Introduction
Hypertension is a leading cause of cardiovascular disease and a significant indicator of chronic kidney disease [1]. The global prevalence of high blood pressure continues to rise [2, 3]. Studies in China show that 23.2% of adults have hypertension (HTN), yet only 15.3% have achieved effective blood pressure control [4]. Patient-Centre Evaluative Assessment of Cardiac Events (PEACE) funded by the Chinese government revealed that 45% of individuals aged from 35 to 75 live with HTN, and most patients urgently require medical treatment and correct education on HTN from doctors [5]. Even among those with stage 2 HTN, only one-third of patients receive regular treatment [6]. Compared to developing countries, developed nations exhibit higher HTN awareness and treatment rates, driven by substantial healthcare investment and widespread disease education in communities [7]. Although the Chinese government has regarded the management of HTN patients in communities as a National Basic Public Health Project (NBPHP), the high population risk of HTN still persists, directly reducing the life quality and increasing the burden on patients [6].
Effective self-management improves the quality of life for HTN patients. Effective management includes clinical treatment, lifestyle modification, and self-management, all of which help reduce cardiovascular disease risk [8]. Studies show that patients with mild to moderate HTN at diagnosis are often highly motivated to adopt lifestyle changes [9]. Apparently, unhealthy lifestyles, including eating habits with excessive sugar and salt, high-pressure life events, and mental diseases, are factors that potentially increase the morbidity rate of HTN in China [10]. Therefore, improving patient self-management requires appropriate medical intervention and health education provided by Community Medical Services (CMS).
Self-management is crucial for promoting patient health, with the World Health Organization (WHO) recommending measures such as disease prevention, self-medication, health education, and seeking specialist care when needed [11]. Enhancing hygiene knowledge and health awareness is particularly effective for self-management of HTN, especially in rural western China [12]. Meanwhile, chronic HTN self-management is shifting from large general hospitals to CMS, allowing patients to receive personalized treatment plans and lifestyle education [13].
Studies based on Western populations have shown that diverse self-management interventions, targeting body index changes and longevity, effectively control blood pressure (BP) [14]. Currently, no systematic reviews have specifically addressed Chinese patients with HTN.
Therefore, this study aims to investigate whether self-management practices can improve HTN and reduce the risk of cardiovascular disease. The study has two primary objectives: (1) To assess whether self-management improves BP, systolic blood pressure (SBP), and diastolic blood pressure (DBP) in patients. (2) To evaluate whether CMS is more effective than general hospitals in developing personalized plans for BP control.
Methods
Study design
This systematic review was performed according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [15].
Data sources and search strategy
An electronic database search was conducted for studies available up to December 31, 2019. The meta-analysis included data from four international databases: PubMed, Cochrane Library, Web of Science, and EBSCO, as well as four Chinese databases: China National Knowledge Infrastructure (CNKI), Chinese Biomedical Database (CBM), Chinese VIP Information (VIP), and WanFang Database. The search strategy incorporated both Medical Subject Headings (MeSH) and free-text terms. The used search terms were adjusted to each database, and were as follows: (“Hypertension” OR “Blood Pressure, High” OR “Blood Pressures, High” OR “High Blood Pressure” OR “High Blood Pressures”) and (“Self-management” OR “Self-Management” OR “Management, Self”) and (“China” OR “People’s Republic of China”), without any extra limitation. To focus on self-management effectiveness in China, the “Affiliation” filter was applied in PubMed and Web of Science. In addition, all of the searching results were manually checked to identify the potential literature.
Study selection
The selection criteria for these studies were as follows: 1) designed as randomized controlled trial; 2) included individuals aged above 18 with diagnosed or self-measured primary HTN; 3) adopted any self-management measures in the intervention group, including but not limited to health education for patients offered by healthcare providers, and the control group was limited to general caring or normal health education. 4) The major results were BP, SBP, and DBP; the secondary outcomes were the changes of HTN, as the result of HTN-relevant education, and behavior change. 5) The published literature has complete data. Exclusion criteria: 1) Non-randomized controlled trial articles; 2) interventions applied in the research did not satisfy preselection criteria; 3) observational research, reviews, case reports, repeated publications; 4) studies included serious complications with hypertension, such as heart disease, stroke, and kidney failure; 5) studies using mobile applications to intervene in BP control of patients.
