The global burden of ischemic heart disease
Ischemic heart disease is the most common cause of morbidity and mortality in Poland and worldwide. Coronary artery disease (CAD) affects around 3.5% of the population of the European Union [1]. According to IHME data, in 2017 in Poland, 4.2% of the population suffered from CAD, which was 0.1 percentage point more than in 2012 [2]. The number of new cases of CAD in Poland decreased in the years 1990–2017. It was evident in the case of male morbidity, for whom the values in 1995 were much higher than in females, and by 2017 it had dropped to a similar level. The clinical presentation of CAD ranges from chronic (stable) coronary syndromes (CCS) to various forms of acute coronary syndromes (ACS). According to the European Society of Cardiology (ESC), two types of ACS can be distinguished: ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation ACS (NSTE-ACS). The latter group comprises of two sub-groups: non-ST-segment elevation myocardial infarction (NSTEMI) and myocardial ischaemia without cell damage, known as unstable angina (UA). Acute coronary syndromes are the most frequent CAD presentation, which leads to death. ACS are also the most cost-consuming type of the ischemic heart disease, which prominently requires hospital treatment. In 2019, in Poland, expenses provided for ACS accounted for 61.4% of the value of hospital reimbursement due to the ischemic heart disease. In 2019, the total number of ACS cases recorded by the Polish National Health Fund was 102,700, the number was 19% lower compared to the data from 2014. This decrease mainly concerned the number of cases of unstable angina (by 55%, n = 30,000), whereas the number of myocardial infarctions increased by 9% (n = 6,000). Among women, an increase of 3% was noted, and by over 10% in men. The mean age of patients with acute coronary syndromes in 2019 was 66.3 years. Men dominated in the 60–74 age group, whereas predominance of women was noted in the group over 80 years of age [2]. There was also an increase in the proportion of ACS patients treated with coronary angioplasty within 7 days from the onset of symptoms. Angioplasty was most often performed in the case of STEMI (88% in 2018), in a smaller percentage of NSTEMI (64%) and unstable angina (48%). A substantial number of ACS patients were treated with a coronary artery bypass grafting (CABG) procedure within 90 days of the event. The highest percentage was observed in UA patients (14%), followed by NSTEMI (6%) and STEMI patients (3%) [2].
Early and late outcomes following acute myocardial infarction
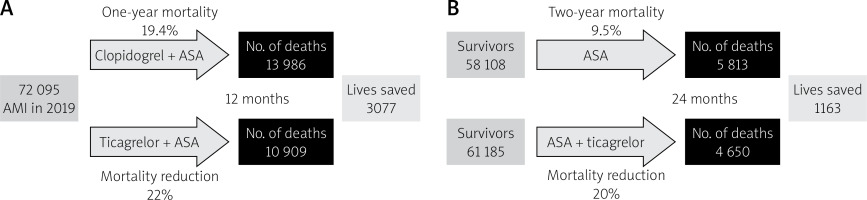
The nationwide AMI-PL database 2009–2012 revealed that among all AMI patients admitted in 2009, in-hospital mortality was as high as 10.5% and was strongly related to patients’ age [3]. The total mortality at 1 year was 19.4%, indicating that the mortality after discharge was 8.9%. As already mentioned, AMI patients who survived the first year after the event are still at increased risk of cardiovascular events.
Wojtyniak et al. have published data from the Polish nationwide AMI-PL registry that included 134,602 patients hospitalized for acute myocardial infarction (AMI) in 2009–2010 [4]. Five-year outcomes of all patients discharged alive were assessed. The AMI definition included patients with STEMI, NSTEMI and unspecified AMI. Data concerning all-cause mortality, a need for further hospitalization for cardiovascular reasons and procedures performed after discharge were collected. The outcomes were presented separately in 4 age groups: below 55, 55–64, 65–79 and above 80 years. Survival dropped the most in the first year after the index hospitalization, whereas further decline remained constant in the following years. The 5-year survival rates differ across the age groups. In males below 55 years, there was the highest survival rate, and in those above 80, the lowest one: 0.915 vs. 0.383, respectively. However, after adjustment for the overall mortality of the entire Polish population, this relationship was substantially attenuated. An even more substantial reduction in the impact of age was observed in women. However, data from the Polish registry differ from those surveyed in SWEDEHEART [5] and other European registries [6, 7]. In Poland, the absolute and relative survival rate was higher in women than in men. Whereas in other countries, this correlation was the opposite. A possible explanation of this phenomenon may be caused by poor guidelines application in clinical practice, level of education, the diversity of cardiovascular risk factors and poor management of numerous comorbidities in a real-life setting. The reported high mortality rate of AMI patients after the first year following the event was consistent with other Polish data published previously [8]. This risk significantly increases shortly after stopping dual antiplatelet therapy (DAPT), typically in most patients after 12 months following AMI [9]. An observational study of numerous patients treated with percutaneous coronary angioplasty (PCI) for AMI showed that recurrent myocardial infarction originating from a previously untreated lesion was twice higher than from a previously stented lesion [10]. Therefore, one of the goals of long-term treatment of such patients should be the identification of those at increased risk of subsequent events, for whom prolonged DAPT will bring clinical benefits. At the same time, patients at high risk of bleeding should be excluded from such an approach.
