Summary
Transcatheter aortic valve implantation (TAVI) has grown to be an alternative treatment for severe symptomatic aortic valve stenosis (AS) in elderly patients. Although TAVI is a less invasive procedure, some patients may require prolonged hospitalization. The aim of this study was to find the determinants of prolonged hospitalization in patients who underwent trans-femoral TAVI. We found that moderate or severe mitral regurgitation and decreased estimated glomerular filtration rate were significantly associated with prolonged hospitalization, while current chopsticks user and taking angiotensin-converting enzyme inhibitors/angiotensin-receptor blockers or statins before TAVI were inversely associated. This was confirmed by multivariable logistic regression analysis.
Introduction
Transcatheter aortic valve implantation (TAVI) has grown to be an alternative treatment for severe aortic valve stenosis (AS) in elderly patients irrespective of surgical risk [1, 2]. Since TAVI was a less invasive surgery than surgical aortic valve replacement (SAVR) [1, 3–5], the length of hospitalization was shorter in patients who underwent TAVI than in patients who underwent SAVR [1, 4]. Moreover, trans-femoral TAVI is less invasive than trans-apical TAVI [6]. Prolonged hospitalization should be avoided for elderly patients, because the cognitive function and athletic performance in elderly tend to decline during hospitalization [7–9]. However, some patients who underwent TAVI still require prolonged hospitalization. The reasons for prolonged hospitalization have not been fully investigated in Japanese patients.
Aim
The aim of the present study was to find the pre-procedural factors that have an association with prolonged hospitalization in patients who underwent trans-femoral TAVI.
Material and methods
Patients
We included consecutive patients who underwent TAVI in our medical center from July 2014 to December 2017. Each candidate for TAVI was referred to the heart team in our medical center, and the treatment strategy including TAVI, SAVR, or non-surgical therapy was discussed on a weekly heart team conference. Exclusion criteria were TAVI by the (1) trans-apical approach, (2) trans-iliac approach, (3) trans-subclavian approach, and (4) direct aorta approach.
According to the length of the whole hospitalization period, the study population was divided into the conventional hospitalization group (≤ 21 days) and the prolonged hospitalization group (> 21 days) [10]. Clinical characteristics were compared between the conventional and prolonged hospitalization groups, and multivariate logistic regression analysis was performed to find the determinants of prolonged hospitalization.
Trans-femoral TAVI procedure
In our medical center, trans-femoral TAVI was performed by surgical cut-down approaches. Before induction of anesthesia, we inserted a 5 Fr sheath into a femoral artery and a 5 Fr sheath into a femoral vein, which were kept during the TAVI procedure as rescue lines. A temporary pacemaker was inserted via the internal jugular vein for rapid ventricular pacing. After general anesthesia, we revealed another femoral artery by the cut-down method and inserted an 8 Fr sheath into the femoral artery. We exchanged the 8 Fr sheath for the main sheath (14 to 18 Fr) following insertion of the stiff guide wire. Valve crossing was performed using a straight wire. After successful valve crossing, we exchanged the straight wire for a stiff wire that had a pre-shaped safety curve. According to the agreement of our heart team, we sometimes performed balloon aortic valvuloplasty and/ or protection of coronary arteries before implantation of a biological aortic valve. Then, we implanted a biological aortic valve (balloon-expandable type or self-expandable type). During the operation, activated coagulation time was maintained ≥ 250 s.
