Introduction
Cardiovascular diseases rank first on the list of causes of death, both in Poland and in the world. Although there has been a significant improvement in reducing mortality due to them for several years, they still account for 49% of all deaths in Europe. In Poland, this percentage varies between 35 and 40% [1,2].
The most common cardiovascular diseases include coronary artery disease and its complications, including heart failure due to myocardial ischemia [1,2]. It is estimated that in recent decades the number of patients with heart failure has doubled, which is why it has become a social problem. This may be related to the aging of the population, but also to the increasingly effective treatment of cardiovascular diseases and longer survival of patients in this group [3]. The incidence of heart failure (HF) depends on age, and the highest incidence is in people over 70 years of age, among whom the percentage of patients with this disease exceeds 10% and increases rapidly after the age of 75, reaching up to 20% [4]. Based on epidemiological data, it was found that HF occurs in about 10 million people in Europe and in about 800,000 in Poland, and according to some sources it reaches even 1 million [3]. The rapidly increasing number of cases of HF is the result of medical progress, especially invasive cardiology. Thanks to more effective treatment of myocardial infarction, more patients survive an acute coronary event, but unfortunately, many of them develop heart failure [5].
The prognosis in heart failure depends, among other things, on the number and frequency of hospitalizations due to decompensation – the more there are, the worse the prognosis. Unfortunately, in Poland the number of hospitalizations due to heart failure significantly exceeded the number of hospitalizations due to myocardial infarctions. The rate of hospitalization for this reason in our country is the highest in Europe and amounts to over 500 per 100,000 inhabitants, while the European average is 200-250 per 100,000 [6]. Poland is one of the leaders among the countries of the Organization for Economic Co-operation and Development (OECD) in terms of expenditure on heart failure treatment, and its results are much worse than in other countries.
Treatment of chronic heart failure should be comprehensive, and its goal is to reduce mortality and severity of disease symptoms, as well as to improve the quality of life of patients in this group. The most important elements of non-pharmacological treatment include:
– limiting sodium/salt intake to 2-3 grams per day,
– limiting fluid intake to 1.5-2 liters a day, – reducing alcohol consumption (two units per day for men and one unit per day for women; one unit of alcohol corresponds to 10 ml of pure alcohol),
– smoking cessation,
– regular, moderate physical activity that improves the efficiency of the respiratory muscles, reduces the feeling of shortness of breath and increases the maximum exercise capacity,
– regular weight control to quickly notice signs of overhydration,
– avoiding certain medications (e.g. ibuprofen, ketoprofen, glucocorticoids, class I antiarrhythmic drugs, lithium salts and tricyclic antidepressants),
– vaccination against influenza and pneumococci, – avoiding travel to places located at an altitude of >1500 meters above sea level or with a hot and humid climate [4,7-9].
Cardiac rehabilitation of patients with heart failure is also a recognized form of non-pharmacological treatment. It should be implemented immediately after initial stabilization of the patient’s condition after an acute cardiac incident. Kinesiotherapy in patients with heart failure should include three types of training: endurance, respiratory and resistance with elements of stretching training. Planning of training loads is based on the patient’s current physical capacity, determined by functional tests. In addition, the patient’s age and lifestyle before the onset of the disease as well as his/her personal preferences should be taken into account. Individual exercise tolerance measured with the Borg scale is also important – the patient should not exceed the perceived intensity of exercise, which is defined as moderate (10/20–14/20 according to the Borg scale). Training loads should be selected individually [10].
In addition to invasive and pharmacological treatment, a very important element is the education of the patient and his/her family, which should be conducted by a group of people taking care of a patient. A doctor, a nurse, a cardiological rehabilitation specialist and a psychologist are valuable source of information. Moreover, not occasionally above-mentioned specialists provide important information regarding a need of patient lifestyle change. However, does education of patients with heart failure make sense and contribute to a real improvement in their pro-health behavior after leaving the hospital?