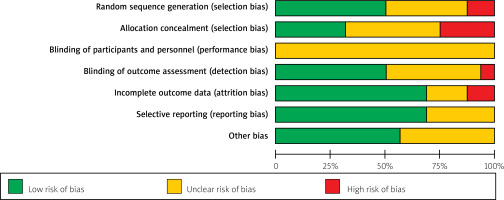
Assessment of risk of bias and quality
To minimize error, bias and quality were assessed independently by two reviewers. The risk of bias and quality among the included examples was independently assessed by two researchers. A consensus meeting was held before analyzing the data, which was to rethink the comparison of details from the available studies selected for this review, and reached an agreement on the conflicting points.
Risk of bias was evaluated using the Cochrane Collaboration’s Risk of Bias Handbook for randomized controlled trials (RCTs) [16]. Bias was rated as “low,” “high,” or “unclear” based on criteria such as random sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting, and other biases. If there was any disagreement from both researchers, a third author (ZSS) would resolve the discrepancies with negotiation.
Data extraction and analysis
Three researchers in parallel extracted independently and double-checked the data, then researchers manually removed the repeated documents. According to the title and the abstract, researchers identified the relative literature. Based on the inclusion/exclusion criteria, two researchers independently screened the literature, and cross-checked each other. The discrepancies were resolved by all the researchers. The researchers extracted the useful data from studies that had been selected, including the study characteristics (title, authors, year of publication, and study location); information of participants (age, gender, baseline BP, BP value after the intervention, demographic information, and sample size); intervention information (time, methods, and contact frequency); and other relevant outcomes.
Review Manager of the Cochrane Collaboration (RevMan 5.3, Cochrane Organization) was used to perform the meta-analysis. All 11 studies without discrepancy of baseline BP (p > 0.05) reported no difference in SBP and DBP between the intervention and control group (p > 0.05). In addition, SBP and DBP are continuous variables, for which the mean difference (MD) was calculated with the 95% confidence interval (CI). Both the Cochrane Q test and I2 statistic were used to assess heterogeneity across study outcomes [17]. In the next step to assess the relationship between intervention characteristics and blood pressure, we pre-defined subgroups in advance: 1) age (divided into groups based on the average age of patients, and one of the groups aged above 60 years old); 2) intervention time (greater than or equal to 1 year or less than 1 year); 3) baseline BP (based on baseline BP value, groups were divided into SBP > 140 mm Hg, or DBP < 90 mm Hg). Owing to the large heterogeneity of the study, a random effect model was used in the analysis.
Results
Search results
A total of 5634 studies were initially identified from the 7 databases. Subsequently, 2,569 duplicate articles were removed. After screening the titles and abstracts of the remaining 3,065 articles, 2,784 irrelevant studies were excluded. Based on inclusion and exclusion criteria, 265 studies were excluded after full-text review of the remaining 281 articles. Finally, all 16 studies were included in the next narrative synthesis, and provide major results, including mean SBP, DBP, and other measures of interventions with self-management. Comparatively, the control groups were managed with the Chinese Three-degree Hypertension Management Model (CTHMM). The flowchart showing the study selection process is presented in Figure 1.
Study characteristics
The characteristics of the 16 studies are presented in Table I [18–33]. Among them, 4 studies were from Shanghai [18, 20, 23, 26], and the others were from Shenzhen [19], Wuhan [21], Zhengzhou [22], Foshan [24], Jiaxing [25], Yangzhou [27], Liuzhou [28], Beijing [29], Sanhe [30], Huai’an [31], Hongkong [32], and Hangzhou in China [33].
