Introduction
Following its discovery in December 2019 in Wuhan, China, COVID-19 swiftly disseminated across the globe, prompting the World Health Organization (WHO) to declare it as a pandemic emergency [1]. As of July 5, 2023, the total number of confirmed COVID-19 cases stands at 767,726,861, with 6,948,764 deaths reported worldwide [2].
In the context of intensive care units (ICUs), the separation of family members from their loved ones poses significant challenges and disrupts their coping mechanisms and experiences of pain. In addition to their role as decision-makers, families in ICUs serve as direct sources of comfort, advocates for patients’ wishes, and sources of information [3]. Attention has been given to the ICU as a source of abnormal experiences for patients and their families, resulting from the disease, injury, or treatment [3].
Family caregivers who assume caregiving roles for their loved ones may experience a combination of positive and negative experiences. They often face physical and psychological challenges, such as caregiving overload and emotional stress [4]. Several factors contribute to caregiver distress, including limited leisure time, lack of assistance from other family members, inadequate knowledge about caregiving, caregiver age, and feelings of guilt for not addressing the patient’s complaints [5,6].
Limited research has focused on capturing the perspectives of family members affected by COVID-19. One such study delved into these experiences and identified several key themes, including the nature of the disease, unmet needs, negative physical, psychological, and social encounters, factors facilitating care, and positive experiences [7].
These encounters may lead to a diminished quality of life for family members. Consequently, the implementation of supportive interventions for family caregivers becomes crucial, as it can help reduce the overall cost of care by enabling home caregiving. However, the experiences of family members of admitted COVID-19 patients in Iraqi Kurdistan remain underexplored [8]. Moreover, previous investigations have predominantly employed a qualitative approach and have primarily focused on patients admitted to ICUs. Furthermore, these studies specifically included patients who were exclusively admitted to ICUs and did not include individuals who were admitted to other medical wards within the hospitals.
Aim of the work
In this study, the objective was to examine the experiences of companions of COVID-19 patients admitted to COVID-19 hospitals using a quantitative approach.
Material and methods
Study design and sampling
This retrospective cross-sectional study enrolled companions of COVID-19 patients who had been admitted to a COVID-19 hospital. The researchers reached out to the companions to participate in the study. The investigation specifically focused on companions of patients admitted to one of three COVID-19 hospitals situated in Duhok City in the Iraqi Kurdistan. The companions of admitted patients were contacted in order to gather their experiences regarding communication with medical staff at the COVID-19 hospitals through a questionnaire survey.
The study included the companions of patients admitted between 2020 and 2022 to three COVID-19 hospitals in Duhok City. The medical records of one hospital (created in 2022) were not included due to the mixing of patient records with other records in the hospital’s archive (Azadi Teaching Hospital). Consequently, a non-random sample of COVID-19 patients from Lalav Respiratory Disease Hospital and COVID-19 Hospital was included.
To obtain a practical and representative sample of patients admitted to these two hospitals since the onset of the outbreak by April 2020, a medical record was selected from every five records. If the fifth record had substantial missing information, the next one was included in the study. The companions who cared for the patient at the hospital were included in the study.
Inclusion and exclusion criteria
The study included the companions of COVID-19 patients admitted to one of three COVID-19 hospitals between 2020 and 2022. Companions of different ages and socio-demographic backgrounds were eligible. Our study exclusively included companions who actively provided care for the patients while they were admitted to the hospitals. Individuals who were not ready to participate or did not respond to two calls were excluded. A total of 502 companions were called for this study, out of which 57 did not respond and 8 did not accept to participate (response rate: 87.05%). The patients included in this study were those admitted to either an intensive care unit (ICU) or a medical ward at one of the COVID-19 hospitals. Severe and critical COVID-19 patients were admitted directly to an ICU. Patients with mild to moderate severity were admitted to a medical ward at the hospital at early stages of the outbreak. In cases of escalating medical conditions, those with mild to moderate cases were transferred to an ICU.
Data collection
General and medical characteristics of COVID-19 patients were obtained from their medical records. The experiences and characteristics of companions were collected through the self-reporting technique by a questionnaire survey. The severity of COVID-19 was recorded based on the national guidelines for COVID-19 diagnosis [9]. The mild and moderate cases were admitted to the COVID-19 hospitals and were included in this study as they were admitted at the beginning of the outbreak (2020) in the Iraqi Kurdistan.
Patient and public involvement
This study was conducted to examine the experiences of patients' companions receiving care at COVID-19 hospitals. Healthcare workers should take into account the perspectives of both companions and patients to enhance patient involvement in the treatment process.
Statistical analyses
Descriptive statistics were applied to the general information of the patients and their companions. The prevalence of companions’ experiences was determined in terms of number and percentage. Factors associated with companions’ satisfaction were examined using the Pearson Chi-squared test. Statistical calculations were performed using JMP Pro 14.30.