Aim of the work
The aim of the study was to check whether the education in the field of pro-health behaviors, with particular emphasis on physical activity, conducted among patients with heart failure has a positive effect on changing their lifestyle.
Material and methods
The study included 78 (100%) patients hospitalized due to heart failure decompensation (NYHA IIIIV), who underwent education in the field of pro-health behaviors. All patients qualified for the study were diagnosed with heart failure in the course of coronary artery disease (myocardial ischemia). Decompensation of heart failure was confirmed based on the assessment of the patient’s clinical condition based on the NYHA (New York Heart Association) scale, as well as echocardiographic and laboratory tests. Patients included in the study were in class III or IV of the scale mentioned above.
The study was approved by the Bioethics Committee of the Medical University of Silesia in Katowice (PCN/0022/KB1/36/21), and all participants gave informed consent to participate in the study.
Before the start of the study, each respondent received an identification number that allowed to compare the results obtained in the decompensation stage and in the long-term follow-up. Original questionnaires were used to conduct the study, consisting of questions of comparable content regarding the discussed topic and the general characteristics of the respondents.
Questions about quality of life and perception of one’s own health were borrowed for the purposes of the study from the standardized WHOQOL-BREF questionnaire and conducted in accordance with its methodology. Reliability analysis showed high (Cronbach’s α=0.99) internal consistency of the analyzed questions in the questionnaire used. Completion of the questionnaire was completely anonymous and voluntary.
Educational activities included a conversation and providing each patient with information on pro-health behaviors recommended for patients with heart failure in the form of a brochure, with particular emphasis on the benefits of physical activity One researcher was appointed to carry out educational activities, thus ensuring uniformity of information related to health-related activities for all examined patients.
Patients hospitalized due to decompensation of heart failure received the first questionnaire to complete, which they returned to the person conducting the examination. Then, each patient had an individual educational conversation and received a brochure with the most important information on the secondary prevention of heart failure, including recommendations on physical activity, the use of stimulants, and regular blood tests, which he/she could take home. All the activities described above were carried out during the patient’s stay in hospital, i.e. before qualifying for cardiac rehabilitation. After 4-8 weeks (during which the patients had time to implement the recommended health-promoting behaviors), during a follow-up visit at the hospital clinic, patients completed a second questionnaire with questions about their healthy habits identical to the first one.
In order to examine the impact of education on health behaviors of the examined patients, the Chi2 test of independence was used, and statistical analyzes were carried out using the Statistica 13.3 program.
Results
Table 1 presents the general characteristics of the study group of patients with heart failure.
Table 1
General characteristics of the study group of patients with heart failure
Men accounted for more than 3/4 (59; 75.64%) of the study group, and the largest group (44; 56.41%) had primary education. The mean age was 68.10±8.93 years.
Figure 1 presents the characteristics of the study group of patients with heart failure, taking into account the self-assessment of improvement in their own pro-health behaviors of respondents undergoing education.
Figure 1
Self-assessment of improvement in pro-health behaviors of the surveyed patients with heart failure undergoing education
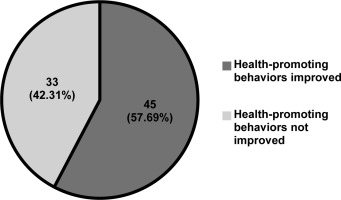
Almost 60% (45; 57.69%) of the surveyed patients claimed that their pro-health behaviors had improved after education.
Table 2 presents the characteristics of the study group of patients with heart failure, taking into account health-promoting behaviors of patients before and after education.
Table 2
Characteristics of the study group of patients with heart failure, including pro-health behaviors before and after education
Smoking was declared by about 1/3 of the respondents (25; 32.05%) at the stage of decompensation, and only about 9% (7; 8.97%) in the long-term follow-up (Chi2=12.738; p=0.0004). However, a disturbing decrease in the number of patients with regular blood pressure monitoring was observed (73; 93.59% vs. 61; 78.21%).
