Introduction
During thoracic surgery blood flow disorders of the peripheral and cerebral vasculature may occur. These procedures include interventions within the pulmonary parenchyma, mediastinum, esophagus, and large venous and arterial vessels. Procedures within the thorax often involve one-lung ventilation (OLV). Due to the anatomical asymmetry of the respiratory system, the volume of ventilated lung tissue varies [1]. Consequently, it is necessary to monitor patients’ intraoperative blood oxygenation. However, measurement of peripheral blood saturation (SpO2) as a single parameter does not allow for accurate assessment of the central nervous system oxygenation. In addition, changes in the blood pressure in the chest area directly affect the oxygenation of the brain. Therefore, it should be remembered that potentially any thoracic surgery interferes with blood flow within the brain. Determining brain oxygenation (BO) can be a method for objective complementation of SpO2. Until recently, methods of cerebral blood oxygenation evaluation included direct brain tissue oxygenation (PtO2 – brain tissue oxygen tension) and blood saturation from the internal jugular vein (SjvO2 – jugular venous oxygenation) [2]. The main disadvantage of these methods is their invasive nature and number of hemodynamic, neurological, and septic complications. On the other hand, BO is a non-invasive method based on near-infrared spectroscopy (NIRS) which is an optic way of measuring brain tissue oxygenation. NIRS can also be applied to measure oxygenation of other internal organs, which is used in neonatology [3]. NIRS evaluates saturation in microcirculation, where arterial blood is mixed with venous blood, reflecting the difference between supply and demand for oxygen. Brain blood oxygenation depends on cerebral blood flow, cardiac output, hemoglobin concentration, global respiratory capacity, oxygen concentration in respiratory mixture, brain temperature and tissue metabolism, as well as the symmetry of blood supply to tissues. Thus, effects on the measurements will include factors such as past ischemic stroke, internal carotid artery stenosis, cerebral blood flow disorders but also intraoperative vessel manipulation. Monitoring brain oxygenation during surgery is helpful in estimating the risk of neurological complications such as stroke, seizures, and post-operative cognitive behavioral disorders in patients initially exposed to such risks. During cardiac, thoracic, neurological, and other surgical procedures requiring cannulation of large peripheral arteries, a decrease in cerebral oximetry may indicate vascular bridge insufficiency, abnormal cannula position or arterial blood flow disturbance due to air embolism [4].
Aim
The aim of this study is to compare SpO2 with BO measurements and evaluate the utility of BO in thoracic surgery.
Material and methods
The present study was performed at the Department of Thoracic Surgery and Transplantation of Pomeranian Medical University in Szczecin between 18.10.2010 and 13.12.2011. A FORE-SIGHT Casmed (USA) device was used to measure BO and the sensors were placed in the forehead region. Spacelabs Medical (model 91387) device was used to measure SpO2. The sensor was placed on the index finger of the hand on the operated side of the patient. During premedication, patients received standard doses of anesthetic drugs. Induction of anesthesia was performed using intravenous propofol, thiopental or etomidate, and fentanyl. Administered relaxants included rocuronium, vecuronium and succinylcholine. Sevoflurane was applied to maintain anesthesia. The patients were placed on the left or right side depending on surgical access. None of the operated patients required blood transfusions during surgery. Standard monitoring procedures were applied, including three-lead electrocardiogram, non-invasive blood pressure, SpO2, and experimental BO measurements. BO and SpO2 assessments were made every 15 minutes. Operation time was defined as the period from tracheal intubation to extubation. Tested parameters were evaluated in the context of duration of surgery, operated side, extent of surgery, sex, and age.
Statistical analysis
Was performed using Statistica software (version 10). Spearman’s rank correlation coefficient was used to analyze relationships between SpO2 and BO values at the specific time points and their variability over time with relation to age and duration of surgery. The Mann-Whitney U test was applied to compare subgroups of patients stratified according to operated side and type of surgery. This study was based on reviewing medical documentation of intraoperative monitoring of the peripheral blood saturation and cerebral oxygenation without any additional interventions. Therefore, it was exempt from obtaining approval from the ethics committee.