Ethical considerations
Ethical approval for the study was obtained from the local health ethics committee in Duhok City, registered under reference number 21082022-6-6 on August 21, 2022. Companions had the freedom to reject participation, and verbal consent was obtained before their involvement. The names of the companions were not included in the study.
Results
Demographic characteristics of COVID-19 patients and their companions
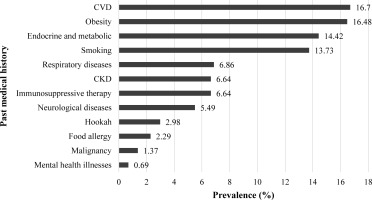
The mean age of admitted COVID-19 patients was 56.74, ranging from 9 to 107 years. The patients belonged to different age groups, with the majority falling between 40 and 80 years old (70%). There was only one child, and one patient was aged 107 years old. Among the patients, 54.92% were male and 45.08% were female. The duration of hospitalization ranged from 1 to 42 days, with a median of 5 days. The patients had varying degrees of disease severity: mild (34.55%), moderate (27.92%), severe (20.14%), and critical (17.39%). The most prevalent comorbidities among the admitted COVID-19 patients were cardiovascular disease (16.7%), obesity (16.48%), endocrine and metabolic disorders (14.42%), and smoking (13.73%). Out of the total 437 patients included in the study, 23.80% died, and the remaining 76.20% recovered from the disease (Table 1, Figure 1). The mean age of the companions of admitted COVID-19 patients was 35.04, ranging from 18 to 65 years. The majority of companions fell between 20 and 50 years old (90%). Among the companions, 74.14% were male and 25.86% were female, with different education levels. Most of them were family members (92.45%), followed by close friends (5.95%) and friends (1.6%) (Table 1).
Table 1
General and medical characteristics of the patients admitted to the COVID-19 hospitals and the facilities
Lived experiences of the patients’ companions
Communication
The study revealed that 79.63% of companions had regular communication with the medical staff, and 71.40% received relevant and sufficient information about the patients’ medical conditions. Additionally, 86.50% reported that the communication from the medical staff was polite and ethical. Fear
Regarding mental health, 34.55% of companions reported fear of COVID-19 infection at the hospitals, and 66.59% expressed fear of the given patient’s death.
Behavior
The study found that 79.86% of companions reported trust in the treatment of patients by the medical staff. Regarding conflicts, 10.76% and 10.07% of companions reported conflicts with nurses and doctors, respectively.
Satisfaction
The majority of companions (86.96%) expressed satisfaction with the healthcare and treatment received at the COVID-19 hospitals. More than sixty percent (66.59%) of companions reported being informed about the patient’s care during their visits to the hospital.
Availability of medical staff
In terms of the availability of medical staff, the majority of companions reported that nurses and doctors were always accessible when needed and answered their questions about the patient’s conditions. Moreover, most companions reported that their needs were addressed by nurses.
Hospital visit attitudes
Regarding hospital visits, most companions reported that the patients were not willing to see their relatives at the hospital (65.45%).
Environment
Regarding the hospital environment, 71.17% of companions reported that the given patient’s room was quiet, while 69.11% reported that the hospitals were quiet for the patients. However, 28.83% and 30.89% reported that the given patient’s rooms and hospital, respectively, were not quiet. In terms of psychological well-being, participants reported that 33.87% of the patients were affected by the ambient noise, and 53.32% were affected by other patients’ fear. Nearly half of the companions reported being infected by COVID-19 while visiting in the hospital (Table 2).
Table 2
Lived experiences of the companions of the COVID-19 patients
The study showed that companions of COVID-19 patients admitted to the medical ward were more likely to experience fear of patient death compared to those whose patients were admitted to an ICU (36.84% vs. 29.75%; p<0.0001). In terms of other experiences, there were no significant differences between the companions of patients in the medical ward and ICU (Table 3).
Table 3
Lived experiences of the companions of the COVID-19 patients per the department
The study revealed that companions who had patients with more severe conditions were more likely to experience fear regarding the possibility of their given patient dying at the hospital. A similar pattern was observed among individuals who had companions or close friends admitted to the hospitals. This fear was more prevalent among companions aged between 30 and 50 (Table 4).
Table 4
Association of the companions’ fear of the patients’ death with demographic characteristics
The study showed that the companions with no regular communication with nurses (23.60% vs. 7.47%; <0.0001) and doctors (21.35% vs. 7.18%; p<0.0001) were more likely to report conflicts with nurses and doctors compared to those who had regular communication with nurses and doctors (Table 5).
Table 5
Association of the conflicts between the companions and medical staff with the regular communication
Discussion
This study showed that COVID-19 patients of different severity and age groups were admitted to the hospital. The majority of the companions reported positive experiences with the treatment of COVID-19 patients in hospitals in the Iraqi Kurdistan. This included regular and polite communication with the medical staff, trust in the treatments, and the availability of medical personnel. However, the main concerns expressed by the companions were the fear of contracting COVID-19 at the hospital and environment-related issues. The primary environment-related problems mentioned by the companions were the lack of quiet in the given patient’s room and hospital, which had a psychological impact due to ambient noise and the fear expressed by other patients.