Table I
The characteristics of the 16 studies
| Author, year | Location, city | Sample size (Int/Con) | Median age | Duration | Intervention theory | Self-management measures | Intervention frequency | Indicator | |
|---|---|---|---|---|---|---|---|---|---|
| Int | Con | ||||||||
| Chen et al. 2011 [18] | Community, Shanghai | 198/196 | 60 | 12 months | CGSMH/SET | Group lectures; Follow-up visit | Routine care | Once a month | BP; HSMK; BW |
| Feng et al. 2015 [19] | Community, Shenzhen | 374/392 | 59 | 3 months | CGSMH | Teaching knowledge of self-management; Behavior guidance | Routine care | Once a week | BP; HSMK; BC |
| Fu et al. 2004 [20] | Community, Shanghai | 111/108 | 67.2 | 6 months | CGSMH | Group lectures; Follow-up visit | Routine care | Once a week | BP; BW |
| Gong et al. 2018 [21] | Community, Wuhan | 167/149 | 64.2 | 30 months | Transtheoretical model | Group lectures; Exercise plan; Follow-up visit | Routine care | Once a week | BP; BC |
| Li et al. 2013 [22] | Hospital, Zhengzhou | 97/95 | 54.2 | 12 months | SET | Conventional medicine; Group lectures; Follow-up visit | Routine care; Follow-up visit | Once a week | BP |
| Lu et al. 2012 [23] | Community, Shanghai | 30/30 | 64 | 12 months | SET | Group lectures; Self-management pamphlet; Behavior intervention | Routine care | Once every 2 weeks | BP; HSMK; BC |
| Luo et al. 2016 [24] | Hospital, Foshan | 100/100 | 38 | 12 months | SMCDG | Group lectures; Talking; Behavior intervention | Routine care; Health education | Once every 2 weeks | BP; BC |
| Luo et al. 2019 [25] | Rural area, Jiaxing | 625/667 | 62.6 | 12 months | CGSMH | Group lectures; Self-management pamphlet; Behavior intervention | Routine care | Once a month | BP; BC |
| Ren et al. 2016 [26] | Community, Shanghai | 977/572 | 64.8 | 6 months | CGSMH | Behavior intervention; Follow-up visit | Routine care | Once every 2 months | BP; BC; BMI |
| Shen et al. 2017 [27] | Rural area, Yangzhou | 266/288 | 66.7 | 12 months | Unclear | Group lectures | Routine care | Once a week, for 2 months; then once a month | BP; BC |
| Wang et al. 2015 [28] | Community, Liuzhou | 40/40 | 67.5 | 12 months | KAP | Group lectures; Belief cultivation; Behavior guidance | Routine care; Health education | Once a month | BP; BC |
| Ding et al. 2014 [29] | Community, Beijing | 1410/655 | 61.6 | 1.5 months | SMCDG | Self-management and heathy education lectures | Routine care; | Once every 2 weeks | BP; HSKM; BC |
| Yu et al. 2003 [30] | Community, San He | 118/110 | 63.3 | 4 months | CGSMH | Group lectures | Routine care | Once a week | BP; BC; BMI |
| Zhang et al. 2014 [31] | Hospital, Huai’an | 198/198 | 58 | 12 months | CGSMH | Group lectures; Behavior intervention | Routine care; Conventional medicine | Once a week | BP; HSKM; BC |
| Chiu et al. 2010 [32] | Hospital, Hong Kong | 31/32 | 53.9 | 2 months | Unclear | Consulting support; Group lectures; Follow-up visit | Routine care | Once a month | BP; SMA |
| Zhu et al. 2017 [33] | Community, Hangzhou | 36/37 | 69 | 1 months | CGSMH | Nurse intervention; Follow-up visit | Routine care; | Once every 2 weeks | BP; SMA |
[i] CGSMH – Chinese Guidelines for Self-Management of Hypertension, SET – Self-Efficacy Theory, KAP – Knowledge; Attitude/Belief, Practice, SMCDG – Self-management of Chronic Disease Guidelines, BP – blood pressure, HSMK – Hypertension and Self-Management Knowledge, BW – body weight, BC – behavior changes, BMI – body mass index, SMA – self-management adherence.
Two studies were conducted in rural areas, 14 in urban areas [18–24, 26, 28–33]. Four studies were professionally conducted in general hospitals with suggestions by experienced doctors and nurses [22, 24, 31, 32], and 12 studies were managed according to the CMS developed by the Chinese government with essential measures of chronic diseases [18–20, 22–26, 29–31, 33]. The age of patients ranged from 38 to 69, and the duration of the trials ranged from 1.5 to 18 months in the 16 articles. A total of 8652 individuals were included in this review, in which 4874 individuals were in the intervention group, and 3788 individuals in the control group. The minimum sample size for a single study was 60 in and the maximum was 2075. The mean baseline BP was reported in 8 of the studies according to the WHO diagnosis criterion of hypertension [20–23, 28, 31–33], and another 8 studies reported SBP < 140 and DBP < 90 [18, 19, 24–27, 29, 30].
All 14 studies indicated that the intervention design was based on existing theories or models [18–26, 28–31, 33]. Chinese Prevention and Treatment of Hypertension Guidelines (CPTHG) were most frequently mentioned for hypertension treatment in 9 studies [18–20, 24–26, 30, 31, 33]. There were 3 among 14 studies that adopted the Self-efficacy theory. Knowledge Attitude/Belief Practice (KAP) [18, 23, 24], Chronic Disease Self-Management Educational Project (CDSMEP), and Transtheoretical Model (TTM) were respectively applied in 3 studies [21, 28, 29]. Two studies did not mention any information about the theory of intervention in those studies [27, 32]. In the control group, all 16 studies adopted routine nursing care, with three studies incorporating health education [24, 28, 31]. Personalized intervention plans were made in 7 studies [19, 21, 23–25, 28, 31], aimed at improving the behavior of patients for a healthy lifestyle.
