Introduction
Chronic wounds include primary venous leg ulcers (VLUs), pressure ulcers (PUs), diabetic foot ulcers (DFUs), and burns (BUs). Wound management is a challenge in terms of the way, duration and cost of treatment both for the patient and health providers. The healing of skin wounds is a highly multi-step coordinated process where four phases can be differentiated: haemostasis, inflammation, proliferation, and remodelling. These phases follow each other and each stage is essential in the healing process. Objective monitoring of treatment at every stage is necessary to assess the applied therapy [1–4]. Thus, an objective assessment of the progress of treatment of chronic wounds (VLU, PU, BU) is very important, an appropriate objective geometric measurement method that gives a response to the effectiveness of the therapy used. Medical records must include wound measurement results such as length, width, surface area, circumference, and volume, with small measurement errors. For these measurements, various measurement techniques are used, from analogue to digital, which, along with the technical progress and development of technology, are becoming more accurate, more effective and more easily available [5, 6].
Analogue methods include the assessment of the healing progress by measuring the two axes of the wound (length – L and width – W) L × W, as shown in the results of Rogers et al. Studies have shown that this method overestimates the values by up to 41% [7]. Since many wounds are roughly elliptical in shape, the researchers used a mathematical model that approximates the surface of the wound to the surface of an ellipse. It consists in multiplying the length and width of the wound by π or another constant. A similar approach was taken by Bowling and Show, who used similar equations: area1 = L × W × π × 0.25 (Bowling) and area2 = L × W × 0.73 (Show). The formulas (area1 and area2), apart from the axis of the wound, were multiplied by the authors by a constant value differing by 0.05. Bowling reported that this approach was questioned for wounds greater than 40 cm2 [8, 9]. Digital methods include both contact and non-contact digital planimetry and methods using dedicated software. Digital contact planimetry was used in studies by Dolibog (VLUs) [10–12], Taradaj (VLUs) [13], Franek (PUs) [14] and Polak (PUs) [15]. It consists in drawing the shape of the wound on the foil, and then using a digitizer (Kurta XGT, Altek Inc, USA) and the C-Geo software (CGS) (Nadowski, Poland) to calculate the length, width, circumference and surface area of the wound. The authors report the absolute error of area measurement caused by the thickness of the plotting device (0.2 mm) and of the digitizer’s cross-hair (0.1 mm), whose value ranges from 13.1% to 2.7% for wounds with a surface area ranging from 1 to 70 cm2 [10–15]. Non-contact digital planimetry is used by taking a photograph of the wound with a dimension reference marker in the first stage. The second step is to use a graphics program (Photoshop, ImageJ, AutoCad) to calculate the dimensions of the wound. With large wounds surrounding the limb, the measurement error increases due to the curvature of the wound surface area. Eberhardt et al. presented, as the aim of the work, verifying the reproducibility of using AutoCAD software (ACS) to measure the area of VLUs. Pictures with a digital camera (Fujifilm Camera FinePix S14) with a marker were taken by both researchers and nurses. Then, on this basis, the outline of the ulceration was made and the marker was calculated from the given formula: wound area = (wound area obtained with AutoCAD ×9)/(square area obtained with AutoCAD). Researchers have shown that the program is more accurate for ulcers over 10 cm2 than for ulcers lower 10 cm2, without specifying accuracy [16, 17].
Waniczek et al. presented a method of planimetry based on taking a series of photos with a digital camera (Canon PowerShot G9) at different angles to the wound surface. Then, using Adobe Photoshop CS3, the authors superimposed successively taken photos of the wound from the surface of the oval limb. The image processed in this way was digitally analysed to calculate the ulcer surface area. The method error was determined to be about 1.46% [18].
Non-contact methods are also programs intended directly for assessing the dimensions of wounds. Foltyński created the Planimator app for Android. It showed almost two times more precision than the Visitrak device, the SilhouetteMobile device (Aranz, New Zealand), the AreaMe software [19, 20]. Glik et al. used Planimetric system IRIS® (Medicom, Wrocław, Poland) to monitor the healing progress of chronic wound treatment with hyperbaric oxygen therapy. The researchers found the system useful, but did not pay attention to measurement errors [21].
In turn, Chaby et al. demonstrated the operation of the digital 3D LifeViz Imaging System (QuantifiCare SA, Valbonne, France) for imaging ulcers. The system has been shown to be a non-contact stereophotographic method that provides measurements of the VLU area or changes in VLU areas that are as accurate and reliable as those obtained using the planimetric method and under conditions as close as possible to those of a clinical trial [22].
