Introduction
Worldwide, breast cancer is a frequently diagnosed cancer in the female population with high survival rates. According to GLOBOCAN 2018, most countries have experienced an increasing trend in breast cancer incidence regardless of whether the female population is older or younger; therefore, it is one of the causes of cancer morbidity and mortality [1]. In 2020, there were more than 2.3 million new cases and 685,000 deaths from breast cancer [2]. A large number of breast cancer survivors have to face the consequences of the disease, which can adversely affect their quality of life. The most common problems in breast cancer are pain, fatigue, insomnia, lymphoedema, cognitive impairment or depression, which tend to occur in combination [3,4]. Pain is one of the most feared and persistent clinical symptoms of cancer, which can occur in people at an early stage, but also several years after survival or cessation of treatment. It is estimated that up to 30% of women with breast cancer suffer from chronic pain, even ten years after treatment [5]. The prevalence of cancer pain is high, so it should not be underestimated and should be addressed from the beginning of its course, not only if it is severe, because patients suffering from pain respond less well to cancer treatment. Women diagnosed with advanced breast cancer may also feel pain in other areas of the body away from the breasts.
The etiology of pain can be due to the release of inflammatory mediators, invasion into other tissues (bone, muscle, nerve structures). Similarly, treatments potentiate pain, including surgery, radiotherapy, chemotherapy, immunotherapy, and hormone therapy [6,7]. Women with hormone receptor-positive breast cancer usually take hormone therapy to reduce the risk of a relapse. The most well-known types of hormone therapy drugs are tamoxifen (TAM) and aromatase inhibitors (IA), which cause unpleasant adverse reactions. Hot flushes and the risk of blood clots can occur when taking TAM, as well as muscle and joint pain with IA. Other less common ones are heart problems, osteoporosis, and bone fractures. To reduce bone and joint pain, analgesics belonging to the group of antiphlogistics, antirheumatic drugs, are prescribed. Some nonpharmacological techniques have been shown to relieve bone pain: acupuncture, chiropractic, massage, music therapy and hypnosis. Physical therapy can also relieve painful areas [8].
Treatment of early-stage breast cancer may include taxane chemotherapy, which is often associated with chemotherapy-induced peripheral neuropathy (CIPN), which can negatively affect quality of life [9]. Symptoms of CIPN include paresthesia and pain, depending on the type and severity of nerve pathway involvement. The incidence of CIPN in breast cancer patients ranges between 30% and 97%. Taxanes are characterized by distal symmetrical paresthesia to burning pain in the extremities, which may be transient and later persistent, with spontaneous improvement months to years after the end of therapy. The plantar region of the feet and the tips of the toes are also affected. Sensory symptoms, including tremors and decreased sensitivity to heat and touch, are also common. Patient may feel uncomfortable with common tasks requiring fine motor skills. Symptoms of CIPN have been reported by women even several years after treatment [10]. Currently, a number of drug groups such as antidepressants, anticonvulsants and narcotic analgesics are used to treat CIPN in cancer patients [11]. The American Society of Clinical Oncology (ASCO) does not yet recommend prescribing therapeutics other than duloxetine [10,11].
Some women who have had breast surgery may develop an unpleasant set of symptoms called postmastectomy pain syndrome. Soreness may occur immediately after surgery or several days, weeks or months apart. The pain is most commonly described as tightening, clenching and burning, particularly around the surgical scar on the chest, in the axilla, and on the back of the shoulder. Women also often complain of a feeling of numbness or the presence of foreign tissue around the scar. Early postoperative rehabilitation, gentle massage, and exercises to the shoulder area may be effective in preventing the pain syndrome [12]. Phantom breast pain may also occur in women after mastectomy. Women experience pain, discomfort, itching, tingling, pressure, and a pricking sensation. Phantom breast pain is more likely to be experienced by women who experienced pain before mastectomy [13]. Postoperative pain in BC patients also has a significant impact on a woman’s psychological and physical functioning [14,15]. It can lead to reduced activities and social isolation. Although it might seem that avoiding activities such as exercise and social opportunities should allow for rest and recovery, on the contrary, scientific data show that moderate activity and continued engagement in daily activities is best for preventing and managing chronic pain [16].