Definitions
Hypertension was defined as receiving treatment for hypertension before admission. Dyslipidemia was defined as total cholesterol > 220 mg/dl, low-density lipoprotein cholesterol > 140 mg/dl, or medical treatment for dyslipidemia. Diabetes mellitus (DM) was defined as hemoglobin A1c (HbA1c) > 6.5% (national glycol-hemoglobin standardization program (NGSP) value) or medical treatment for DM [11]. Estimated glomerular filtration rate (eGFR) was calculated by the modification of diet in renal disease (MDRD) method adjusted for the Japanese population [12, 13]. Atrioventricular block was defined as PR interval > 200 ms or certain dissociation of atrioventricular conduction [14]. Acute decompensated heart failure (ADHF) was defined as New York Heart Association class ≥ II, evidence of congestion revealed by physiological findings, chest X-ray and/or echocardiogram, or diagnosis by experienced cardiologists [15, 16]. Recent percutaneous coronary intervention (PCI) was defined as a history of PCI within 1 year from TAVI. The number of aortic valve cusps, diameter of annulus, maximum velocity of aortic valve, value of E/A, severity of aortic valve regurgitation and mitral valve regurgitation (MR) were investigated by echocardiography. Left ventricular ejection fraction were measured by the Teichholz method, and aortic valve area was calculated by the continuity equation method. We also performed contrast enhanced computed tomography (CT) to obtain information regarding annulus area, annulus perimeter, diameter of Valsalva sinus, diameter of sino-tubular junction, coronary height, and characteristics of access vessels. Each STS score [17–19] and logistic EuroSCORE [20, 21] were calculated before the procedure using online available calculators. Post-procedural events such as new stroke or conduction disturbance were defined according to the Valve Academic Research Consortium 2 [22]. Furthermore, ability to have meals by using chopsticks was routinely checked at the time of hospital admission by a nurse in the medical ward. Patients who were able to eat meals with chopsticks were defined as current chopsticks users. In general, almost all Japanese are chopsticks users, at least when they are young. Thus, non-current chopsticks users at admission were at least former chopsticks users.
Statistical analysis
Categorical data were presented as number and percentage, and continuous data were presented as mean ± standard deviation (SD). Normally distributed continuous variables were compared using the unpaired Student’s t-test. Other continuous variables were compared using the Mann-Whitney U-test. Categorical data were compared using the χ2 test or Fisher’s exact test. Multivariate logistic regression analysis was performed to find the determinant of prolonged hospitalization. In this model, the prolonged hospitalization group was used as a dependent variable. In the present study, our goal was to find the predictors from baseline clinical factors. Therefore, in multivariate analysis, we selected independent variables from baseline clinical factors. Furthermore, we used well-known variables such as albumin value and STS score. We also added right bundle branch block (RBBB) because RBBB was a major risk of de novo pacemaker implantation. Variables that showed significant differences (p < 0.05) between the two groups in univariate comparisons were also used as independent variables. Variables that had missing values were not included in the multivariate analysis. Odds ratios (OR) and 95% confidence intervals (95% CI) were calculated. A p-value < 0.05 was considered statistically significant. All analyses were performed using the statistical software SPSS PASW Statistics 18, release 18.0.0/Windows (IBM Corp.).
Results
We screened the consecutive 129 patients who underwent TAVI in our medical center from July 2014 to December 2017. We excluded 31 trans-apical approached cases, 2 trans-iliac approached cases, 1 trans-subclavian approached case, and 1 direct aorta approached case. A total of 94 AS patients who underwent trans-femoral TAVI were included as the final study population. The study population was divided into the conventional hospitalization group (≤ 21 days) (n = 74) and prolonged hospitalization group (> 21 days) (n = 20) (Figure 1). The mean length of hospitalization in the conventional hospitalization and prolonged hospitalization groups was 14.9 ±2.9 days and 31.2 ±16.0 days, respectively (p < 0.001).
Figure 1
Flowchart of patient inclusion: a flowchart of how to determine the final study population, conventional hospitalization group and prolonged hospitalization group
TAVI – trans-catheter aortic valve implantation.

The comparisons of baseline characteristics are shown in Table I. The prevalence of current chopsticks users was significantly greater in the conventional hospitalization group (97.3%) than in the prolonged hospitalization group (65.0%) (p < 0.001). The ADHF at admission was lower in the conventional hospitalization group (54.1%) than in the prolonged hospitalization group (80.0%) (p = 0.04). The eGFR was greater in the conventional hospitalization group (57.5 ±23.2 ml/min/1.73 m2) than in the prolonged hospitalization group (42.7 ±18.4 ml/min/1.73 m2) (p = 0.01). Moderate or severe MR was more frequently observed in the prolonged hospitalization group (40.0%) than in the conventional hospitalization group (13.5%) (p = 0.01). STS score was significantly lower in the conventional hospitalization group (6.19 ±5.72) than in the prolonged hospitalization group (9.82 ±11.91) (p = 0.006), whereas logistic EuroSCORE was not different between the groups (p = 0.77).