The literature has reported some issues similar to those reported in our study. Of these, a thematic analysis study reported [10]. The experiences of family members can be categorized into seven main themes: (a) responses to the COVID-19 diagnosis, (b) the disruptive impact of COVID-19 on the family unit, (c) the influence of COVID-19 on the grieving process, (d) the desperate search for information, (e) the needs of family members themselves, (f) conflicting emotions regarding video calls, and (g) gratitude for the quality of care provided. Family members’ stress and anxiety were intensified by their emotions towards the given patient’s diagnosis and the circumstances of contracting the virus. They struggled to stay informed about the care being provided, which they couldn’t witness firsthand, and they faced challenges in comprehending the available information. Family members expressed dissatisfaction with video calls as a means of communication. Despite these difficulties, they acknowledged the dedication and care demonstrated by healthcare providers on the frontlines, and their appreciation for their loved one’s well-being. These experiences were reported by the family members in a medical ICU in Buffalo, New York, United States. They obtained the required information through the individual telephone interviews in a private room to maximize privacy and reduce interruptions.
Specifically, the experiences of the family members of patients with severe COVID-19 who died in ICUs in France were the challenge with the difficulty of establishing a connection with the ICU medical staff and coping with feelings of isolation. Family members faced obstacles in developing a rapport and understanding the medical information provided by the ICU team. Distance communication alone was insufficient, exacerbating the sense of solitude experienced by the participants. The second challenge centered on the presence of the patient in the ICU and the associated risks of separation. Due to limited access to the ICU, family members encountered disruptions and gaps in their relationship with their loved ones. These disruptions resulted in feelings of helplessness, abandonment, and a sense of unreality. The third challenge revolved around the disruptions in end-of-life rituals. Family members expressed the loss of meaningful moments following the patient’s death, which generated intense feelings of disbelief. These experiences could potentially contribute to complicated grief [11]. Similar experiences were reported in developing countries [7,12].
It seems that regular communication with the medical staff and receiving medical information about the patients’ conditions are the main challenges in developed countries. The family members had contact with the medical staff only through video calls. The family members/relatives had direct and regular contact with the medical staff (nurses and doctors) in Iraqi Kurdistan. The family members of COVID-19 patients receiving care in ICUs are at high risk of psychological burden [13]. Two significant risk factors identified are having a loved one who passed away or was in critical condition and experiencing inadequate communication with the ICU team. The quality of communication with the ICU team has been determined to play a crucial role in shaping the experiences of family members, both during the patient’s stay in the ICU and in the aftermath of their death [14]. The family members had direct communication with the medical staff instead of the distance communication in developed countries [10,11]. However, direct communication increases the risk of COVID-19 infection as close to half of the family members/relatives reported that they were infected by COVID-19 at the hospitals. Families of ICU patients often require repeated and varied information, and they need the ability to continuously ask questions in real time. While telephone and video calls can facilitate communication between clinicians and family members regarding the patient’s condition, the absence of a strong connection between the family and the ICU team can lead to tension. A considerable percentage of the companions reported that they had conflicts with medical staff (10%). This study showed that companions who did not have regular communication with medical staff were more likely to report a conflict. But, we are unaware of the conflicts occurred between companions and medical staff.
Unfortunately, phone and video calls often focus primarily on providing technical information rather than fostering effective communication, which can leave the family feeling frustrated. Effective communication, on the other hand, entails not only conveying information but also involves verbal and nonverbal communication, active listening, and empathetic statements to establish a high-quality interaction [15]. High-quality communication not only enables the family to comprehend the situation better but also helps them feel accepted, supported, and able to place trust in the healthcare team. Distance communication, such as through phone or video calls, may not offer the same level of emotional connection and support as face-to-face interactions. The physical distance can create barriers to establishing a strong sense of acceptance, support, and trust that are crucial for effective communication and a positive experience for the family [16].
The psychological well-being of the admitted COVID-19 patients must not be ignored in ICUs, especially the severe and critical patients. The companions reported that the patients responded negatively to the unpleasant sounds of the hospital. When a patient died, the ambulance vehicle used a powerful siren when transporting the deceased patient to the forensic medicine department. This siren generated a high level of fear in the patients hospitalized for COVID-19. Some rooms were designated for more than one patient. Therefore, the admitted patients in the same room were negatively affected when they witnessed the death of the patient sharing the room. In addition, some patients were weak psychologically and had a high level of fear. The fear of these patients strongly affected other patients psychologically. It could prove necessary to provide mental health services to patients admitted for COVID-19 and to their companions as well.
Strengths and limitations
The strong point of this study is that we tried to include as much as possible the experiences in a quantitative study. The randomization process was not possible in this study due to not being provided the patient lists by the COVID-19 hospitals, but the response rate was high. In addition, we included one patient in each five medical records in this study.