Assessment of the patient’s medical condition and critical evaluation of pain and its characteristics is the basis of pain management. Pharmacotherapy uses both opioid and non-opioid analgesics in breast cancer patients, but non-pharmacological therapies are gaining popularity in the complex management of pain.
Aim of the work
The aim of this review study is to present non-pharmacological interventions used for effective pain management in breast cancer patients.
Research Question: Do non-pharmacological interventions reduce pain in breast cancer patients compared with breast cancer patients undergoing other interventions to reduce pain?
Methods
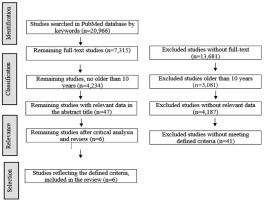
The PubMed electronic database was searched for studies. The search was based on the following keywords: non-pharmacological AND intervention AND pain AND breast cancer OR breast neoplasms. Inclusion criteria were patients with breast cancer or having undergone breast cancer with manifestations of pain, randomized controlled trials and clinical trials, full-text studies in English language, not older than 10 years.
Literature review results
There were 20 996 records retrieved. Initial sorting excluded studies that did not meet the full-text criterion (n=13,681). Then studies older than 10 years were excluded from the remaining 7,315 studies, leaving us with 4,234 studies. Content with duplication was removed, and the remaining articles were sorted and assessed by title and abstract (n=4,187). A total of 41 articles were finally considered after careful review of the quality and content of each. After critical review and analysis of the remaining studies, articles that did not meet the defined criteria were excluded and six studies were selected (Figure 1).
The following data were included in the study overview: authors of the study, year of publication, location of the study, characteristics of the respondents, type of pain and intervention, aim and type of study. Individual information is presented in Table 1.
Table 1
Review of studies
| Author, year and country | Sample characteristics | Type of pain, type of intervention | Aim and type of study | Main results |
|---|---|---|---|---|
| Carson et al., 2020, UK [17] | 48 women (age ≥ 18 years) with metastatic breast cancer (stage IV), randomized to either Yoga (n=30) or a supportive interventiongroup (n=18). During the study, participants continued to receive their usual medical care. | Somatic pain, Mindful Yoga | To determine if daily pain changed significantly during the Mindful Yoga program in women with metastatic breast cancer compared to a control group (RCT) | Pain levels were low in women in both groups; no differences were found in the effect of the intervention on daily pain. Women practicing Yoga for longer periods of time on two consecutive days perceived lower pain. Meditation showed the strongest relationship with lower daily pain (p=0.001**). |
| Peppone et al., 2015, USA [18] | 167 women (21 years and older) who are breast cancer survivors receiving hormone therapy (IA or TAM). | Somatic pain (arthralgia myalgia), Yoga for Cancer Survivors (YOCAS)© | To investigate the effectiveness of Yoga to improve musculoskeletal symptoms in breast cancersurvivors currently receiving hormone therapy (RCT) | Among breast cancer survivors on hormone therapy, the YOCAS©® brief community intervention significantly reduced overall pain, muscle pain, and physical discomfort (p≤0.05*). |
| Tsai et al., 2021, Taiwan [19] | 52 female breast cancer survivors (41-70 years) on hormone therapy for IA were divided into 2 groups: 1. received first a 6-week Yoga intervention and then a 6-week massage intervention, and 2. received the interventions in reverse order, at the same weekly intervals. | Somatic pain (arthralgia), Mindful Yoga | To evaluate the therapeutic effects of Yoga and massage on knee pain associated with IA (RCT) | Results showed that Yoga was superior to massage intervention, significantly reduced knee joint pain associated with IA (p<0.05*). |
| Hershmanet al., 2018, USA [20] | 206patientswho completed the study were postmenopausal women with stage I-III breast cancer who were receiving stage IA hormone therapy. | Somatic pain (arthralgia), acupuncture | To investigate the effect of acupuncture on reducing IA-related joint pain (RCT) | Actual acupuncture resulted in a statistically significant reduction in joint pain at 6 weeks compared to the sham or control group (p=0.01). |
| Lu 2019, South Korea [11] | 40 women with stage I-III breast cancer after adjuvant taxane-containing chemotherapy were enrolled and randomized 1:1 to the immediate acupuncture group or the delayed acupuncture control group. | Neuropathic pain, acupuncture | To assess the feasibility, safety, and effect of acupuncture intervention on CIPN (RCT) | Women with CIPN after adjuvant taxane therapy experienced significant improvement in neuropathic symptoms from an 8-week acupuncture treatment regimen compared with a control group (p=0.01*). |
