A 65-year-old woman with hypertension, hypercholesterolemia and diabetes was referred from another hospital for percutaneous retrieval of the unraveled coronary wire filament left in the ascending aorta after the unsuccessful percutaneous coronary intervention (PCI) on the chronically occluded (CT) right coronary artery (RCA).
In 2009 she sustained inferior wall myocardial infarction treated with RCA PCI with bare metal stent (BMS) implantation and staged left anterior descending (LAD) PCI with another BMS implantation. In 2022 LAD in-stent restenosis (ISR) was treated with implantation of 2 drug-eluting stents (DES) and the stenosis of the ramus branch of her left coronary artery was treated with drug coated balloon (DCB). Re-occlusion of the RCA was discovered at the same time and the decision was made to open the in-stent reocclusion electively in September 2023.
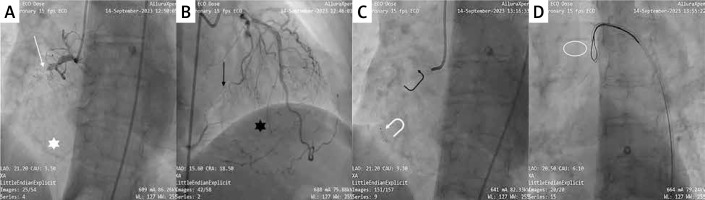
On angiography the tapered proximal cap was located in the proximal segment below the conus branch take-off. The course of the occlusion was relatively straight with moderate calcification and extended distal to the stent implanted in the distal segment. Some moderately tortuous septal branches from the LAD gave collaterals to the posterior descending artery (PDA) branch (CC1) and the posterior left ventricular (PLV) branch was filled via the epicardial collateral from the circumflex artery. A Judkins right (JR4) 6F guide catheter was introduced into the ostium of the RCA and only a balloon-supported wire was advanced into the body of the occlusion. After several minutes of manipulations and balloon inflations in the proximal segment, a Gaia second wire (Asahi) got stuck in the mid RCA segment within the stent, unraveled and broke, leaving its filament proximal end above the bifurcation of the aorta. The retrieval of the filament using a large 27–45 mm EnSnare (Merit Medical) was unsuccessful; part of the wire broke at the level of the brachiocephalic trunk take-off and was removed. The procedure took around 2.5 h with application of a 5 Gy dose of radiation (Figure 1).
Figure 1
Right coronary artery (RCA) angiogram: tapered proximal cap (white arrow) and stent (white star) (A); left coronary artery angiogram: septal collaterals from left anterior descending (LAD) (black star) and epicardial collateral from circumflex artery (black arrow) (B); stuck and unraveled Gaia second wire in mid RCA segment: clearly visible tip (white curved arrow) and poorly visible filament (black curved arrow) (C); unsuccessful retrieval of the filament by EnSnare (Merit Medical), the invisible distal end of the broken filament in the aortic arch (white ellipse (D)
On the first angiographic run done in our institution with the Launcher JR4 7F catheter (Medtronic) we discovered the ballooned proximal segment of the RCA with the visible tip of the wire in the mid segment and weak distal filling of the artery. The other end of the wire was hardly seen, freely floating in the aortic arch. We decided to snare the wire from the ascending aorta with a 27–45 mm Atrieve tulip-snare (Argon) introduced into a 6F Guidezilla guide catheter extension (Boston Scientific) to tighten the snare around the filament. After several torquing movements of the snare we grabbed the filament and gently closed it by pulling it back into the guide. At the same time we directed the guide into the ostium of the RCA using the filament as a rail. We introduced the guide extension as far as possible and then pulled on both the snare and the guide extension at the same time. The wire broke again and we managed to retrieve only a small part of the filament; the rest of it remained in the guide catheter. Then, we introduced the Solaris 2.5/20 mm semi-compliant balloon (Medtronic) to trap the filament at the tip of the guide. By pulling on the guide we removed another part of the filament, leaving only a few centimeters of it within the lumen of the right coronary artery. The procedure took 25 min with application of a 0.5 Gy radiation dose (Figure 2).
Figure 2
Visible tip of the wire in the mid RCA segment (white arrow) and “radiolucent” proximal end of the filament in the ascending aorta (white brace) (A), B – snaring the filament from the ascending aorta Ensnared filament pulled into the guide catheter tightly fixed by Guidezilla (C); short part of the filament retrieved after pulling on the snare and the guide extension (black arrow) (D); balloon trapping (white star) with guide extension at site (white arrow) (E); final results: long part of filament alongside the trapping balloon (black brace) (F)

We decided not to proceed with the CTO opening at the same setting, bearing in mind the time, contrast and X-ray burden of the previous procedure. The patient remained on dual antiplatelet therapy (DAPT). We scheduled the cardiac magnetic resonance and the clinical follow-up in 3 months.
We present the case of this rare PCI complication for two reasons. First, we wish to emphasize the importance of proper preparation for the CTO PCI, particularly in severely calcified or restenotic lesions by using contrast dual injections, the supportive proper size guide catheter, the microcatheter, and avoiding over-torqueing of the wire when its tip is stuck in the lesion. Second, we present a technique to retrieve the unraveled filament of the coronary wire in the aorta using a large 3-loop snare. We must understand the challenges of snaring the unraveled wire in the aorta: the poor visibility of the wire segment, the size of the aorta and the risk of fracturing the wire during snaring. To face them, the technique we present includes a large 3-loop snare that would occupy the aorta and blindly grab the invisible wire fragment, the guide extension catheter to tighten the snare around the filament, introduction of the guide catheter over the rail formed by the captured filament back into the ostium of the artery, and the balloon trapping within the guide catheter in case of filament breakage [1–3].