Results
Patients
This study involved 100 consecutive patients undergoing thoracic surgery. Baseline and intraoperative characteristics are presented in Table I. The youngest operated patient was 20 years old and the oldest 85 years old. The mean age was 61.24 ±11.63 years, and the median was 62 years. We found a negative correlation between the patient’s age and BO at the beginning of surgery (p = 0.04). This relationship was not observed at other time points and no correlation with age was found in the case of SpO2 values. Initial BO values were lower in older patients and the baseline SpO2 values were independent of the patient’s age. The study group was composed of 37 women and 63 men – 37% and 63%, respectively. A statistically significant difference was found between SpO2 at 15 minutes of surgery and sex of the patient (p = 0.012). No differences were found for other time points and BO values (Table II). Due to the lack of physiological bases for this result, it should be assumed that this association is random. Performed operations included 38 segmentectomies, 40 lobectomies and 10 pneumonectomies. Sixty operations involved the right lung and 39 operations concerned the left lung. Mediastinoscopy was performed in one patient.
Table I
Baseline and intraoperative characteristics of the study group
Table II
Comparison of SpO2 and BO values in terms of patient’s sex
[i] BO – brain oxygenation, BO Dec – decrease in brain oxygenation, BO Min – minimum brain oxygenation, BO Mean – mean value of brain oxygenation, SpO2 – peripheral blood saturation, SpO2 Dec – decrease in blood saturation value, SpO2 Min – minimum blood saturation, SpO2 Mean – mean value of blood saturation.
Duration of surgery
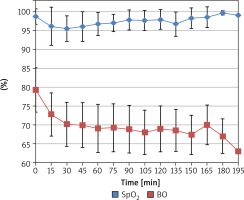
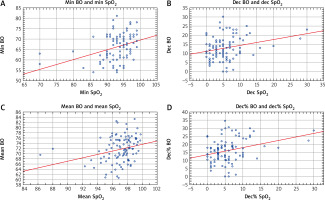
The mean duration of surgery was 91.45 minutes (range: 30–200; median: 87.5 ±37.94 min). Twenty operations lasted longer than 120 minutes. Both SpO2 and BO, measured from 45 to 105 minutes, showed statistically a significant negative correlation with overall duration of surgery (Table III). Longer surgery was associated with a greater decrease in SpO2 and BO values. This relationship was not detected at other time points. Furthermore, we observed that a decrease in BO correlated positively with overall duration of surgery (p = 0.01). In other words, BO decreased the longer surgery lasted. Mean BO value correlated negatively with overall duration of surgery (p = 0.0004). A fast recovery of SpO2 to baseline values was observed, unlike for BO (Figure 1). There was a statistically significant positive correlation between SpO2 and BO between 15 and 90 minutes (Table IV). After 90 minutes a negative correlation was observed, which means that after 90 minutes SpO2 stopped reflecting brain oxygenation. Other correlations were found between minimum, mean, and decrease in SpO2 and BO (Figure 2). From the 105th minute of surgery, sample size decreased significantly. Only one operation lasted longer than 195 minutes.
Table III
Correlation of SpO2 and BO values with overall duration of surgery
Table IV
Spearman rank correlation for SpO2 and BO measured at specific time points
Figure 2
Spearman correlations of BO and SpO2
BO – brain oxygenation, BO Dec – decrease in brain oxygenation, BO Min – minimum brain oxygenation, BO Mean – mean value of brain oxygenation, SpO2 – peripheral blood saturation, SpO2 Dec – decrease in peripheral blood saturation value, SpO2 Min – minimum peripheral blood saturation, SpO2 Mean – mean value of peripheral blood saturation.