| Mao et al., 2014, USA [21] | 67 postmenopausal women (41-76 years of age) with stage I-III breast cancer who were receiving hormone therapy (IA) were enrolled. | Somatic pain (arthalgia), electroacupuncture | To evaluate the short- term effect and safety of electroacupuncture for IA-related arthralgia compared with usual care (RCT) | The mean reduction in pain severity was greater in the electroacupuncture group than in the control group (p=0.0004***). |
Yoga practice predicts improvement in daily pain in women with metastatic breast cancer (MBC)
Yoga is a physical and mental discipline that promises to reduce the pain of cancer. In a study by Carson et al. [17], pain scores were collected over the duration (8 weeks) of the intervention period from 48 women with MBC, randomized to a mindful Yoga intervention group (n=30) and a supportive Yoga intervention group (n=18). Mindful Yoga was originally developed to address symptoms of pain, fatigue, and emotional distress related to cancer. Mindful Yoga included meditation (25 minutes), gentle postures (40 minutes), breathing techniques (10 minutes), presentation of Yoga principles (20 minutes), and group discussion (25 minutes). The intervention support group participated in discussions about the most common problems and themes that arise in patients confronted with MBC (concerns about change: body image, physical functioning, mortality, future plans). During the 8-week period, daily pain measurements were alternately recorded in both groups. Results showed no differences between groups in the effects of treatment on daily pain, but when patients spent more time practicing Yoga (meditation, breathing, postures) for two consecutive days, they were more likely to experience less pain the following day. This relationship was observed for meditation practice (p =0.001**) and breathing practice (p=0.026*), both of which independently demonstrated a significant dose-response relationship for daily pain.
Effect of YOCAS©® Yoga on musculoskeletal symptoms in breast cancer survivors on hormone therapy
Peppone et al. [18] confirmed the efficacy of the standardized YOCAS© Yoga intervention to improve musculoskeletal symptoms (general pain, muscle pain, physical discomfort) compared with standard care. The sample consisted of 167 women taking IA (n=95) or TAM (n=72) who suffered from musculoskeletal symptoms. The standardized YOCAS© program consisted of two forms of Yoga: gentle hatha Yoga and restorative Yoga. The intervention took place in a group setting, twice a week for 75 minutes for 4 weeks, for a total of eight Yoga sessions. The control group without the Yoga intervention continued with a significantly greater percentage of Yoga participants experienced a reduction in total body pain (Yoga = 88.0% vs. control group the standard care provided by the oncologists) and was followed for the same amount of time. A significantly greater percentage of Yoga participants experienced a reduction in total body pain (Yoga = 88.0% vs. control group 56.7%; p=0.02*). There was also a significant improvement in the physical sub score of the FACIT-F (Yoga = 78.9% versus control group 60.0%; p=0.01*) and in the physical sub score of the MFSI-SF (Yoga = 66.2% versus control group 52.9%; p=0.09) in the Yoga group of participants.
Yoga in the treatment of knee joint pain associated with IA in female breast cancer survivors
Tsai et al. [19] in their study evaluated the efficacy of Yoga versus massage for the relief of knee joint pain associated with IA. Women (n=60) were assigned to two groups that underwent both interventions (Yoga and massage). One group (n=30) first underwent a 6-week Yoga intervention, followed by a 2-week rest period, and after rest, they underwent a 6-week home massage. The second group (n=30) underwent the interventions in the reverse order, namely a 6-week home massage, followed by a 2-week break, and then a 6-week Yoga intervention. Yoga classes (Mindful Yoga) were scheduled twice weekly with 60-minute sessions/classes. Treatment efficacy was assessed at baseline, post-intervention, and post-massage exposure using the Western Ontario and McMaster University Osteoarthritis Index Scale (WOMAC) and plasma cytokine levels. The WOMAC score for IA-related knee pain decreased after Yoga in the first group (p<0.05*) during the intervention period. However, there was no significant change in pain in the initial massage group. WOMAC pain scores also decreased after 1-week rest and 6-week Yoga exposure in the initial massage intervention group. In the first Yoga-initial group, WOMAC scores worsened after one-week’s rest despite undergoing a six-week massage, suggesting that the benefits of Yoga are not sustained even at eight weeks. Changes in plasma cytokine levels were not observed for either intervention used.
