Introduction
One of the most common postoperative complications associated with lung resection is air leakage, which, according to some studies, occurs in more than 50% of thoracic operations. Most leaks heal in the first 24 to 48 h, but between approximately 5% and 10% persist. Prolonged air leakage, defined as leakage persisting for more than 5 days, increases hospital stays and healthcare costs, and is associated with higher incidence of empyema and other complications [1, 2].
Air leakage increases the length of time patients stay in the hospital, increases hospital costs, and is associated with a higher prevalence of empyema and other complications [3, 4]. Since air leakage is more common in partial and sub-lobar resections compared to lobectomy, strategic placement of the pleura and careful suctioning can be effective in preventing this complication [3]. In recent years, the use of supporting materials and sealants has garnered attention in lung resection procedures [5]. These sealants are categorized into synthetic and fibrin types [5, 6]. Tissue biological adhesives are often made from a combination of fibrinogen and thrombin, of which fibrinogen is of human origin, and thrombin is of bovine origin. This substance is wholly absorbed during tissue repair and does not cause a foreign body reaction or fibrosis [7]. In addition, the risk of transmitting viral infections such as hepatitis B and C and allergic reactions using autologous fibrin adhesives is minimized. There have been several studies on using fibrin adhesives in thoracic surgery, the authors of which have recommended using fibrin adhesives to reduce air leakage. Still, thoracic surgeons have not reached a consensus on its routine use [7]. Given the limited number of studies on fibrin adhesives, more research is required for an accurate evaluation of their efficacy.
Aim
The present study investigated the effect of autologous fibrin adhesive in improving air leakage in thoracic surgery and can help increase the available information in this field.
Material and methods
Study design and setting
This was a randomized, parallel-group, single-blind study, conducted at the Thoracic Surgery Department of our hospital from 2020 to 2021.
Participants
Patients eligible for this study were those referred for thoracotomy and pulmonary resections or lung decortication. The inclusion criteria encompassed candidates deemed suitable for these procedures based on preoperative evaluations, which included respiratory function testing and cardiac counseling. The study excluded patients presenting with severe comorbidities. These included conditions such as renal failure, heart failure, uncontrolled diabetes, uncontrolled hypertension, severe ischemic heart disease, and severe chronic obstructive pulmonary disease. This approach ensured the selection of participants whose medical profiles were aligned with the study’s objectives while maintaining safety and ethical considerations.
Interventions
Patients in the study were randomized to two distinct groups: the intervention group and the control group. Those in the intervention group received autologous fibrin adhesive, which was specially prepared from 50 ml of the patient’s blood collected 2 days prior to the operation. This adhesive was strategically applied to the lung parenchyma and suture lines at the conclusion of the surgical procedure. In contrast, patients in the control group underwent standard surgical procedures as typically practiced, without the incorporation of the fibrin adhesive. This distinction between the groups was central to assessing the efficacy of the fibrin adhesive in the context of thoracic surgery.
Randomization and blinding
Randomization was performed using a random permuted block design, with block sizes of 4 or 6. Allocation concealment was ensured using sealed envelopes. The study was single-blinded, with the data analyst unaware of group assignments.
Outcomes
The primary outcomes included the duration of air leakage, chest tube drainage volume, and length of hospital stay. Secondary outcomes were postoperative complications, assessed during hospitalization and at 1-week and 1-month follow-ups.
Procedure
In this study, patients who met the inclusion criteria entered the study after obtaining informed consent. All patients who were candidates for lung resection or decortication and preoperative assessments considered suitable for surgery were randomly assigned to intervention and control groups using the envelope method. In the intervention group, 50 ml of the patient’s blood was taken 2 days before the operation to prepare the autologous fibrin adhesive. After lung surgery, at the end of the operation, the prepared adhesive was sprayed on the damaged surface of the lung parenchyma and suture lines using a syringe. Other surgeries and postoperative care stages were routine and similar to the control group. Patients in the control and intervention groups in the postoperative period were evaluated in terms of air leakage, the volume of chest tube drainage, chest tube exit time, length of hospitalization, complications after surgery during hospitalization, and 1-week and 1-month visits after discharge, and the findings were recorded in prepared checklists.
Autologous fibrin adhesive preparation method
Blood samples were taken from the patients to prepare platelet-rich plasma (PRP) and tissue adhesives. PRP and fibrin glue were prepared in completely standard and sterile conditions in a clean room.
48 h before surgery, 50 ml of blood was taken from the patient’s peripheral veins and sent to a clean room at room temperature. PRP was prepared by the first centrifugation at 2,000 g for 2 min and the second at 4,000 g for 8 min. The supernatant plasma was separated, and 3 ml of PRP was initially separated. Fibrinogen was prepared from the supernatant plasma. Plasma was frozen at –80°C, then thawed at 4°C, centrifuged at 2300 g for 3 ml fibrinogen preparation, and mixed with the PRP; the final volume of PRP and fibrin glue was about 6 ml. During surgery, fibrin glue was prepared sterile by adding 1 ml of 1% calcium gluconate to 6 cc of platelet-rich fibrinogen.