Left-sided vs right-sided thoracotomy
Operations involved 60 procedures on the right side and 39 on the left side. The difference between measurements of minimal SpO2 values measured during right- or left-sided surgery was statistically significant (p = 0.02). In patients with left-sided surgery, there were higher minimum SpO2 values (93.97%) compared to patients who had surgery on the right side (92.4%). No correlation was found between SpO2 and BO measurements at individual time points during surgery. A statistically significant difference between BO value and operated left or right side (p = 0.02) was found only at the 135th minute of surgery, which seems to be a random result. At this timepoint, a higher BO was measured in patients operated on the right side than on the left side (70.1% and 63.25% respectively, Table V).
Table V
Comparison of SpO2 and BO values using Mann-Whitney U test in terms of patient’s operated side
Extent of surgery
Thirty-eight wedge resections, 40 lobectomies, 10 pneumonectomies, and 12 other thoracic operations, including video-assisted thoracoscopic surgery (VATS), were performed in the study group. The relationships of the types of surgical intervention (wedge resection, lobectomy, pneumonectomy) with SpO2 and BO were analyzed and are presented in Tables VI–VIII. Compared to lobectomy, SpO2 values were significantly higher in patients undergoing wedge resections at 45, 60 and 90 minutes (p = 0.005, p = 0.002 and p = 0.03 respectively). We observed no differences in BO values between wedge resections and lobectomies at any time points. However, the BO decrease was significantly higher in lobectomy patients (p = 0.01). Furthermore, overall mean BO was lower during lobectomies compared to wedge resection procedures (p = 0.03).
Table VI
Differences in SpO2 measurements at different time points, depending on the type of surgery (wedge resection versus lobectomy)
Table VII
Differences in SpO2 and BO measurements at different time points, depending on the type of surgery (wedge resection versus pneumonectomy)
Table VIII
Differences in SpO2 and BO measurements at different time points, depending on the type of surgery (lobectomy versus pneumonectomy)
SpO2 values were significantly higher in patients undergoing pneumonectomy compared to wedge resection at 15 and 30 minutes (p = 0.02 and p = 0.04 respectively). Furthermore, in the pneumonectomy group, minimum SpO2 values were higher and the SpO2 decrease smaller, as compared to the wedge resection group (p = 0.02 and p = 0.01 respectively). There were no differences in BO measurements between these surgery types.
After comparing lobectomy with pneumonectomy, we found that SpO2 values were higher in the latter group at 45, 60, 75 and 105 minutes (p = 0.003, p = 0.001, p = 0.004 and p = 0.006, respectively). Moreover, minimum and mean SpO2 values were higher in the pneumonectomy group (p = 0.008 and p = 0.002 respectively). Additionally, BO values were higher in the pneumonectomy group at several time points (15, 45, 60, 75 and 90 minutes). Minimum and mean BO values were also significantly elevated (p = 0.02 each). Tables IX–XI present different saturation and oxygenation values between aforementioned procedures with the group of patients undergoing other thoracic procedures. There were no statistically significant differences when comparing wedge resection and lobectomy groups with the other cohort. In contrast, after comparing pneumonectomy with other procedures, the former was associated with higher saturation at 45, 60, and 75 minutes. Furthermore, mean blood saturation was higher in this group (p = 0.01).
