Introduction
In 1910, Hans Christian Jacobaeus performed the first thoracoscopic operation. With the advent of single lung ventilation in 1960, minimally invasive thoracic surgery gained popularity. Today, many thoracic surgery procedures are carried out using video-assisted thoracoscopic surgery (VATS) [1, 2].
Although VATS procedures are less painful than standard thoracotomies, postoperative pain remains a significant cause of morbidity in patients undergoing thoracic surgery [3]. Additionally, preoperative anxiety levels are significantly elevated in surgical patients [4]. Preoperative anxiety makes it harder to heal and causes more problems after surgery, but it also makes the pain after surgery worse [5].
Effective patient education has a positive effect on postoperative outcomes. According to numerous studies, preoperative patient education reduces preoperative and postoperative anxiety in surgical patients, increases patient compliance, and decreases postoperative pain levels [6–9]. Although preoperative patient information is provided in several ways, multimedia-supported information is considered to be the most effective approach [10–14].
There are studies demonstrating the good impact of preoperative multimedia-supported information on postoperative pain and anxiety, as well as postoperative complications, in a variety of surgical patient groups [10–14]. To our knowledge, there are no studies examining the effects of multimedia-supported information on pain and anxiety in VATS patients.
Aim
The goal of this study was to find out how educating patients using multimedia affects their pain and anxiety before and after VATS surgery.
Material and methods
After getting permission from the local ethical council (3.11.2017–2017/11) and our hospital administration, the study included 50 patients who had VATS between December 2017 and December 2018.
Patients younger than 18 or older than 85, patients with trauma or who needed surgery right away, patients with poor general health, patients who were unconscious or intubated, patients who could not read or write, patients who had trouble communicating, patients with active mental illnesses such as anxiety disorder or depression, and patients who had already had a VATS or thoracotomy were not included in the study.
Informed consent was obtained from all patients. Before surgery, the subjects were put into two groups – the multimedia information group (MIG) and the control group – using a closed-envelope method.
For both groups, demographic information and vital signs were written down, and all patients were given spirometry tests before and after surgery in the spirometry laboratory.
Preoperative STAI-T and STAI-S tests were administered. In the preoperative phase, the MIG watched a 6-minute video, and then the STAI-S exam was administered again. An additional STAI-S test was administered to both groups 1 day following surgery. Thoracic anatomy, VATS procedure, complications, and post-operative follow-up are explained in the multimedia training video used in the study.
During the procedure, all patients were administered general anesthesia, intubated with a double-lumen (Robertshaw) endotracheal tube, and ventilated with a single lung. In circumstances where single-lung ventilation was not possible due to malpositioning of the tube, the surgery was performed using an apneic approach. The same surgical team was responsible for all procedures. At least one chest tube was inserted following surgery.
As part of routine postoperative care, all patients received 2 g of paracetamol each day (2 × 1 g iv). Additional analgesics (tramadol and pethidine) were given according to the VAS score and whether the patient had pain or not. The patients’ daily VAS scores were found by taking the average of the three highest VAS values for each day.
Statistical analysis
With a two-tailed α value (error rate) of 0.05 (sensitivity = 0.95) and a β value of 0.20 (study power = 0.80), we calculated (G*Power 3-power analysis program) that each group required at least 21 participants.
The demographic and operational data are presented as a number (N) and a percentage (%). Continuous variables are represented by their median, minimum (Min), maximum (Max), and interquartile range (IQR).
The Shapiro-Wilk test was used to assess whether continuous variables were suitable for normal distribution, while non-parametric tests were employed when the data were not suitable for normal distribution. The χ2 test was used to assess categorical data, the Mann-Whitney U test was used to compare groups, and the Wilcoxon and Friedman tests were used to examine variations within the group. In this study, a p-value of less than 0.05 was considered statistically significant (95% CI).
The statistical analysis was performed using IBM SPSS v25.0 (IBM, New York, USA).
Results
The study involved fifty patients in all. These patients were divided into two groups: the multimedia information group (MIG; n = 25) and the control group (n = 25).
The median age of patients in the multimedia information group was 56 (range: 19 to 72, IQR = 34), whereas the median age of patients in the control group was 35 (range: 18 to 80 years, IQR = 39). There was no statistically significant difference (p = 0.260). Table I lists the demographic characteristics and surgical information of the patients included in the study.
Table I
Demographic characteristics and surgical information
Comparing the preoperative and postoperative pulmonary function tests (PFT) of both groups, there was no significant difference in FEV1 (p = 0.914 and p = 0.174 for MIG and control groups, respectively) or FEV1/FVC (p = 0.175 and p = 0.927 for MIG and control groups, respectively). Table II provides information about PFT values.
Table II
PFT valuesa
All patients underwent STAI-T testing, and preoperative and postoperative STAI-S testing. The difference in the preoperative and postoperative STAI-S scores between the two groups was statistically significant (p = 0.001 and p = 0.0001, respectively). The postoperative STAI-S scores of MIG increased, but this increase was not statistically significant (p = 0.656). In the control group, postoperative STAI-S scores were reduced significantly (p = 0.010).
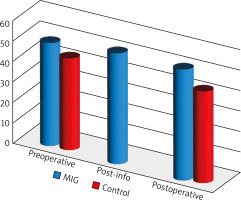
MIG also underwent a post-training STAI-S examination. There was no significant difference between post-training STAI-S scores and pre- and post-operative STAI-S scores (p = 0.146 and p = 0.688, respectively). Table III provides information on STAI testing. The mean STAI-S scores are illustrated in Figure 1.