In another study Williams et al. compared the accuracy and reproducibility of two systems: Eykona camera (Fuel 3D, UK) and Silhouette camera (ARANZ, New Zealand) to measure the wounds. In terms of the wound area, both systems match the accuracy of traditional planimetry. However, the volume measurement is already underestimated by 58% (Eykona) and 28% (Silhouette), respectively. In addition, the authors emphasize that the use of 3D systems in the clinic is too expensive and therefore may have limited clinical use [23].
Dymarek et al. used the planimetric smartphone device (iPhone 7 Plus) application – Swift Skin and Wound Mobile App (Swift Medical, Canada) for imaging and documenting the progression of pressure ulcer healing. The software allows to calculate the length, width and area of the wound. The authors indicate that the measurements have negligible error smaller than 0.5% and low 2–5% variability [24].
Most articles published on the digital planimetry involved comparison of the most common two measurement methods and the vast minority involved calculation of measurement errors of the applied method.
Aim
The aim of the study was to show the possibility of using the AutoCad software as a tool for accurate geometric measurement (area, perimeter) of the venous leg ulcers on the lower limbs and compare with the contact planimetry method.
Material and methods
Study design
The study was designed and performed in the Department of Biophysics in Zabrze, Poland and the Department of Dermatology of the Medical University of Silesia. All participants provided informed consent to this project that was approved by the Bioethics Committee of the Medical University of Silesia in Katowice.
Planimetric laboratory assessment for wound models
Four Circle Templates for Drafting of diameter of 5, 10, 20 and 40 mm, imitating four different wounds surface areas of wounds were used as ulcer models. This choice was intentional due to the good imitation of the curves of natural wounds. The wound models were photographed using a smartphone (SAMSUNG smartphone Z3 FLIP, Korea) at a 90-degree angle to the surface. The ruler with an accuracy of 0.1 cm was used as a calibration marker. The measurements of the surface area and circumference for the wound model were performed by using a personal computer (ASUS with Windows 10 OS) with AutoCad software (Autodesk, 2013, USA). Each wound model was ten times outlined, starting always in a different place to determine the average areas and perimeters of the model.
Technical note
Before drawing the outline of the model, each image was scaled to the calibration ruler dimensions using the ALIGN command (which aligns objects with other objects in 2D and 3D). After calibration the ulcer was outlined and drawn onto an electronic image file (.jpeg) using a command PLINE (which creates a 2D polyline, a single object that is composed of line and arc segments) and its area and perimeter was calculated using PROPERTIES (displays properties palette) command.
Error measurement
The error of measurement method consists of a systematic error, largely dependent on the absolute measurement method used (software, calibration), and a random error, which is the standard deviation here.
The absolute measurement error (AE) was calculated using the formula: AE = X – X 0; where: X – real value measured; X0 – mean value calculated after 10 trials. Then, the relative error (RE) was estimated using the formula RE% = (AE/X0) × 100.
Standard error
A standard error ( where: SD – standard deviation; N – number of samples) is, in effect, the standard deviation of the sampling distribution of statistic. This is because the standard error is the measure of how much random variation we would expect from samples of equal size drawn from the same population.
where: SD – standard deviation; N – number of samples) is, in effect, the standard deviation of the sampling distribution of statistic. This is because the standard error is the measure of how much random variation we would expect from samples of equal size drawn from the same population.
Planimetric clinical assessment for VLUs
The study included 11 adult outpatients with VLUs (8 females and 3 males) with a mean age of 64.6 ±11.0 years (range: 47–80) and a median of 64 years. The average duration of the disorder was 15.8 ±5.2 months with a median of 8 months (range: 3–48). Five patients had two venous ulcers on each leg. The patients were treated with active compression therapy for 4 weeks. Once a week, the wound was photographed and outlined on a transparent foil to assess the progress of healing. During the observation period, 76 photos and 76 outlines on the planimetric foil were taken. The healing progress rates (total ulcer surface area [cm2], perimeter [cm]) were assessed by contact planimetry using a digitizer with dedicated CGS and non-contact planimetry using ACS, and the results were compared with each other.
In the contact planimetry method, a transparent foil was applied on the wound on which the edge of the ulcer was redrawn by a permanent marker with a 0.5 mm tip. Next, the projection of ulceration on the clean foil was redrawn. The digitizer Mutoh Kurta XGT (Altek Kurta XGT, USA) with the included computer program C-Geo (v.4.0, Nadowski, Poland) was used for measurements of the total area and perimeter.