Effect of acupuncture on IA-related joint pain in women with early-stage breast cancer
Hershman et al. [20] investigated the effect of acupuncture versus sham acupuncture and a control group without acupuncture on the reduction of IA-related joint pain. Postmenopausal women with early-stage breast cancer were randomized to a real acupuncture group (n=110), a sham acupuncture group (n=59), or a control group without acupuncture (n=57). The real and sham acupuncture intervention consisted of twelve 30- to 45-minute acupuncture sessions for six weeks (two sessions per week). The control group did not undergo any intervention for 24 weeks. The difference was monitored at the end of six weeks by assessing the mean score using the Brief Pain Inventory-Worst Pain (BPI-WP) tool. There was a difference of 0.92 points (p =0.01*) between the actual acupuncture group and the sham acupuncture group, and a difference of 0.96 points (p=0.01*) between the actual acupuncture group and the control group. After twelve weeks, patients randomized to the real acupuncture group had a statistically significant improvement in mean pain, but no significant improvement in pain interference, pain severity, or worse stiffness compared with the sham acupuncture group. Compared with the control group, patients randomized to the real acupuncture group at week 12 had improvement in pain by all BPI measures (p≤0.003**).
Acupuncture for peripheral neuropathy in breast cancer survivors
Lu et al. [11] investigated the benefit of acupuncture in breast cancer survivors with chemotherapy-induced parietal neuropathy (CIPN) symptoms. Forty women with breast cancer after taxane-containing adjuvant chemotherapy were randomized into an immediate acupuncture group (n=20) and a delayed acupuncture control group (n=20). Immediate acupuncture patients received eighteen sessions of 30 minutes each over eight weeks, with no other intervention afterwards. Patients in the second group first received usual care for the first eight weeks, followed by nine sessions of acupuncture over eight weeks. The effectiveness of the intervention was assessed using the Patient Neurotoxicity Questionnaire (PNQ) and other measurement tools and compared at baseline and at week eight of the implemented intervention. The mean PNQ sensory score decreased by 1.0±0.9 points between baseline and outcome (at week eight) in the immediate acupuncture group and by 0.3±0.6 points in the control group (p=0.01*), indicating that the acupuncture intervention led to a significant reduction in CIPN sensory symptoms compared to the control group. After eight weeks, the mean motor PNQ scores were not significantly different between the two groups. After eight weeks, participants randomized to the acupuncture group also experienced a significant improvement in CIPN quality of life compared with participants in the control group, as assessed by the FACT-NTX (p=0.002**) and QLQ-C30 (p =0.03*) questionnaires, as well as significant reductions in pain severity (p=0.03*), pain interference (p =0.03*), and average pain (p=0.01*).
Effect of electroacupuncture for arthralgia related to IA use in women with breast cancer
Mao et al. [21] conducted a study of electroacupuncture (n=22) versus a control group without electroacupuncture (n=23) and simulated acupuncture (n=22) in 67 women with breast cancer who reported arthralgias associated with IA. Interventions were applied twice weekly for two weeks, then once weekly for an additional six weeks, for a total of ten electroacupuncture sessions in during eight weeks. The change in pain severity scores, as measured by the Brief Pain Inventory (BPI) pain scale, was compared at the end of the eighth week of intervention with baseline score. Other parameters were also assessed: upper limb stiffness and functional limitations, physical performance, balance, and endurance. The results showed that at week eight, the BPI pain scale score decreased statistically significantly more in the electroacupuncture group than in the control group (-2.2 points versus -0.2 points), and the mean difference between the groups was 1.9 points (p=0.0004***). The electroacupuncture group also had a statistically significant reduction in their pain-related interference score than the control group (-2.0 points versus 0.2 points), and the mean difference between the groups was 2.2 points (p=0.0006***). Compared with the baseline, the electroacupuncture group achieved a 43.1% reduction in pain intensity and a 52.6% reduction in pain-related interference during the eight-week intervention period. The electroacupuncture group also experienced statistically significant improvements in lower extremity pain (p=0.0009***), stiffness (p=0.0014**), and functional limitations (p =0.0005***), as measured by the WOMAC index. There was an equally statistically significant improvement in upper limb disability scores as measured by the DASH scale (p=0.005**).