Table IX
Differences in SpO2 and BO measurements at different time points, depending on the type of surgery (wedge resection versus other)
Table X
Differences in SpO2 and BO measurements at different time points, depending on the type of surgery (lobectomy versus other)
Table XI
Differences in SpO2 and BO measurements at different time points, depending on the type of surgery (pneumonectomy versus other)
Discussion
In the present study, we compared the use of BO and SpO2 as basic intraoperative parameters in thoracic surgery. The values of both parameters have been found to decrease during surgery. Furthermore, BO was found to be a more sensitive method of monitoring blood oxygenation. During surgery, the mean decrease in values between maximum and minimum measurements was 5.67% for SpO2 and 12.96% for BO. In addition, it should be noted that both SpO2 and BO values from 45 to 105 minutes are negatively correlated with overall duration of surgery. SpO2 values return to near-baseline values while BO continues to decrease with surgery after 90 minutes. Thus, SpO2 and BO values are not identical. SpO2 values within normal ranges do not exclude central nervous system hypoxia. Older patients presented lower BO values at the beginning of the surgery. This is probably related to the physiological changes that occur in the elderly, together with a greater number of vascular diseases occurring in older people. SpO2 showed no relationship with age, which may lead to underestimation of the risk of complications during further hospitalization. No relationship between BO and sex of the patients was found. Higher values of SpO2 were observed at 15 minutes of surgery in men.
Several risk factors are associated with cerebral desaturation during thoracic surgery, such as OLV, lateral decubitus position and hypoxic pulmonary vasoconstriction [5]. OLV used during thoracic surgery causes specific ventilation-dependent oxygenation disorders. Left lung operations result in higher minimum SpO2 values compared to the right side as perfusion distribution is heterogenous throughout the lungs and is slightly increased in the right lung [6]. Excluding smaller lung from ventilation results in fewer blood oxygenation disorders. On the other hand, BO values did not show a correlation with operated side. Nevertheless, Roberts et al. found that OLV in thoracic surgery is associated with frequent cerebral desaturations. Out of 117 patients, 60 developed cerebral oxygenation values below 65% for at least 3 minutes. Desaturations were correlated with postoperative delirium and prolonged the length of hospital stay [7]. In our study, cerebral desaturations below 70% were observed between 45 and 195 minutes of surgery. According to a study by Kazan et al., 56% of the patients undergoing thoracic procedures experienced at least a 20% decrease in cerebral oxygenation [8]. Hemmerling et al. reviewed BO of 20 patients undergoing thoracic surgery. The baseline BO value was 80% and the minimum was 63%. BO decrease was not correlated with other clinical parameters, such as blood loss, peripheral oxygen saturation, or PaO2 [9]. In the conducted study, the mean minimal BO value was 66.3% while BO and SpO2 decreases were positively correlated (p = 0.02). However, we found that SpO2 stopped reflecting brain oxygenation after 90 minutes of the procedure. Different vasoactive drugs may be administered to maintain high cerebral oxygenation. Choi et al., in a randomized clinical trial, analyzed the use of dopamine and phenylephrine in patients undergoing thoracic surgery. The authors found that use of dopamine was associated with increased mean BO values compared to the phenylephrine group (72 vs. 66, p = 0.01). In addition, 0 out of 25 patients experienced a BO decrease of more than 20%, as compared to 6 out of 19 in the phenylephrine group [10]. Type of anesthesia also affects cerebral oxygenation. Akdogan et al. found that the use of intravenous propofol was correlated with increased risk of BO decrease over 20% as compared to inhalation with sevoflurane (50% vs. 33%, p < 0.05) in patients undergoing thoracic surgery (lobectomies, chest wall resections, pneumonectomies) [11]. However, Sato et al. in a randomized clinical trial noted that propofol and desflurane induced similar alterations in BO during one-lung ventilation [12].
Nevertheless, reports of BO measurements in thoracic surgery are less common than other surgical fields, such as cardiac surgery. A large multicenter study by Raghunathan et al., involving 1.19 million patients, revealed that intraoperative use of cerebral oximetry is associated with decreased major organ mortality and morbidity in patients undergoing cardiac surgery [13]. Additionally, a common complication associated with a decrease in BO is postoperative cognitive impairment. A meta-analysis of studies describing BO measurements in abdominal, orthopedic, cardiac, spinal, and vascular surgery showed that intraoperative monitoring of cerebral oximetry was related to decreased rates of postoperative cognitive dysfunction [14]. Another recent study from a cardiac surgery department revealed that NIRS-based BO monitoring was associated with better 6-month postoperative functionality and shorter stay in the intensive care unit. Nevertheless, there was no difference in cognitive dysfunction, stroke, renal dysfunction, or multi-organ failure [15].