Out of all the studies, 12 used the BP data as their primary outcome [18–21, 23, 25–27, 29, 30, 32, 33], and 4 studies adopted behavior changes of individuals as the final purpose to prevent hypertension [22, 24, 28, 31]. Meanwhile, behavior changes were regarded as the secondary outcome in the other 10 studies [19, 21, 23, 25–27, 29, 30, 32, 33]. Behavior changes were measured through improvements in self-management scores, lifestyle habits, and medication adherence.
Intervention characteristics
To synthesize the effects of self-management interventions on hypertension, we summarized seven key aspects of the interventions mentioned in the studies: the educational courses of healthy lifestyle and hypertension, behavior guidance, personal intervention scheme, education manual, self-management manual, interview, and feedback from personnel. Each intervention study included at least two components, with health education serving as the foundation for self-management.
Five studies found that self-management measures in intervention groups improved medication adherence [27, 30–33]. Nine studies showed that behavior changes, including a low-salt diet and exercise combined with goal setting, were more effective in the intervention group than the control group, though unhealthy habits such as smoking and drinking persisted [18, 23, 25, 27, 29–33]. Six studies reported that hypertension awareness in the intervention group was significantly higher than in the control group (p < 0.05) [18, 19, 23, 27, 28, 31]. Seven studies developed detailed personalized plans for patients, including education on healthy diets, hypertension knowledge, exercise regimens, sugar and protein intake, and the supervision of BMI and blood biochemical markers [19, 21, 23-25, 28, 31]. In these studies, four reported that self-management intervention is capable of improving the diet habits of high salt [19, 21, 25, 31], protein, and monosodium glutamate. Five studies indicated that after regular learning sessions and group discussions, patients were more attentive to related diseases and hypertension knowledge [19, 21, 23, 24, 31]. Three studies showed that patients who use self-management interventions tend to be motivated to exercise [21, 24, 28]. Changes in mental stress were observed in two studies [19, 25].
Regarding timing and frequency, most studies varied considerably, and the effective implementation of the intervention was not always clear. The frequency of most of the interventions was decided based on the total intervention duration. For interventions lasting 3 months or less, delivery occurred weekly in two studies and biweekly in another [29, 32]. Ranging from 3 months to a year, four of the studies adopted a learning course once a week, and regular physical examination [19, 20, 26, 30].
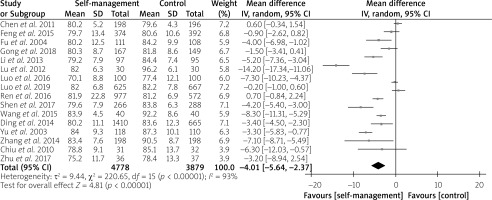
Meta-analysis of blood pressure
SBP and DBP data were mentioned in all the literature, two of which reported that there was not any significant difference after self-management intervention (p > 0.05) [19, 26]. Six studies assessed hypertension control knowledge acquisition through questionnaires and quizzes [18, 19, 23, 27, 28, 31]. After 6 months of intervention, only one study found that blood pressure was significantly reduced, but the differences were not obvious in the final result [27]. As shown in Figure 2, the estimated MD of SBP between intervention and control groups was significant as –6.37 mm Hg (p < 0.001; 95% CI: –9.13 to –3.61), with high heterogeneity (X215 = 350.81, I2 = 96%, p < 0.001). Following Figure 3, there was a statistically significant difference in MD of DBP as –4.01 mm Hg (p < 0.001; 95% CI: –5.64 to –2.37), with high heterogeneity (X215 = 220.65, I2 = 93%, p < 0.001). It was demonstrated that self-management interventions are an effective approach to improving hypertension.
Figure 2
Forest plot of the difference of systolic blood pressure between intervention and control group
CI – confidence interval.
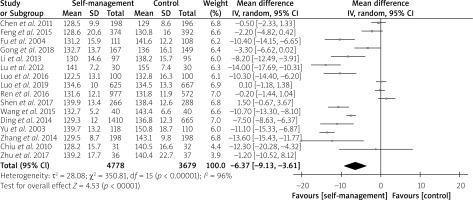
Figure 3
Forest plot of the difference of diastolic blood pressure between intervention and control group
CI – confidence interval.
