Introduction
Patients with acute respiratory distress syndrome benefit from mechanical ventilation in the prone position (PP), which was first advised five decades ago [1] and may be easily adopted in any critical care unit (ARDS) [1]. Research published in the last several years has shown that PP may decrease mortality in certain patients with severe ARDS if treatment is started early and used for a long time [2]. Many critically ill patients, however, have a low tolerance for early enteral nutrition due to decreased stomach motility with delayed gastric emptying, which can increase their risk for problems such vomiting, aspiration, and ventilator-associated pneumonia [3]. Recent studies’ findings to the contrary, guidelines propose monitoring gastric residual volumes (GRVs) on an intermittent basis and withholding enteral feeding when GRVs reach predetermined thresholds in order to minimize this danger [4].
Critically ill and ventilated patients frequently have a negative nitrogen balance and a hypermetabolic condition. Nutritional support, regulation of the immune response, lessening of disease severity, and improvement in prognosis are only a few of the ways in which enteral nutrition contributes to the care of critically ill patients [5]. The two most prevalent types of enteral nutrition are gastric-tube feeding and post-pyloric feeding. The most effective and safest method of administering enteral nourishment is still up for debate. Some research [6, 7] showed no significant difference in pneumonia comparing the two feeding strategies, while studies by Acosta-Escribano [8] found a decreased incidence of pneumonia with post-pyloric feeding. Similar inconsistencies were found in research examining the impact of the gastrointestinal diet. According to Hsu et al. [9] and Acosta Escribano et al. [8], post-pyloric feeding is preferable to gastric-tube feeding in terms of the proportion of the patient’s total nutrition that is absorbed. A previous study [10] found no statistically significant difference between the two feeding routes in terms of the proportion of total nutrition delivered to the patient.
The clinical prognosis of intensive care unit patients is strongly correlated with their dietary status. Some studies found that post-pyloric feeding reduced the need for mechanical ventilation compared to gastric-tube feeding [8, 11], whereas others found the opposite [6, 10, 12]. Hence, the aim of the study is to assess the safety and tolerability of different enteral feeding techniques in critically ill patients regarding mortality, pneumonia, aspiration, and vomiting.
Material and methods
The epidemiological declaration served as the basis for the development of a methodology that was subsequently meta-analyzed.
Criteria for study selection
Using statistical methods such as frequency rate, odds ratio (OR), relative risk, or mean difference (MD) at a 95% confidence interval, the current meta-analysis aimed to compare the safety and tolerability of different enteral feeding techniques in critically ill patients in terms of mortality, pneumonia, aspiration, and vomiting (CI).
Eligibility criteria of the study
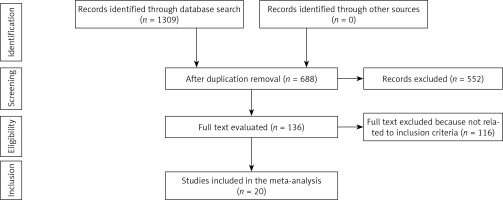
Studies of any size were eligible for inclusion in the current meta-analysis; however, letters and review articles were excluded since they did not meet the inclusion criteria due to their lack of causality. Figure 1 shows a conceptualization of the meta-analysis, comparing the sensitivity of various enteral feeding methods in critically sick patients with respect to mortality, pneumonia, aspiration, and vomiting.
Criteria for inclusion of articles that were used in the current meta-analysis
Studies that could be included were those that fulfilled the following criteria: First, studies with different designs, such as randomized controlled trials, cross-sectional, cohort, prospective studies, and retrospective studies, were all included in this investigation. The second criterion for inclusion of studies was that the research participants should be hospitalized, critically ill, and receive enteral nourishment. Finally, regarding methods for gauging the safety and acceptability of gastric and post-pyloric feeding interventions, studies focusing on the impact of different ventilation positions on clinical outcomes for subjects receiving enteral feeding were included.
Study exclusion criteria
The excluded studies were those that did not meet the following criteria: studies that did analyze feeding practices, but either did not compare prone to supine position, or did not assess their impact on clinical outcomes of hospitalized individuals; studies with inaccurate or misleading outcome measurements that are needed for data analysis and presentation; in addition, studies that did not directly compare stomach and post-pyloric feeding findings or did not focus on ventilation position.