Table III
STAI test results
| Variable | MIG (median – IQR) | Control (median – IQR) | P-value |
|---|---|---|---|
| STAI-T test | 50 – 5 | 42 – 15 | 0.002 |
| Preoperative STAI-S | 49 – 6 | 41 – 10 | 0.001 |
| Post-info STAI-S | 50 – 7 | NA | |
| Postoperative STAI-S | 49 – 5 | 38 – 10 | < 0.0001 |
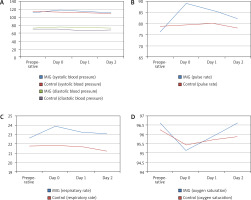
In all groups, there was no significant difference in the changes in systolic blood pressure, diastolic blood pressure, respiratory rate, or oxygen saturation between the preoperative and postoperative first 3 days. Pulse variations in the control group were not significant (p = 0.502). Table IV provides information on the alteration of vital signs. Changes in vital signs are illustrated in Figure 2.
Table IV
Change of vital signs
In the first 3 days after surgery, there were no significant differences between the groups in terms of pain scores (VAS score), tramadol, or pethidine use. In the control group, VAS ratings and pethidine doses were dramatically reduced, except for the dose of tramadol. Table V provides postoperative VAS scores and analgesic dosages. Figure 3 illustrates variations in postoperative VAS ratings and analgesic dosages.
Table V
Postoperative VAS scores and analgesic doses
| Variable | Day 0 | Day 1 | Day 2 | P-value3 |
|---|---|---|---|---|
| VAS Score: | ||||
| MIG1 | 3.6 – 1 | 3 – 1.50 | 1 – 2 | < 0.0001 |
| Control1 | 3.5 – 2.48 | 2 – 2.25 | 1 – 2 | < 0.0001 |
| P-value2 | 0.207 | 0.059 | 0.874 | |
| Tramadol doses [mg]: | ||||
| MIG1 | 300 – 100 | 300 – 50 | 300 – 0 | 0.004 |
| Control1 | 300 – 0 | 300 – 0 | 300 – 0 | 0.115 |
| P-value2 | 0.051 | 0.696 | 0.727 | |
| Pethidine doses [mg]: | ||||
| MIG1 | 50 – 100 | 0 – 50 | 0 – 0 | < 0.0001 |
| Control1 | 50 – 100 | 0 – 50 | 0 – 0 | < 0.0001 |
| P-value2 | 1.000 | 0.913 | 0.156 |
Discussion
There were no statistically significant differences between the two groups in terms of demographic information, surgical characteristics, or vital signs. In our study, when we investigated the changes in blood pressure, pulse, respiration rate, and oxygen saturation over the first 3 days of patients’ hospitalization, we observed that only patients with MIG had a substantial decrease in the daily pulse change. Lee et al. [15] found that educating patients before surgery did not change their blood pressure, breathing rate, or pulse. Pulmonary function tests showed no statistically significant differences between the two groups, and we could not find a study that compared pulmonary function tests.
There was a statistically significant difference in the STAI-T, preoperative, and postoperative STAI-S scores between groups. In a meta-analysis study on patients undergoing orthopedic surgery, Johansson et al. [16] found that preoperative information reduced patient anxiety levels. In another study evaluating patients undergoing cataract surgery, with preoperative information participants were shown to be less anxious and more satisfied with their treatment [4, 17]. Similar outcomes were observed in investigations involving heart surgery patients [18–20]. Tarhan et al. [21] in a study on patients who underwent transrectal prostate biopsy and Lin et al. [7] in a study on patients who underwent surgery under general anesthesia found that video-assisted information reduced anxiety levels prior to surgery. However, there is contradictory research indicating that video information does not reduce the anxiety levels of surgical patients. According to a study by Salzwedel et al. [14], video information had no effect on the anxiety levels of patients undergoing major surgery.
In our study, we discovered that multimedia materials did not reduce anxiety. On the contrary, although it was not significant, there was a slight increase in postoperative anxiety in the MIG group. Moreover, the decrease in the control group was significant. This could be due to the lack of standardized video content.
Postoperative pain is one of the key concerns for surgical patients [22–25]. Numerous studies have shown that patient education decreases postoperative pain and painkiller intake [15, 25]. In our study, both groups had similar postoperative VAS scores and analgesic use. In the first 3 days, the dose of tramadol administered to MIG decreased significantly. However, the postoperative tramadol doses in the control group were similar. Many other factors may affect this result.
Although the study’s power analysis indicated that 21 patients were sufficient, we believe that the study’s most significant weakness is its small sample size. At the time of randomization, patients with MIG exhibited higher baseline anxiety levels than those in the control group. In this instance, it is possible that the information provided influenced the change in anxiety levels. Our results show that receiving multimedia information before surgery has some effect on pain but none on anxiety.
Conclusions
Providing multimedia information does not reduce postoperative anxiety. It can even be said that it slightly increases the level of anxiety, although it is not significant. Although significant results were obtained only for the dose of tramadol in patients who received multimedia information, it can be said that it had no effect on VAS scores or analgesic consumption. However, in order to generalize these results, prospective randomized trials with larger populations are required.