According to different intervention characteristics, subgroup analyses were used to estimate heterogeneity and effect-size difference in hypertension. Subgroup analyses showed that SBP (p = 0.42 > 0.05) and DBP (p = 0.28 > 0.05) were not well controlled in rural areas. The results of analysis of the remaining subgroups were consistent with those shown without grouping, and the intervention group showed effective control of BP (p < 0.05). In groups below the BP baseline, the intervention effectiveness in the subgroup of SBP > 140 mm Hg (MD = –9.72; 95% CI: –12.70 to –6.74) was better than that in the subgroup of SBP < 140 mm Hg (MD = –3.48; 95% CI: –6.44 to –0.51) (p < 0.01). Also, the intervention effectiveness in the subgroup of DBP > 90 mm Hg (MD = –6.26; 95% CI: –8.96 to –3.57) was better than that in the subgroup of DBP < 90 mm Hg (MD = –2.05; 95% CI: –3.67 to –0.43) (p = 0.01 < 0.05). With grouping based on the location of intervention, self-management intervention showed a greater advantage of SBP control (p < 0.01) in hospital (MD = –11.38; 95% CI: –14.24 to –8.52) than that in communities (MD = –6.17; 95% CI: –9.27 to –3.06) or rural areas (MD = 0.51; 95% CI: –0.74 to 1.77). Meanwhile, the same result was found for DBP control (p = 0.01 < 0.05): those in hospital (MD = –6.56; 95% CI: –7.71 to –5.40) showed a greater advantage compared to those in the community (MD = –3.54; 95% CI: –5.73 to –1.34) or rural areas (MD = –2.17; 95% CI: –6.09 to 1.75). Analyzing the subgroups of intervention time or the subjects’ age, the effects of SBP and DBP control did not show any significant difference (p > 0.05). All the results are shown in Table II.
Table II
Results from the subgroup analyses of mean differences in systolic blood pressure and diastolic blood pressure
Risk of bias
The risk of bias was assessed, and was found to be high risk. There was not any study that was absolutely free of bias. Among 16 studies, 8 studies that reported the procedure of sequence generation were rated as low risk [19–21, 24, 27, 28, 31, 32]; however, 2 studies were judged as high risk, due to cluster sampling that did not generate a random sequence [18, 25], and the remaining studies were judged to be unclear as the sequence generation was not elucidated [22, 23, 26, 29, 30, 33]. Five studies that specifically reported allocation concealment were rated as low risk [24, 27, 28, 31, 32]; four studies were assessed as high risk due to allocation based on the personal characteristics of trial participants [18, 20, 26, 29]; the remaining seven articles were rated as unclear due to insufficient detail [19, 21–23, 25, 30, 33]. Due to the nature of self-management interventions, it was impossible to blind participants or researchers; therefore, all studies were rated as unclear risk for performance bias. The risk of detection bias was low in eight studies [18–21, 25, 28, 30, 33], which presented reliable results; but only one was unmasked to outcome assessors [24]; seven articles were rated as unclear [22, 23, 26, 27, 29, 31, 32], as it was not sufficiently clear whether the researchers were blinded. Five of the studies reported that some of the individuals withdrew from the tests [18, 22, 26, 27, 30], two of which were assessed as high risk due to the missing values being over 10% [18, 26]; twelve other studies were rated as low risk due to complete data [20–25, 27–29, 31–33]. Eleven studies were rated as low risk for selective outcome data because they reported the primary and secondary outcomes that were pre-defined in their plans [18–20, 24–31]. Five studies displayed incomplete outcome data, which were assessed as unclear [21–23, 32, 33]. Nine studies with other biases were defined as low risk [19, 21–23, 25, 26, 28, 30, 32]. It was unclear whether in the remaining studies there existed other bias [18, 20, 24, 27, 29, 31, 33]. The total bias in all the literature is presented visually in Figure 4.
Publication bias and sensitivity analysis
Graphical representation of publication bias was depicted through a funnel plot separately for SBP (Figure 5) and DBP (Figure 6), which was slightly asymmetric and with outliers. Sensitivity analyses were conducted using the “leave-one-out” method to assess the reliability of the estimates obtained from the meta-analysis. It was found that none of the studies had a significant adverse effect on the overall results.