Identification
Gastric feeding, Post-pyloric feeding, Ventilation, Vomiting, Mortality, and similar terms were used to conduct a comprehensive literature search in Medline/PubMed, the Cochrane Library, OVID, Embase, and Google Scholar up until the end of February 2022 (Table I). P (population): hospitalized people in critical condition; I (intervention/exposure): stomach feeding versus post-pyloric; Comparison of gastric and post-pyloric feeding (letter C). Aspiration, vomiting, pneumonia, and reflux of stomach content all fall under the umbrella term “outcome” (O). Study types (S) include both randomized clinical trials and retrospective studies. EndNote software was used to classify the research publications in order to eliminate duplicates. To further assess the impact of risk variables on the safety and tolerability of various enteral feeding procedures in critically ill patients with regards to mortality, pneumonia, aspiration, and vomiting, we also reviewed all title and abstract data. All relevant data for this topic were collected from the subjects we considered.
Table I
Strategy of searching scientific databases
Screening
All of the information relevant to the subjects and the research was recorded into a standardized database. Traditional forms also included information about the study’s setting, primary outcome evaluation, treatment mode, duration, categories, statistical analysis, information source, and qualitative and quantitative evaluation, as well as the first author’s surname and the total number of subjects.
The Risk of Bias Tool from the Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1, was used to assess the methodology’s robustness.
Different levels related to bias risk might be found in the criteria for assessment
The examination of the criteria revealed three distinct types of prejudice. To put it another way, the risk of bias was rated from low (when all quality parameters were met) to moderate (when some quality parameters were met but not all) to high (when none of the quality criteria were met or included). Examination of the paper revealed similar anomalies.
Statistical analysis
The odds ratio (OR) and 95% confidence interval (CI) were determined dichotomously in the statistical analysis utilizing the fixed effect model. To begin with, the I2 index was measured from 0% to 100%, whereas the heterogeneity scale went from 0% to 25%, 50%, and 75%, representing no, low, moderate, and high levels of heterogeneity. If the value of I2 was greater than 50%, then the random effect was prioritized over the fixed influence. A p-value of less than 0.05 was needed to draw any conclusions; thus we used subgroup analysis on the first data set. Reviewer Manager, Version 5.4.1 was used for statistical analysis with two-tailed p-values (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
Results
Among the 1309 unique reports, the current meta-analysis included 25 studies [6–30] published between 1992 and 2019 that matched the inclusion criteria. The current study included 1984 participants at the start of the study (Tables II and III). The mean outcome that had been evaluated among studies comparing prone versus supine position was the gastric residual volume (GVR). When comparing the mean GRV in the prone and supine positions for administering enteral feeding, there was no significant difference in three included studies [27, 29, 30]. One study found that after 5 days of observation, the mean GRV in the prone position was considerably larger than in the supine position (10 (0–58.6) vs. 27.6 (3.8–119.4) ml) [28]. In contrast, another trial including newborns found that the prone position considerably reduced GRV compared to the supine position (43.95% vs. 23.26%, for a 50 ml/kg/day infusion volume, and 48.07% vs. 28.46% for a 100 ml/kg/day infusion volume) [26]. Regarding the safety and tolerability of different enteral feeding techniques in critically ill patients regarding mortality, pneumonia, aspiration, and vomiting were assessed during the current analysis including a total of 13 clinical trials that compared the incidence of pneumonia for included subjects for both groups (gastric and post-pyloric feeding), while 7 studies assessed the impact of both techniques on pulmonary aspiration occurrence among subjects. Three studies compared the impact of both interventions on the reflux gastric content, while 12 and 13 studies compared the effect of both interventions on rates of vomiting and mortality respectively. As shown in Figures 2–6, in comparison with the post-pyloric nutrition group, gastric feeding had no significant impact on the mortality rate (OR = 1; 95% CI: 0.76–1.32). While the findings showed a significantly higher incidence of pneumonia with gastric feeding compared with post-pyloric (OR = 1.92; 95% CI: 1.43–2.57), there was no significant difference regarding pulmonary aspiration and vomiting (OR = 1.41; 95% CI: 0.75–2.65 and OR = 0.92; 95% CI: 0.66–1.27 respectively). Reflux gastric content was significantly higher with gastric nutrition (OR = 8.23; 95% CI: 2.43–27.89). A subgroup analysis was performed to minimize heterogeneity among the included studies. Subgroup analysis was performed to demonstrate the impact of COPD status and the statistical power of the included studies.