Table I
Comparison of baseline characteristics
[i] ADHF – acute decompensated heart failure, COPD – chronic obstructive pulmonary disease, IP – interstitial pneumonia, PCI – percutaneous coronary intervention, eGFR – estimated glomerular filtration rate, PT-INR – prothrombin time-international normalized ratio, APTT – activated partial thromboplastin time, BNP – brain natriuretic peptide, RBBB – right bundle branch block, LBBB – left bundle branch block, LVEF – left ventricular ejection fraction, LVD – left ventricular diameter, PG – pressure gradient, AR – aortic valve regurgitation, MR – mitral valve regurgitation, ACEI – angiotensin converting enzyme inhibitors, ARB – angiotensin II receptor blockers, STS – Society of Thoracic Surgeons.
Table II shows the comparisons of procedures and complications following TAVI between the two groups. There were no significant differences except complications following TAVI. We also checked the direct reasons why the hospitalization period was prolonged. The most frequent reason was new pacemaker implantation, and the second most frequent reason was peri-operative ADHF (Figure 2).
Table II
Comparison of procedure and after TAVI
Figure 2
Main causes of prolonged hospitalization periods
ADHF – acute decompensated heart failure, CKD – chronic kidney disease.
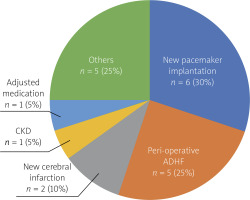
Table III shows the multivariate logistic regression analysis to identify the determinants of the prolonged hospitalization group. Moderate or severe MR was significantly associated with prolonged hospitalization (OR = 4.49, 95% CI: 1.16–17.47, p = 0.03). Current chopsticks user was inversely associated with prolonged hospitalization (OR = 0.05, 95% CI: 0.01–0.41, p < 0.01). Furthermore, eGFR value (per 15 ml/min/1.73 m2 incremental) (OR = 0.49, 95% CI: 0.26–0.90, p = 0.02), taking statins (OR = 0.13, 95% CI: 0.02–0.71, p = 0.02) or angiotensin converting enzyme (ACE) inhibitors/angiotensin II receptor blockers (ARB) (OR = 0.25, 95% CI: 0.06–0.96, p = 0.04) on admission were also inversely associated with prolonged hospitalization.
Table III
Multivariate logistic regression analysis
[i] MR – mitral valve regurgitation, eGFR – estimated glomerular filtration rate, ACE – angiotensin converting enzyme, ARB – angiotensin II receptor blockers. Initial step included current chopsticks user at admission, moderate or severe MR, Pre eGFR, statin, ACE inhibitors/ARB, ADHF, albumin value, right bundle branch block, atrioventricular block and STS score before procedure.
Discussion
We included 94 AS patients treated by trans-femoral TAVI, and analyzed the determinants of prolonged hospitalization using multivariate logistic regression analysis. The most frequent cause of prolonged hospitalization was new pacemaker implantation (30%), followed by peri-operative ADHF (25%) (Figure 2). Multivariate logistic regression analysis revealed that moderate or severe MR was significantly associated with prolonged hospitalization, whereas current chopsticks user was inversely associated with prolonged hospitalization. Furthermore, eGFR value (per 15 ml/min/1.73 m2 incremental) and taking statins or ACE inhibitors/ARB at admission were also inversely associated with prolonged hospitalization.
We should discuss why moderate or severe MR was significantly associated with prolonged hospitalization. Because patients in the present study were very elderly (83.7 ±5.1 years old), the etiology of MR would be secondary such as volume over caused by heart failure rather than primary such as mitral valve prolapse [23, 24]. As peri-operative ADHF was the second most common reason for prolonged hospitalization, moderate or severe MR might reflect the severity of ADHF before trans-femoral TAVI.