Table 3 presents the characteristics of the study group of patients with heart failure before and after education, including physical activity and the use of supervised cardiac rehabilitation.
Table 3
Characteristics of the study group of patients with heart failure before and after education, including physical activity and the use of supervised cardiac rehabilitation
About 85% (66; 84.62%) of patients declared taking up physical activity before education, but among the discussed respondents almost 3/4 (58; 74.36%) did not perform physical exercises, e.g. gymnastics. Regular use of cardiac rehabilitation before education was declared by about half of the patients (41; 52.56%), and less than 45% (34; 43.59%) after education.
Figure 2 presents the characteristics of the study group with heart failure taking into account the regularity of body weight control, and in Figure 3 the daily fluid balance among patients after education.
Figure 2
Characteristics of the study group of patients with heart failure, taking into account the regularity of body weight control by the subjects after education
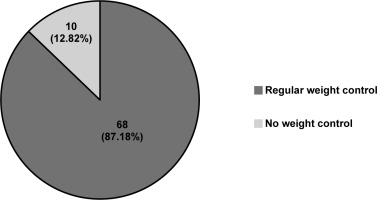
Figure 3
Characteristics of the study group, taking into account the regularity of fluid balance checks by the subjects after education
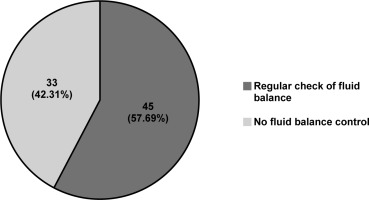
Almost 90% (68; 87.18%) of the examined patients regularly monitored their body weight, but over 40% (33; 42.31%) did not regularly monitor their fluid balance. Figure 4 presents the characteristics of the study group of patients with heart failure, taking into account the respondents’ opinions on the need to conduct health education.
Figure 4
Characteristics of the study group of patients with heart failure, taking into account the respondents’ opinions on the need to conduct health education
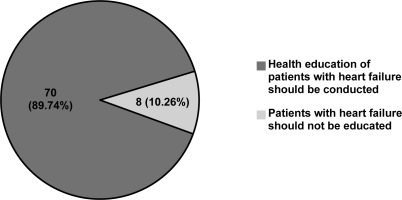
Only about 10% (8; 10.26%) of the respondents claimed that there is no need to educate patients with heart failure.
Table 4 presents the characteristics of the study group of patients with heart failure before and after education, including the assessment of the quality of life using the WHOQOL-BREF questionnaire. The characteristics of the study group of patients with heart failure before and after education, including the assessment of their own health using the WHOQOL-BREF questionnaire, are presented in Table 5.
Table 4
Characteristics of the study group of patients with heart failure before and after education, taking into account the results of assessing the quality of life using the WHOQOL-BREF questionnaire
Table 5
Characteristics of the study group of patients with heart failure before and after education, taking into account the results of the assessment of their own health using the WHOQOL-BREF questionnaire
Over 60% (52; 66.66%) of respondents with heart failure before education assessed their quality of life as bad, while almost 1/5 (14; 17.95%) of respondents assessed their health after education as good. Comparison of the study group before and after education, both in terms of quality of life and satisfaction with health, confirmed statistically significant differences before and after education in both examined parameters (Chi2=70.609, p<0.001*).
Discussion
In our study, over 3/4 (59; 75.64%) of the study group were men, and the largest group of respondents (44; 56.41%) had primary education. The mean age was 68.10±8.93 years. As described in the methodology, all patients (78; 100%) underwent education in the field of pro-health behaviors.
