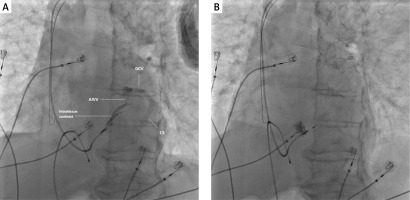
An 88-year-old man was admitted to the Cardiology Ward from the Emergency Department due to atrial tachycardia with complete atrioventricular block and a junctional escape rhythm of 35 beats per minute on the electrocardiogram. On admission, he was in a stable condition with no significant findings on physical examination. The patient complained mostly of severe dizziness without loss of consciousness for a few days preceding the hospitalization. After the admission the patient suffered from a recurrent ventricular fibrillation that was successfully defibrillated. Due to electrical instability a temporary pacing lead was placed in the right ventricle and the patient was scheduled for emergency pacemaker implantation. Since the anticipated ventricular pacing percentage was high, an attempt was made to position the lead in the left bundle branch area using a C315 HIS sheath with a Select Secure 3830 lead (Medtronic). After achieving the desired position on the interventricular mid-septum and an initial lead screw-in, a contrast medium was administered through the sheath, revealing a fistula draining into the coronary venous system (Figure 1 A). The lead was then repositioned posteriorly and superiorly on the septum, achieving left ventricle septal pacing (which, due to the patient’s advanced age and initial complications, was considered an acceptable position) without further complications (Figure 1 B). A follow-up echocardiographic study after the procedure ruled out any pericardial effusion, and further hospitalization was uneventful.
Figure 1
A – Initial ventricular lead position on the interventricular septum revealing a fistula draining through the anterior interventricular vein (AIVV) into the greater cardiac vein (GCV) and coronary sinus (CS), 30° left anterior oblique (LAO) view. B – Final ventricular lead position on the interventricular septum, 30° LAO view
Coronary venous fistula is an extremely rare complication during a left bundle branch area pacing procedure. Only a few similar cases without adverse outcomes have been described [1–3]. In a large, multicenter, observational study involving 2533 patients, Jastrzębski et al. described 7 similar complications (0.28%) [4]. Moreover, in the reviewed literature the approach to dealing with such findings was heterogeneous – only some of the operators chose to reposition the lead, while others accepted the electrode position, seemingly without negative consequences. In the present case, although there were no clinically significant symptoms related to the fistula, the decision was made to reposition the lead, which resulted in ventricular pacing with a narrow QRS morphology and no connections with the coronary venous system. This case highlights the importance of routine use of a contrast medium during physiological pacing procedures in order to rule out any arteriovenous connections after electrode placement. More studies are needed to evaluate the significance of coronary venous fistula during conduction system pacing procedures. Until more data are available, repositioning the lead might be a reasonable option.