Discussion
Pain is a common symptom that afflicts and debilitates women with breast cancer during and after treatment. Post-operative pain, cancer metastasis pain, treatment side effects, and other breast cancer related pain are among the most common complications of breast cancer patients. Chronic pain is a devastating symptom or syndrome with a psychosomatic response, which is sometimes difficult to manage adequately in clinical practice. Many studies have focused on the use of medications to reduce patients’ pain, with a limited number of studies on the impact of non-pharmacological approaches, even though medications do not always alleviate pain or bring sufficient relief [22]. The use of non-pharmacological interventions can help patients to reduce the damage to the body, but also improve patient´s well-being.
Effective pain management depends on regular screening for early recognition of pain, accurate characterization of pain such as onset, duration, intensity, location, and severity to correctly determine the type of pharmacological or non-pharmacological treatment required. The main advantage of non-pharmacological interventions is their safety with minimal incidence of adverse effects, affordability, and the usability of the intervention when needed, even alone in the home environment, which increases the sense of control over pain. The disadvantage of non-pharmacological interventions is the low awareness among health professionals and patients, as well as the lack of knowledge of research regarding non-pharmacological interventions in pain management in women with breast cancer. The neglect of non-pharmacological interventions in pain management has further been influenced by the low confidence of physicians and other non-medical professions in these interventions, even though there is substantial evidence of their effect on pain management in women with breast cancer. The late onset of the effect of particular interventions or lack of familiarity with these interventions may lead patients to distrust these methods. Therefore, non-pharmacological interventions that have a beneficial effect in the management of pain in women with breast cancer should be noted [23,24].
Conventional research presents contraindications of non-pharmacological procedures in connection with their application in patients with cancer. The opinions of experts should be considered when deciding on their use in the context of complex treatment of the disease. More recent publications have provided the theoretical background to the immunomodulatory effect of acupuncture [25,26]. The most common contraindications of acupuncture include bleeding or hematoma, pain, vegetative symptoms; furthermore, physicians do not recommend intervention in the case of skin malignancy, as there could be a risk of neoplastic cell proliferation; and severe neutropenia secondary to the risk of infection [27,28]. Of course, theoretical approaches need to be considered, as the aim of the studies presented was to reduce pain and influence the onset of relapse and deterioration of health status. Unquestionably, these methods have relevance in the palliative setting, with only a small group of studies addressing this issue and presenting their results.
Acupuncture
Acupuncture is now a compulsory part of the curriculum in all medical schools in China. Acupuncture is generally considered safe when performed by a licensed, trained practitioner. The procedure uses disposable, pre-sterilized needles to apply heat, pressure or electrical stimulation to specific areas or points on the body. Acupuncture can be used as a stand-alone therapy or as part of comprehensive pain care, as well as to treat other physical, mental, and emotional conditions [29]. The positive effect of acupuncture on reducing IA-related joint pain in postmenopausal women with breast cancer was confirmed in a study by Hershman et al. [20], where, after eight weeks, there was a statistically significant reduction in joint pain in the acupuncture group compared with the simulated acupuncture and control groups. The reduction of joint pain in postmenopausal women with IA-associated breast cancer has also been confirmed in a study by Mao et al. [21], which compared the effect of electroacupuncture in comparison with simulated acupuncture and a control group. At week eight and continuing at week twelve, the electroacupuncture group showed a statistically significant decrease in pain scores assessed and pain interference than in the control group.
