ALA-PDT compared to simple red light therapy. However, ALA-PDT was less effective for non-inflammatory lesions, with results comparable to those of single red light treatment. Our findings align with those of other researchers [16, 20]. The reason for the lower efficacy in treating comedonal acne remains unclear, but researchers speculate that inflammatory lesions may absorb the photosensitizer and light more efficiently than non-inflammatory lesions [20].
PDT has been safely used in all skin types including Fitzpatrick skin types I–VI [21, 22]. However, it is important to acknowledge that PDT is not without adverse reactions, including pain, erythema, and oedema, typically occurring in the days immediately following treatment. We speculate that adverse effects tend to be more pronounced in individuals with a lower Fitzpatrick skin phototype. In such cases, careful consideration should be given to adjusting the ALA concentration, especially in patients who are more sensitive. To decrease pain associated with ALA-PDT, researchers recommend use of cold air, brief pauses during illumination, intralesional lidocaine injection or topical anesthetics prior to treatment [23]. Another side effect of this therapy is occurrence of hyperpigmentation. According to the previous studies on ALA-PDT acne management, hyperpigmentation was more frequent in dark skin patients and those who have undergone treatment with a higher light dose [8]. In our study only one person experienced hyperpigmentation due to the therapy, for which we are unable to find a plausible explanation.
Although the study was designed to be as much unified as it is possible, confounding variables were interpersonal differences between participants, such as skin type, life style and a level of adherence to the recommendations after therapy. Other limitations of this study included a relatively low number of participants. Further studies are needed to be conducted on a larger sample.
In our perspective, the choice of ALA concentration should be tailored to the patient’s skin phototype, skin sensitivity and acne severity. To establish these recommendations and strengthen the evidence base, further research is needed. In conclusion, numerous studies have consistently demonstrated that ALA-PDT therapy can lead to significant improvements in the skin condition of acne patients, making it a viable choice in broad spectrum of acne treatment options.