Assessment of BO and SpO2 values showed a statistically significant benefit in the case of a wedge resection compared to the lobectomy. SpO2 values were higher in the wedge resection group at 45, 60 and 90 minutes of surgery. Furthermore, we observed higher mean and smaller BO decrease during surgery in patients undergoing wedge resections. On the other hand, pneumonectomy, a more radical approach, showed better SpO2 than wedge resections and higher SpO2 and BO than lobectomies. Nevertheless, it should be noted that a much stricter selection process applies to patients undergoing whole lung resections than smaller procedures. In other words, patients with more comorbidities or with less cardiopulmonary reserve can undergo wedge resections but would be not suitable for a pneumonectomy. In addition, out of 10 pneumonectomies included in this study, only 1 (10%) lasted for 135 minutes. In contrast, out of 40 lobectomies, the duration of 15 (37.5%) of them was equal to or exceeded 135 minutes. Therefore, the potential period of hypoxia was also shorter in the pneumonectomy group.
Moreover, NIRS can be applied in fields other than intraoperative monitoring of cerebral oxygenation. For instance, it can be used to monitor the autoregulation of cerebral oxygenation in patients with a generalized inflammatory response. In the study by Steiner et al., the authors showed that slow blood flow in the transcranial Doppler test correlated with low brain oxygenation values determined by NIRS. Due to the dynamic autoregulation of the blood flow and mean arterial pressure (MAP) within the skull, intracranial pressure can be estimated, which is significant during extensive surgical procedures and intensive care [16]. Furthermore, in the field of emergency medicine, the sensor may be placed on the limb or neck to monitor regional tissue oxygenation to help identify or monitor shock patients [17, 18]. Additionally, it was found that higher BO values correlate with the return of spontaneous circulation during resuscitation in patients with cardiac arrest [19]. Another potentially beneficial use of BO is the monitoring of neurological status of critically ill patients who require extracorporeal membrane oxygenation (ECMO), often used in lung transplantation. Patients undergoing ECMO therapy are usually subjected to deep sedation, which limits other methods of controlling neurological status. Neurological complications are one of the most common complications in patients with ECMO support. The results of BO measurements may help to adjust ECMO parameters to ensure that the brain oxygenation is optimal. Due to the size of the arterial cannula, there is a high risk of peripheral ischemia of lower limbs. NIRS may be beneficial in early detection of ischemia but also in the early diagnosis of compartment syndrome and its consequences. Therefore, brain oximetry in ECMO may improve quality of patient care [20].
Nevertheless, this study cannot be considered without certain limitations. Firstly, we did not evaluate postoperative neurological complications. Simultaneous use of BO and SpO2 measurements should improve postoperative outcomes and decrease the rates of cognitive disorders. Secondly, we did not measure oxygenation in the postoperative period, which could depict the return of BO to baseline values and correlate with improvement of patients’ condition after surgery.
Conclusions
In the conducted study, we observed that cerebral oxygenation did not return to baseline values until the end of the surgery, unlike the SpO2. Furthermore, both SpO2 and BO correlate negatively with the overall duration of thoracic surgery. However, after 90 minutes of surgery, SpO2 stopped reflecting brain oxygenation. BO is a more sensitive method of detecting blood oxygenation decrease than SpO2 and it is subject to greater variations during thoracic surgery. Left lung surgery results in higher minimum SpO2 values than right lung surgery. However, this finding was not significant in the case of BO. In addition, minor alterations in SpO2 and BO values were noted during wedge resections compared to lobectomies. We found that there is a likely benefit from shortening the duration of surgery, which decreases the time of cerebral hypoxia. Baseline BO values are lower in elderly patients, but there were no age-related differences in SpO2 measurements.