It has already been demonstrated that among various risk factors, some are vital for both ischemic and bleeding events. Lindholm and coauthors studied the impact of risk factors such as age > 65, chronic kidney disease, diabetes mellitus, multivessel coronary artery disease, prior myocardial infarction and prior bleeding on the incidence of new ischemic and bleeding events [11]. The study was based on the SWEDEHEART registry and Swedish National Patient Register that combined data obtained between 2006 and 2014. The primary outcome was the composite of MI, stroke and cardiovascular death. The majority of patients had two or more risk factors (53.5%). The authors found a strong cumulative correlation between the number of risk factors and the rate of ischemic events. With each risk factor added, there was a marked, gradual increase in the incidence of cardiovascular death, myocardial infarction or stroke. Also, a similar but less pronounced correlation with bleeding events has been found. Prior bleeding was the strongest predictor of this complication. After excluding such patients from analysis, an increasing number of risk factors remained associated with a substantial rise in the ischemic events. In contrast, the bleeding rate increased only minimally. This finding is consistent with the PRECISE-DAPT score that is recommended in ESC Guidelines for bleeding risk assessment in ACS patients and those undergoing PCI [12, 13].
The role of antiplatelet therapy in mortality reduction following acute myocardial infarction
Dual antiplatelet therapy (DAPT) is a foundation of successful coronary artery disease management. DAPT is recommended according to ESC guidelines for 6 months following elective PCI and for 12 months following ACS. It has been documented that more potent and predictable P2Y12 inhibitors – prasugrel and ticagrelor, compared to clopidogrel, significantly reduce the incidence of major adverse cardiovascular events (MACE) in broad-spectrum ACS patients [14, 15]. In addition to lowering composite ischemic endpoint, ticagrelor significantly reduced all-cause and cardiovascular mortality [15]. This beneficial effect has been recently confirmed in a network meta-analysis of 52,816 ACS patients from 12 randomized trials [16]. The long-term use of ticagrelor in patients with previous myocardial infarction was also related to a significant reduction in MACE [17]. In patients who had a myocardial infarction 1 to 3 years earlier, the addition of ticagrelor on top of a low dose of aspirin resulted in a significant reduction in the composite endpoint of cardiovascular death, myocardial infarction, or stroke at the expense of a small but significant increase in bleedings. No excess fatal bleeding or intracranial hemorrhage has been observed. In the approved European label, ticagrelor at a dose of 60 mg b.i.d. was associated with a significant reduction in cardiovascular and all-cause death – hazard ratio 0.71 (0.56–0.90) and 0.80 (0.67–0.96), respectively [18]. The EU label group consisted of patients who were randomized ≤ 2 years from qualifying MI or ≤ 1 year from stopping DAPT.
Given the well-documented positive effect of ticagrelor on mortality and its major underuse in ACS patients in Poland, it is worth calculating the hypothetical number of deaths that might be prevented by using ticagrelor instead of clopidogrel. These are theoretical calculations as it will never be possible to replace clopidogrel for everyone because of contraindications or side effects. The calculations assume the number of patients who had AMI in Poland in 2019 because the statistics for 2020, due to the COVID-19 pandemic, differ significantly from previous years. The early benefit (12 months) was calculated based on the results of the PLATO study [15], whereas the long-term effect (another 24 months) was based on the approved European label, patients from PEGASUS-TIMI 54 study [18]. As shown in Figure 1 A, the strategy of replacing clopidogrel with ticagrelor in all patients with AMI in Poland would result in more than three thousand lives saved within the 12 months following AMI. Moreover, another 1163 deaths could be avoided by adding a low dose of ticagrelor to ASA in the following 2 years (Figure 1 B). These hypothetical calculations should be corrected for the actual use of antiplatelet drugs in patients with myocardial infarction in Poland. The recent analysis of the PL-ACS registry shows that in 2020, ticagrelor was used in less than 40% of patients in the first year after AMI and in less than 5% of patients in > 12 months post-AMI.