In the non-contact planimetry method, a photograph of the wound was taken with a measuring marker (ruler with an accuracy of 1 mm), then the image was imported into AutoCad software and the area and circumference were calculated.
Statistical analysis
Data were collected in Microsoft Excel (Microsoft 2016) and Statistica software (13.3). The normality of the distribution of the data was tested by means of the Shapiro-Wilk test. We used the Wilcoxon test to examine the differences between the dimensions of the models measured using AutoCad and calipers. The reliability of measurements was assessed by the intraclass correlation coefficient (ICC). ICC values and their 95% confidence intervals were calculated based on values of 10 recordings for each wound model. The level of statistical significance was assumed at p = 0.05.
Results
Planimetric laboratory evaluation
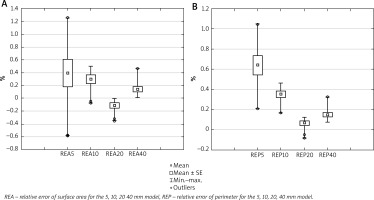
A well-planned and reliably conducted trial indicates a small value of the random error. The results of wound model measurements were presented in Table 1. The arithmetic mean, SD, SE and RE were calculated for four measurement models. The mean percentage errors were calculated for all models. The result of the percentage error measurement for the area was as follows: the arithmetic mean was 0.40% for the 5 mm model, and the mean was 0.30% for the 10 mm model, and the mean was 0.11% for the 20 mm model, and the mean was 0.30% for the 40 mm model. The result of the percentage error measurement for the perimeter was as follows: the arithmetic mean was 0.64% for the 5 mm model, and the mean was 0.35% for the 10 mm model, and the mean was 0.07% for the 20 mm model, and the mean was 0.15% for the 40 mm model. AEs and REs were calculated for all measurement models and the results showed that the largest error values were for the model with the smallest surface area and perimeter, and with the increase in the surface area and perimeter, the errors decreased. Figure 1 shows a comparison of measurement error values for four different wound models. In a direct comparison of the results of measurements using ACS and calipers, there were no statistically significant differences between the measurement areas (p = 0.493) and perimeters (p = 0.089). The reliability of measurements of the surface area and circumference of wound models was checked using the intraclass correlation coefficient (ICC). The analysis carried out for the measurements of the surface area shows a significant agreement of the measurements (p < 0.001); the reliability of the measurement was ICC = 0.999. Similar reliability results were obtained in the circumference of wound models (p < 0.001, ICC = 0.999).
Table 1
The means, standard deviations (SDs), standard errors (SEs), absolute errors (AEs) and relative errors (REs) for four different wound models
Planimetric clinical evaluation
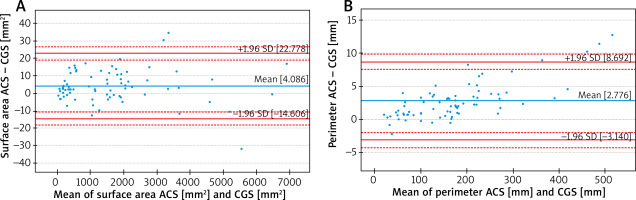
The mean ulceration area measured by the ACS (Figure 2) was 1571.36 ±1496.84 mm2 (range: 18.76–6909.79) and a median of 1394.62 mm2. The mean ulcer perimeter was 174.39 ±109.54 mm (range: 20.63–521.75) and a median of 164.26 mm. The mean ulceration area measured by the CGS was 1567.28 ±1496.84 mm2 (range: 20.00–6893.00) and a median of 1388.50 mm2. The mean ulcer perimeter was 171.62 ±107.36 mm (range: 20.00–509.00) and a median of 164.00 mm. Intergroup comparisons demonstrated statistically significant planimetric changes in favour of measurements made using the ACS, regarding all studied planimetric parameters: area (p < 0.005) and perimeter (p < 0.005). A detailed presentation of the planimetric results is shown in Table 2.
Table 2
Comparison of the results of surface area and circumference measurements of VLUs using two methods
In Figure 3 A, the Bland-Altman chart indicates that a CGS gives lower results than an ACS on average by 4.09 mm2 by surface area (the line for the mean difference was 4.09 higher than the absolute correspondence illustrated by the line of level 0). The range of the compliance interval was 33.38 mm2. Another Bland-Altman graph (Figure 3 B) for the collected perimeter data indicates that a GCS showed lower results (on average 2.78 mm) than an ACS (the line for the mean difference is 2.78 higher than the absolute correspondence illustrated by the line of level 0). The range of the compliance interval was 11.83 mm.