The results of many systematic reviews and meta-analyses show that regular physical training improves exercise capacity and health status, and reduces the number of hospitalizations of patients due to decompensation and heart failure. Long et al. reviewed the scientific literature on cardiac rehabilitation and, based on 44 studies involving a total of 5783 patients with heart failure, concluded that one of the most important benefits of rehabilitation of patients with heart failure was the reduction of the risk of rehospitalization [11]. There is also evidence that in patients with preserved left ventricular ejection fraction, exercise training had many benefits, including improved exercise capacity as measured objectively by assessing peak oxygen uptake, improved quality of life, and diastolic function as assessed by echocardiography [12]. In the study, physical activity was declared by about 85% (66; 84.62%) of patients with heart failure before education, but almost 3/4 (58; 74.36%) did not perform physical exercises, e.g. gymnastics. Regular use of cardiac rehabilitation before education was declared by about half of the patients (41; 52.56%), and after education – less than 45% (34; 43.59%). Unfortunately, there was no statistically significant difference between the above-mentioned results, which means that education on the benefits of physical activity and rehabilitation did not bring positive effects in the study group in the form of increasing the aforementioned pro-health activities.
Sallis et al. suggested that in all patients admitted to healthcare facilities, especially those with heart failure, the level of physical activity should be recorded as one of the vital signs for routine assessment and appropriate counseling or subsequent referral to cardiac rehabilitation [13].
Regular physical activity is considered as a valuable therapeutic method in the treatment of patients with heart failure. Taking it significantly improves exercise tolerance, which cannot be achieved using only pharmacological treatment. It also has a positive impact on the quality of life and clinical outcomes of patients. Unfortunately, despite increasing scientific evidence, most patients do not undertake adequate physical activity [14]. Additionally, some patients which do not feel responsible for their health and neglect health-promoting behaviors, including regular physical activity. Abandonment of health-promoting activities can be observed especially when the patient’s general health condition improves [15]. The above-mentioned “complication” of improvement in health condition was observed among the respondents of our own study, where in the long-term follow-up (4-8 weeks after hospitalization), the number of people exercising regularly has decreased. Obtained results were surprising and it may be worth conducting similar studies on a larger group.
The study by Kamimura et al. showed that frequent hospitalizations due to heart failure were strongly associated with smoking by patients, as well as smoking in the past and the number of cigarettes smoked, compared to non-smokers [16]. Researchers Ding et al. showed a relationship with smoking with an increased risk of morbidity and decompensation of heart failure, as well as between smoking cessation and reduction of this risk, confirming that smoking is an important, modifiable cardiovascular risk factor [17]. Similar conclusions were drawn by Lu et al. [18]. Following the results of Biondi-Zoccai et al., in which the researchers stated that smoking cigarettes was one of the main causes of heart failure in their study group [19]. It can be suggested that the risk of illness and decompensation can be mitigated by stopping smoking altogether [19]. In our study, smoking was declared by about 1/3 of the respondents (25; 32.05%) before education and about 9% (7; 8.97%) after education (Chi2=12.738; p=0.0004). The result was statistically significant, so it can be said that after the education, the number of people declaring smoking significantly decreased.
Although there are studies showing the cardioprotective effect of moderate alcohol consumption, especially red wine [20-22], higher alcohol consumption may contribute to myocardial damage, atherosclerosis, and, consequently, heart failure. According to many studies and studies, it is recommended to limit or avoid excessive alcohol consumption in heart failure [23,24]. In turn, taking into account proper nutrition, there are many studies in which the benefits of the Dietary Approaches to Stop Hypertension (DASH) diet and the Mediterranean diet in the prevention of secondary heart failure have been noticed [25]. The studies by Bechthold et al. showed that the optimal consumption of products that are most often recommended in the above-mentioned diets, i.e.: whole grains, vegetables, fruits, nuts, legumes, dairy products, fish, red, processed meat, eggs, significantly reduced risk of cardiovascular diseases, including heart failure [26]. In our study, no statistically significant difference was found between alcohol consumption (p=0.237), and nutrition (p=0.85) of the surveyed patients before and after education.