We revealed that current chopsticks user at admission was inversely associated with prolonged hospitalization. Current chopsticks user may reflect the patient’s frailty as well as nutritional status. In patients with acute heart failure, nutritional status was associated with prolonged hospitalization [25, 26]. Furthermore, frailty is known to be associated with prolonged hospitalization, re-hospitalization, and death in elderly patients in acute care settings [27]. Therefore, “current chopsticks user” can be a simple predictor reflecting the patient’s nutrition status and frailty in patients with AS.
The eGFR was also inversely associated with prolonged hospitalization. This association may be related to acute kidney injury (AKI) after TAVI. AKI after TAVI was reported to be a risk factor for prolonged hospitalization [28]. The chance of AKI after TAVI might be enhanced by decreased eGFR [29].
ACE inhibitors/ARB user at admission was inversely associated with prolonged hospitalization. Since ADHF was the cause of prolonged hospitalization, ACE inhibitors/ARB might improve patient’s heart failure [30, 31]. Another reason was that unstable AS patients tended to have less chance to be prescribed ACE inhibitors/ARB, because ACE inhibitors/ARB have been considered not to be safe for symptomatic severe AS [32]. Similarly, statin user at admission was inversely associated with prolonged hospitalization. Unstable AS patients did not have a chance to be prescribed statins.
Current risk scores such as STS score or EuroSCORE calculate the risk of death associated with surgery, but do not address prolonged hospitalization. Prolonged hospitalization is closely associated with decline of activities of daily living (ADL) in elderly patients [7–9]. It may be important to find a new risk score to address the prolonged hospitalization for patients who undergo TAVI. Although our study would be helpful to find such a risk score, we need more data and future studies to establish a new risk score.
Study limitations
First, since this study was a retrospective study, there was a potential selection bias. The most frequent reason for prolonged hospitalization was new pacemaker implantation. This could be caused by the procedure of TAVI or selection of bioprosthetic valves, while the type and size of bioprosthetic valves were not different between the conventional and prolonged hospitalization groups. Although we proposed current chopsticks user as a simple indicator of prolonged hospitalization, it is unclear whether current chopsticks user can be an indicator of prolonged hospitalization in patients who undergo trans-apical TAVI. Since minimum thoracotomy is necessary for trans-apical TAVI, the predictors of prolonged hospitalization may be more complex in trans-apical TAVI as compared to trans-femoral TAVI. As the study population was relatively small, the statistical analysis has an inherent risk of β error [33]. We should mention about the length of hospitalization. The length of hospitalization was much longer in our hospital than in US or European countries (Table II). Although the safety of short hospitalization after TAVI have been reported [34, 35], clinical experience of TAVI might not be sufficient yet in Japan as compared to US or European countries, which might have the length of hospitalization longer than in our study. Furthermore, the drive to minimize the length of hospitalization may be weaker in Japan than in other countries, because the cost of additional hospital stay, especially the self-pay burden, is quite low in Japan. TAVI with percutaneous femoral puncture or local anesthesia was less frequently performed in Japan than in US or European countries [36], which might prolong the length of hospitalization in our study. However, in several conditions, the duration of hospitalization is gradually getting shorter in our center. We should also discuss the many ADHF patients at the baseline of the present study. Since it was difficult to distinguish ADHF from advanced chronic heart failure, we might include advanced chronic heart failure as ADHF.
Since our study population consists entirely of Japanese patients who can use or could use chopsticks, whether a patient is a current chopsticks user or not was a meaningful question that reflects frailty. However, current chopsticks user may not reflect frailty in western countries.
Conclusions
In patients who underwent trans-femoral TAVI, moderate or severe MR was significantly associated with prolonged hospitalization. Current chopsticks user, eGFR value, and taking ACE inhibitors/ARB or statins before the procedure were inversely associated with prolonged hospitalization. Current chopsticks user would be a simple indicator reflecting frailty as well as nutritional status for patients with TAVI.