The study by Lu et al. [11] investigated and confirmed the benefits of acupuncture in female breast cancer survivors with CIPN symptoms. CIPN is a relatively common side effect of anticancer treatment that significantly interferes with the patient’s daily, social activities. As a result of damage to sensory, autonomic, motor and nerve fibers, the fingers and toes feel tingling or numb. From the fingers, however, the symptoms spread to the entire limbs, and patients describe the pain as burning, stabbing, sharp, electrifying in nature, or as a dull, pressing, unbearable pain. In addition to numbness, ataxia of the lower limbs may occur, associated with impaired stability and risk of falling, which reduces the patient’s quality of life, daily living activities, and disrupts sleep [30]. In that study [11], after 8 weeks, acupuncture resulted in a significant reduction in sensory symptoms of CIPN, improved quality of life, reduced pain severity, pain interference, and average pain compared with the control group. The effect of acupuncture on pain, nausea, anxiety, and coping in women undergoing mastectomy was assessed in a study by Quinlan Woodward et al. [31]. A total of 30 women were divided into an acupuncture group (n=15) and a control group (n=15). Baseline scores of pain, anxiety, nausea, and coping ability were recorded by the patients before undergoing the intervention. Women enrolled in the acupuncture intervention group had acupuncture applied twice during the postoperative hospitalization, at least 12 hours apart, on the day of surgery or the day after surgery. Women assigned to the standard care control group were observed twice after surgery and at least twelve hours apart to assess the same variables. After the first intervention, women in the acupuncture group demonstrated statistically significant improvements in pain, nausea, anxiety, and coping skills. After the second intervention, they continued to report significant improvements in pain and anxiety compared with pre-intervention baseline scores. In contrast, women in the control group showed no statistically significant differences between pre- and post-standard care measures for pain, nausea, anxiety, and coping ability at either the first or second visit [31].
Transcutaneous electrical acupoint stimulation applied 30 minutes prior to induction of anesthesia was also of positive benefit. A study revealed that transcutaneous electrical acupoint stimulation in combined acupoints prior to anesthesia in patients undergoing mastectomy is associated with a reduced incidence of chronic pain in the breast scar, axilla, shoulder, and flank for 6 months postoperatively, compared with simulated acupuncture as a control group [32].
Yoga
Abroad, the interventions of complementary and alternative medicine, under which Yoga also falls, are recognized and studied at universities as accredited disciplines. Yoga connects the mind and body with breath, movement, and meditation. Cancer patients practicing Yoga gradually find that their quality of life and complications arising from their emotional and physical condition are greatly improved. Yoga has been studied in the interest of helping cancer patients to relieve pain and other related problems [33]. A study by Carson et al. [17] showed no differences in the effects of treatment on daily pain in women with metastatic breast cancer between the group receiving the Mindful Yoga intervention and the group receiving the supportive intervention. However, in the group of women practicing Yoga, they found a relationship between the length of Yoga practice and daily pain. By spending relatively more time practicing Yoga on two consecutive days, they were more likely to experience less pain the following day. Tsai et al. [19] confirmed that Mindful Yoga is more effective than massage intervention in reducing knee joint pain associated with IA use in women who have survived breast cancer. However, after the eight-week Yoga intervention, the positive results were maintained for at least one week, highlighting the importance of ongoing Yoga intervention. YOCAS© Yoga contributed to improved musculoskeletal symptoms in women who had survived breast cancer taking IA or TAM compared to the control group. Participants in the study demonstrated significant relief of general pain, muscle pain, body aches, and other musculoskeletal symptoms (feeling sick, needing help with activities of daily living, and feeling heavy in the head and body) after the Yoga intervention compared with the control group [18].
This trend of using Yoga has been supported by international professional societies that have included Yoga as an integrative therapy in their guidelines. The Society for Integrative Oncology (SIO) and the American Society of Clinical Oncology (ASCO) clinical guidelines for the use of integrative therapies during and after breast cancer treatment recommend Yoga because of the proven evidence for reducing anxiety as well as improving quality of life, mood, depressive symptoms, fatigue, and sleep [34]. The National Comprehensive Cancer Network (NCCN®) also accepts Yoga and recommends that patients incorporate Yoga into their lives to improve certain areas of survival such as fear, cognitive function, menopausal symptoms, and pain. Yoga is formally included in the NCCN Clinical Practice Guidelines in Oncology as an effective intervention for managing cancer-related fatigue and anticipatory nausea/vomiting [35,36].