Discussion
There are no scientific reports on errors in geometric measurement of venous ulcers using ACS. As mentioned in the introduction, measurement errors always occur during measurements (e.g. systematic error and random error), but we can have an impact on minimizing them by choosing the right tools. Therefore, in the first part of this study, this measurement error in ACS was determined, and in the second its effectiveness compared to the contact planimetric method was shown.
The results shown in this study, for both measurement of the circumference and surface area, indicate good repeatability and reliability. The undoubted advantage of the method used is the fact that the researcher can determine the border of the wound of interest in a very precise manner. There were no significant changes between the measurements of circumference and surface area the AutoCad software and calipers in the study wound models. Eberhardt et al. in their study demonstrated high reproducibility of AutoCad software as a tool for wound contours and showed greater accuracy of contours by the researcher and evaluators for wounds greater than 10 cm2. However, the authors do not present the value of measurement errors made by the researcher and evaluators. Measurement errors were given in the study of Franek et al. from 2.7% to 13.1%, Waniczek et al. 1.46%, Foltyński et al. from 0.43% to 1.73%. In this study, errors ranged from 0.07 to 0.64% [14, 16–20].
Calibration
Calibration is a measuring element that increases the accuracy, precision of measurement and makes the researcher independent from the distance to the tested object. Eberhardt et al. used a black square measuring 3 cm × 3 cm printed on a white sheet and placed close to the ulcer as a reference object [16, 17]. Dymarek et al. [24] do not include calibration information in the work. Foltyński used 2-ruler calibration of linear dimensions for increasing accuracy and precision of the measurement with digital planimetry during wound area measurement. Foltyński has shown that the use of an appropriate reference measure significantly reduces the error of the method from 0.43% to 1.73%. This is the argument presented that complicated 3D systems do not increase the accuracy of the measurement in comparison with the digital planimetry. The same author draws attention to setting the apparatus at 90 degrees to the wound surface [19, 20, 24]. In this study, we used a ruler as a reference device and all photos were taken at an angle of 90°.
Correct determination of the wound edge as a necessary factor for correct measurement
The studies of Eberhardt et al., Foltyński, Williams et al. show that the differences in measurements are influenced by the correct identification of wound edges. From our 15 years of experience in digital planimeters, the conclusion is that the correct identification of the wound edges reduces measurement errors.
Experience in wound sizing is a very important aspect that affects measurement error. The software that automatically determines the wound is not always able to precisely define the boundaries of the wound, which makes it necessary to be corrected by the researcher. Digital planimetry is certainly a good tool for measuring the geometric dimensions of wounds as it gives small confirmed errors and is non-invasive [16, 17, 19, 20, 23, 25, 26].
Comparison with the second planimetric methods
In this study, we analysed geometrical measurements (area and circumference) of VLU, using two methods: planimetry using CGS and ACS. 76 measurements of the surface area and circumference of venous leg ulcers were made using both methods. The results obtained in both methods were compared with each other. Wilcoxon test showed significant differences between the methods used for both the surface area and circumference of the wounds. The obtained surface areas and perimeters measured with an ACS gave statistically significantly higher values compared to surface areas and perimeters measured with a CGS. An ACS gives higher values than a CGS by an average of 4.09 mm2 for the surface area; an ACS gives higher values than a CGS by an average of 2.77 mm for the perimeter (Figures 3 A and B). The obtained results are confirmed in the study of Eberhardt et al., which compared Image Tool 3.0 and AutoCAD software. The authors showed that the sizes of the ulcers showed great variance, and the intraclass correlation coefficient and agreement were excellent for both software programs [16, 17]. The use of AutoCad software gives great opportunities to enlarge the analysed wound, which significantly reduces the measurement error. To the best of our knowledge, the ALIGN command has not been used to perform geometric measurements of wounds. As we have shown in studies using wound models, the average measurement error was small, which gives us the grounds to recommend this program not only in the analysis of wounds but also other skin lesions and can be used in dermatology, surgery or orthopaedics.
We are aware of the limitations of the work, which should be noted. As we stated in the introduction, AutoCad software has already been used to examine wounds, but none of the authors reported measurement errors of the method, which was presented in this work. In addition, in the Technical note chapter, we presented a point-by-point measurement procedure using the software. The last aspect is an innovative approach to the use of AutoCad software, showing the great possibilities of this program.
Conclusions
Examination of measuring error tests, repeatability indicate that AutoCAD software is a good and reliable measuring tool. The ease of use means that it can be used to monitor the healing of chronic wounds (VLUs, PUs, BUs) in the daily medical and nursing practices as well as in the physiotherapist’s offices.