Due to the hospitalization of the patient and the daily visit by the surgeon, possible postoperative complications, such as empyema and failure to open the lungs, were diagnosed by plain radiography or, if necessary, a chest computed tomography (CT) scan. Based on the diagnosis, appropriate treatment was performed with drainage or suctioning of the pleural air.
Ethical considerations
The study was approved by the Ethics Committee of Mashhad University of Medical Sciences (reference number IR.MUMS.REC.1397.324).
Statistical analysis
Data were analyzed using SPSS software version 20. The continuous variables were checked using the Kolmogorov-Smirnov test to determine the normal distribution of mentioned data. The variables with or without normal distribution were reported as the mean ± standard deviation (SD), or median (percentile 25–75), respectively. The qualitative variables were described using frequency (%) and compared by χ2 or Fisher’s exact test. The unpaired sample T-test or Mann-Whitney test was used to compare quantitative variables between groups. The p-value < 0.05 was considered significant.
Results
Patient enrollment and characteristics
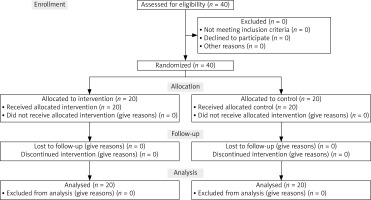
A total of 40 patients were enrolled in this study, randomized equally into the intervention and control groups. The baseline demographics and clinical characteristics of the patients are summarized in Table I. This table provides a comparative overview of gender, diagnosis, and type of surgery across both groups (Figure 1).
Table I
Comparison of gender, patient diagnosis, type of operation, and complications in patients in the intervention and control groups
Primary and secondary outcomes
The primary outcomes evaluated were the duration of air leakage, volume of chest tube drainage, and length of hospital stay. The secondary outcomes included the frequency and types of postoperative complications.
Outcome measures
In the study, significant differences were observed across primary outcome measures between the intervention and control groups. The intervention group demonstrated a marked reduction in chest tube drainage, with a mean volume of 457.50 ±211.68 ml, notably less than the control group’s mean of 627.50 ±137.15 ml (p = 0.005). Similarly, the duration of air leakage was significantly shorter in the intervention group, averaging 0.30 ±0.73 days compared to the control group’s 6.10 ±8.51 days (p = 0.007). Additionally, the length of hospital stay was reduced in the intervention group, with a mean duration of 5.40 ±1.63 days, in contrast to the control group’s mean of 9.75 ±8.36 days (p = 0.033). However, the analysis of postoperative complications revealed no significant difference between the groups, indicating that the use of autologous fibrin adhesive effectively improved specific postoperative outcomes without increasing complication risks (Table II).
Table II
Comparison of chest tube drainage volume, duration of air leakage, and length of hospital stay after surgery in control and intervention groups
Discussion
This study focused on evaluating the effectiveness of autologous fibrin glue in reducing post-thoracic surgery air leakage. While our findings indicated no significant difference in complication rates between the intervention and control groups, the use of autologous fibrin glue was associated with a notable decrease in chest tube drainage volume, air leakage duration, and hospital stay length. However, it is important to consider the variance in surgical procedures between groups, as this may have impacted the outcomes.
Comparative studies in this domain yield interesting parallels and contrasts. Kılıç et al. [8] reported similar hospitalization durations in their study, but with higher complication rates in both autologous and homologous fibrin glue groups. The disparity in complication rates compared to our study could be attributed to the smaller sample sizes, suggesting a need for larger-scale studies for more definitive conclusions.
Similarly, Cardillo et al. [7] found no significant difference in postoperative complications between their fibrin glue and control groups. However, the types of complications differed, indicating potential variability based on the nature of the adhesive (autologous vs. non-autologous).
Lopez et al. [9] demonstrated shorter air leakage times in the fibrin glue group, aligning with our findings. However, their study did not show significant differences in drainage removal times, highlighting the variability in postoperative outcomes.
Gonfiotti et al. [10] observed reduced air leakage duration in patients using fibrin glue, similar to our results. Interestingly, unlike our study, they did not find a significant difference in hospital stay duration, suggesting that factors other than fibrin glue application may influence this outcome.
Finally, Moser et al. [5] emphasized the efficacy of autologous fibrin glue in reducing long-term air leakage and chest tube drainage duration, corroborating our findings. The larger sample size in our study lends additional credence to these results.
Conclusions
The current literature, along with our findings, underscores the potential of autologous fibrin glue in improving postoperative outcomes in thoracic surgery. However, variations in study designs, sample sizes, and types of fibrin glue used suggest that further research is needed. We recommend that thoracic surgeons consider autologous fibrin glue as a viable option, given its demonstrated benefits and the supportive evidence from various studies.