Cognitive-behavioral therapy
Other available studies have demonstrated a beneficial effect on pain reduction using cognitive-behavioral therapy. In a study, Johannsen et al. [37] assessed the effectiveness of cognitive therapy on late post-treatment pain (after surgery, chemotherapy, or radiotherapy) in women treated for breast cancer. A total of 129 women were randomly assigned to either a group that underwent an eight-week intervention once a week or a control group. Pain intensity was assessed at baseline, after the intervention, and at three and six months. The intervention included slightly shorter two-hour sessions, shorter meditation exercises, gentler Yoga exercises, psychoeducation with a main focus on participants’ painful experiences at the time of presenting, and cognitive exercises that focused on pain. Daily 45-minute home exercise was also encouraged. An experienced mindfulness therapy instructor facilitated all sessions. A statistically significant effect on pain experience was observed in favor of cognitive therapy, and the effect appeared to be relatively stable over time. A similar result was achieved in the study by Mozafari-Motlagh et al. [38]. Twenty-four breast cancer patients were randomized into two groups: twelve patients with intervention and twelve patients without intervention. Meetings were held weekly (90 minutes) for eight weeks. The intervention consisted of breathing exercises, awareness of visceral sensations, exercises focusing on the perception of one’s own body, behavioral therapy techniques (such as problem solving), assertiveness, acceptance, and coping with distress in daily life. The results showed that pain was significantly reduced in the intervention group compared with the non-intervention group, at different times of measurement.
Massage therapy
Massage therapy appears to be a promising additional non-pharmacological intervention that has shown significant pain reduction in many studies. Massingill et al. [39] in their study found a beneficial effect of myofascial massage (n=10) applied to the breast, chest, and shoulder area in resolving pain and upper extremity mobility limitations in women who underwent breast cancer surgery compared with a control group who underwent relaxation massage (n=10). The groups underwent two 30-minute massages per week for eight weeks (sixteen massages total). After eight weeks, pain and mobility scores were reassessed compared with baseline scores. There was a significant reduction in pain scores among participants in the myofascial massage group, but no significant change among participants in the control group. However, a change in pain scores was observed between the two groups.
Reflexology is a type of massage in which pressure is applied to specific points on the feet or hands that are thought to coincide with certain parts of the body and create systemic balance. Sikorskii et al. [40] examined the effect of a home-based reflexology intervention (n=102) delivered by either a friend or family caregiver compared with a no-intervention control group (n=107) on multiple symptoms in women with breast cancer undergoing chemotherapy or hormone therapy. The friend or family caregiver was trained during two home visits by a reflexologist and was asked to provide at least one 30-minute reflexology intervention per week for four weeks. The reflexology intervention proved to be more successful in assessing pain, but not in assessing other observed symptoms such as fatigue, disturbed sleep, shortness of breath, lack of appetite, numbness, tingling, and depression compared with the control group.
Therapeutic touch and massage are used to manage cancer-related pain and are approved as supportive care methods specifically for breast cancer patients by the professional cancer society ASCO. The goal of healing touch is to use light, gentle touch with the hands to restore and balance energy that has been disrupted due to stress, illness, injury, grief, various medical procedures, and cancer treatments such as chemotherapy, surgery, radiation, and hormone therapy. Several studies suggest that healing touch reduces cancer-related pain, including for breast cancer patients. A study by Gentile et al. [41] compared the effect of therapeutic touch and massage on pain reduction before and after an intervention. A total of 407 breast cancer patients at different clinical stages were divided into a group undergoing therapeutic touch (n=233) and a group undergoing massage (n=174) for approximately 45 minutes. The therapeutic touch intervention was tailored to the individual patient’s needs. Patients received healing touch individually, remained clothed, and lay in the supine position in a separate room with soft lighting and soothing music. The massage intervention was also provided in a dedicated room with soft lighting, soothing music, and a heater to induce patient comfort. The massage therapists used the following techniques: gliding, rhythmic strokes, and gentle brief holding of the skin and subcutaneous tissue. After one application of the therapeutic intervention, patients in both groups reported a statistically significant reduction in pain scores: 69% of patients in the massage group and 65.7% of patients in the healing touch group. Thus, both therapeutic touch and massage were associated with clinically significant improvements in pain.