Discussion
The purpose of this meta-analysis was to evaluate the effectiveness of self-management interventions implemented by Chinese healthcare workers in improving SBP and DBP among patients with hypertension. This systematic review incorporated data from 16 RCTs, involving a total of 8,457 participants. The findings indicate that self-management interventions are effective in improving the hypertension status of participants within the intervention groups. Specifically, compared to the conventional care group, the average reductions in SBP and DBP were 6.37 mm Hg and 4.01 mm Hg, respectively. Subgroup analyses further demonstrated significant differences in both SBP and DBP based on intervention location, duration, and lifestyle modifications. This suggests that effective blood pressure control is influenced not only by the types of self-management methods employed but also by the participants’ willingness to engage actively in these practices. These results underscore the role of self-management interventions in alleviating high blood pressure symptoms, even amidst considerable heterogeneity among the studies. In this systematic review, the sources of heterogeneity probably derived from the following reasons: 1) The diversity of interventions. The different self-management theories were conducted with different findings. 2) The heterogeneous qualities of the included studies. There are three studies with a sample size of less than 100. 3) Publication bias may exist. Most studies reported positive results, but two studies were the opposite.
Comparative analysis of intervention sites reveals that self-management interventions are most effective when conducted in hospital settings, followed by community interventions. Notably, self-management interventions in rural areas showed no significant differences in SBP and DBP between the intervention and control groups. However, this finding is based on only two studies conducted in rural settings, indicating a need for further research to validate these results. As we know, self-management intervention is conducted mainly to stimulate the enthusiasm of the patients, cultivate the sense of hypertension prevention, and thus let them participate in their own health management. Due to the low educational level, incomplete medical system, and low quality of life, for patients in Chinese rural areas, especially the elderly, it is difficult to achieve the right concept of self-management of HTN. Because of the professional treatment and health care, the self-management intervention in the hospital is more effective than in the community, but most patients are those with a serious situation of hypertension [34]. In contrast, the self-management interventions implemented in the community are mainly for those who have mild hypertension symptoms, and the effect is not as great as that observed in the patients in the hospital [35]. This conclusion can be proved in the subgroup analyses of the baseline BP. Subgroups with baseline SBP ≥ 140 and DBP > 90 showed significantly better results than those with SBP < 140 and DBP < 90. In the subgroup analyses based on the age of the patient and the duration of intervention, there were no significant differences after self-management intervention between groups.
Although this meta-analysis did not specifically examine the relationship between self-management behaviors and hypertension awareness, six studies reported an increase in hypertension recognition among participants in the intervention group. Additionally, nine studies demonstrated positive behavioral changes among individuals with hypertension, including adherence to low-salt diets and increased physical activity. However, certain addictive behaviors, such as smoking and drinking, are notably resistant to modification through self-management interventions. This resistance can be attributed to the fact that these behaviors are not only personal choices but are also significantly influenced by social factors.
Hypertension has been a major public health problem worldwide. According to the statistics, one-fifth of the Chinese adult population has HTN, and another two-fifths is in the pre-HTN state, diagnosed by Chinese hypertension guidelines, and the median age of patients is continually rising [36]. In addition, hypertension is increasingly being diagnosed in young adults across China [37]. According to the clinical evidence, hypertension has become a serious trigger for many chronic diseases, such as cardiovascular diseases, diabetes, and obesity, which significantly impair the quality of life [38]. Thus, implementing the self-management measures and increasing the detection of HTN are beneficial to improve quality of life and reduce medical expenditure. On the side of government, it is time to put more money into hypertension prevention and build a robust basic healthcare system in undeveloped areas.
This is the first systematic review and meta-analysis conducted in China that focuses on the relationship between self-management interventions, blood pressure improvement, blood pressure control, and behavioral outcomes. A major strength of our research is its comprehensive analysis, which evaluates various relevant factors related to self-management interventions and includes only randomized controlled trials (RCTs) to provide accurate evidence. However, one limitation of our study is the significant heterogeneity among the included studies. To address this, we performed subgroup analyses and used a random-effects model for assessment. Additionally, most of the literature comes from high-income regions, which may limit the applicability of our findings to other areas.
In conclusion, this systematic review clearly demonstrated that self-management interventions can reduce both SBP and DBP in patients with hypertension, with hospital-based interventions being the most effective. Additionally, these interventions can improve lifestyle behaviors [39]. However, hypertension patients living in rural areas still require more self-management support and proper education to manage the progression of hypertension. The impact of the duration of self-management interventions on hypertension status remains unclear.