In our study, a statistically significant difference (p=0.02*) was noted between the number of respondents declaring their willingness to be vaccinated against influenza before education (22; 28.21%) and after education (10; 18.82%). This decline in interest in vaccination is worrying, particularly as there are reports that exacerbation of pre-existing heart failure may be caused, among others, by influenza infection, and vaccinations reduce the risk of morbidity and death of patients [27,28]. It is possible that in Poland there is still a trend of “reluctance” to vaccination due to the widespread activities of anti-vaccination movements [29].
In our own study, a disturbing, statistically significant (p=0.006*) reduction in the number of patients regularly controlling their blood pressure was observed (73; 93.59% vs. 61; 78.21%). This is important because regular blood pressure measurements allow for proper control of hypertension, which is the most common cause of development and decompensation of heart failure [4,7-9]. According to the recommendations of the Polish Society of Hypertension (PTNT) regarding blood pressure measurement, patients with high blood pressure should measure it regularly, as recommended by the attending physician, several times a week, or even every day [30].
When discussing the effects of the education conducted among the surveyed patients, it should be mentioned that almost 90% (68; 87.18%) declared regular control of their body weight, but over 40% (33; 42.31%) did not regularly control their fluid balance. Weight control in heart failure is important but not sufficient without controlling fluid balance. Weight fluctuations in patients with heart failure are common due to the occurrence of edema in periods of decompensation [4,7-9]. Thanks to regular body weight control, you can quickly assess its sudden increase indicative of the beginning of decompensation. However, without fluid balance control, it is difficult to clearly determine whether the described changes result from changes in diet and increased body fat, or from edema.
In our own study, almost 60% (45; 57.69%) of respondents believed that their pro-health behaviors had improved, and only about 10% (8; 10.26%) claimed that there was no need to educate patients with heart failure. In addition, 60% (52; 66.66%) of respondents with heart failure before education assessed their quality of life as bad, while almost 1/5 (14; 17.95%) of respondents after education assessed their health as good. The comparison of the study group before and after education, both in terms of quality of life and satisfaction with health, confirmed statistically significant differences in both parameters before and after education (Chi2=70.609, p<0.001). At this point, it should be emphasized that the discontinuation of compliance with the recommendations, despite the education, could have resulted from the fact that the patients felt better in the long-term follow-up. They did not feel burdensome ailments or the need to control their own health, e.g. to perform regular blood pressure measurements. It is worth emphasizing that Tables 4 and 5 contain identical values. This is not an error during the preparation of the manuscript, but the result of the analyzes performed. The occurrence of identical numerical values in questions regarding self-assessment of health and quality of life may indicate a strong connection between the above-mentioned variables.
The limitations of the study include a small number of respondents and only two surveys. Nevertheless, despite the observed improvement in the quality of life and satisfaction with health, other results mentioned above showed that conducting extensive education, not only in terms of the benefits of physical activity, but also on the use of a proper diet, not smoking, limiting alcohol consumption, the use of preventive vaccinations, in particular against influenza, in this group of patients is very important, because the patients still do not comply with many recommendations regarding non-pharmacological treatment of heart failure.
Patients should be made more and more aware of the positive effects of changing their lifestyle to a pro-health lifestyle in order to eliminate modifiable risk factors, improve their quality of life, and prevent premature death from cardiac causes.
Conclusions
Education of patients with heart failure was associated with increased implementation of pro-health behaviors, but only in the area of smoking cessation and weight control, but did not affect physical activity, nutrition and alcohol consumption.
Improvement of the quality of life and satisfaction with one’s own health in the long-term follow-up of the surveyed patients with heart failure, unfortunately, could have contributed to the abandonment of the implementation of pro-health behaviors discussed during the education.
There is a need for systematic education of patients with heart failure in terms of the benefits of changing their lifestyle to a healthy lifestyle, as these patients were reluctant to eliminate risk factors contributing to the exacerbation of the disease and, consequently, to its progression and death.