Although all of the above studies have shown positive results, their limitations should also be highlighted. The most common limitation was the small sample size, which limited the ability to assess the effect in the intervention groups. Another limitation was the short-term follow-up of the effect; more frequent and longer-term measurements may help to identify the true treatment effect and assess the sustainability of the benefits of the interventions. In some studies, the blinding criterion could not be met, which may have affected outcome monitoring to some extent. A further problem was the premature termination of the study by a few respondents, which could lead to biased estimates. The results may also be influenced by the patients’ pharmacological regimen and its changes during pain management with non-pharmacological interventions. Both the Society for Integrative Oncology (SIO) and the American Society of Clinical Oncology (ASCO) regularly participate in the development and publication of clinical practice guidelines and have developed guidelines focused on the use of integrative therapies for the treatment of cancer pain to provide evidence-based recommendations to patients and physicians. These have included acupuncture for aromatase inhibitor-related joint pain as one of the recommended interventions with proven results in reducing pain. Acupuncture, reflexology and acupressure may be recommended for general cancer or musculoskeletal pain. Hypnosis may be recommended for patients experiencing procedural pain, and massage may be used for patients with pain during palliative or hospice care. The quality of evidence for other mind-body interventions or natural products for pain is either low or inconclusive [42].
The present review study seeks to highlight the possibilities of using non-pharmacological approaches in women with breast cancer, to highlight the positive impact on both somatic and psychological areas. We have to state that the field of alternative pain relief is not yet sufficiently explored and is challenging for the possibility of conducting further studies, with variables such as quality of life, treatment modalities, stages of the disease and other additional factors. Selected studies demonstrate significant results that present the positive impact of non-pharmacological approaches on improving pain perception at different stages of the disease. The heterogeneity of pain causes (tumor and treatment-induced pain) in the presented studies confirmed the impact of non-pharmacological treatments on different types of pain and its alleviation.
The review study had several limitations, including a small sample size, which limited the ability to assess the effect in the intervention and non-intervention groups. Another common limitation was the short-term follow-up of the effect. More frequent and longer-term measurements may help to identify the accurate effect of the intervention and thus assess the sustainability of the benefits of the interventions. In some studies, the blinding criterion was impossible to fulfil, which may have affected the monitoring of the results to some extent. A further problem was the premature termination of the study by a few respondents, which could lead to biased estimates. Some studies excluded patients older than 65 years, patients who were unable to perform basic activities of daily living, or bedridden patients, which narrowed the scope of these results. The results may also be influenced by the patient´s pharmacological regimen and its changes during the course of pain management with non-pharmacological interventions.
Conclusions
Fear and uncertainty of future, fear of death, loss of a sense of femininity, frustration, and other emotional disturbances significantly reduce the quality of life in women with breast cancer. Psychosocial burdens persist even in patients who have undergone breast surgery with minimal damage to the body. The most severe consequence of the disease is pain, which becomes the subject of multidisciplinary care. Knowledge of non-pharmacological interventions may prompt their inclusion in the comprehensive care of the breast cancer patient. As a result of this work, the following recommendations have been made:
– to increase awareness of non-pharmacological interventions among healthcare professionals as effective methods for pain reduction in cancer patients;
– to weigh the benefit over the risks and contraindications of non-pharmacological approaches in the light of the current treatment and the influence of various other factors;
– to conduct open communication between healthcare professionals and patients about their concerns, values, and preferences, enabling shared decision-making about the most appropriate pain management approach;
– to involve the interdisciplinary team in the therapy, training medical staff
– physiotherapists, psychologists, and nurses in certain techniques of non-pharmacological interventions;
– to promote research on non-pharmacological interventions in clinical practice to elucidate the therapeutic value, benefits, and risks for reducing pain, whether perioperative pain or chronic pain syndromes;
– to implement studies with non-pharmacological procedures also in the field of palliative care of cancer patients and to identify their benefits and the possibility of reducing the burden of treatment;
– to support research into non-pharmacological interventions and their impact on overall quality of life in different clinical stages of cancer.