Table II
Outcomes of studies that compared the impact of enteral feeding in different ventilation positions on clinical status
| Study | Country/year | Study type | Population sample | Characteristics |
|---|---|---|---|---|
| Van der Voort [30] | Holland, 2002 | Prospective observational study. Single-center | n = 19 Adult subjects on mechanical ventilation in the prone position | The control group subjects lay supine with their heads elevated (30°) for 6 h. Nutritional goal of 80 ml/h of enteral feeding. After 6 h in the supine posture, the patient should be turned onto their side if they have hypoxemia (PaO2/FiO2 100) or pneumonia with significant bronchial secretion. Bed should have a 30° head elevation. 80 ml/h of enteral nutrition as the dietary goal |
| Reignier [28] | France, 2004 | Prospective cohort. Single-center | n = 71 (37 control/34 intervention). Adult clinical subjects on invasive mechanical ventilation | Semi-recumbent supine position for control. 18 h of enteral nutrition using an infusion pump. In cases of severe hypoxemia (PaO2/FiO2 150; FiO2 = 0.6; PEEP = 10 cm H2O), the prone posture is the recommended course of action. 18 h of enteral feeding with an infusion pump (6-hour rest in the supine or prone position, with position determined randomly) |
| Chen [26] | Taiwan, 2013 | Crossover randomized trial. Single-center | n = 35 Convenience sample of preterm infants | The positions in one group were supine-prone, while in the other group they were prone-supine. The sequence then was reversed. BM was given by OGT via infusion pump to both groups. The volume increased every 3 h to the nutritional target of 160 ml/kg/day from the baseline volume of 20 ml/kg/day. Administration of BM was done in two stages: 50 ml/kg/day and 100 ml/kg/day |
| Saez de la Fuente [29] | Spain, 2014 | Prospective observational study – single center | n = 34 Adult patients on mechanical ventilation | Intervention group: prone posture, if severe hypoxemia (PaO2/FiO2 < 150) in the presence of hemodynamic stability for 48 consecutive hours; neck/head were alternated to the right and left every 2 h. Enteral nutrition through infusion pump for 24 h. Control group: supine position, with discontinuation of enteral feeding if GRV > 500 ml in 6 h. Enteral nutrition through infusion pump for 24 h |
| Lucchini [27] | Italy, 2017 | Retrospective observational study. Single-center | n = 25 patients on mechanical ventilation | Supine position with the head of the bed raised at an angle of at least 15° (control position). Positioning aid: a 15-degree elevation of the head of the bed when lying flat on one’s back (pronation criteria were not described). If the GRV rises beyond 300 ml, the patient in both groups will have their enteral feedings stopped, metoclopramide given, and their fluid intake restored |
Table III
Characteristics of studies included in the meta-analysis
| Study | Year | Country | Total | Gastric | Post-pyloric |
|---|---|---|---|---|---|
| Acosta-Escribano [9] | 2010 | Spain | 104 | 54 | 50 |
| Davies [14] | 2002 | Australia | 66 | 35 | 31 |
| Davies [10] | 2012 | Australia | 180 | 89 | 91 |
| Friedman [6] | 2015 | Brazil | 115 | 61 | 54 |
| Hsu [9] | 2009 | China | 121 | 62 | 59 |
| Kortbeek [18] | 1999 | Canada | 80 | 43 | 37 |
| Kearns [17] | 2000 | USA | 44 | 23 | 21 |
| Montecalvo [20] | 1992 | USA | 38 | 19 | 19 |
| Montejo [21] | 2002 | Spain | 101 | 51 | 50 |
| Taylor [7] | 2016 | France | 50 | 25 | 25 |
| Wan [11] | 2015 | China | 70 | 35 | 35 |
| Wang [24] | 2015 | China | 34 | 19 | 15 |
| Zhu [25] | 2018 | China | 141 | 71 | 70 |
| Esparza [16] | 2001 | Mexico | 54 | 27 | 27 |
| Neumann [22] | 2002 | USA | 60 | 30 | 30 |
| Singh [23] | 2012 | India | 78 | 39 | 39 |
| Day [15] | 2001 | USA | 180 | 89 | 91 |
| Boivin [13] | 2001 | Mexico | 80 | 40 | 40 |
| White [12] | 2009 | Australia | 104 | 54 | 50 |
| Liu [19] | 2019 | China | 100 | 50 | 50 |
| Total | 1800 | 916 | 884 | ||
Figure 2
Forest plot illustrating the impact of gastric tube and post-pyloric feeding on incidence of pneumonia
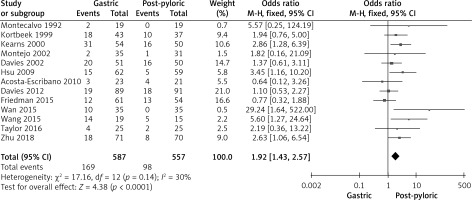
Figure 3
Forest plot illustrating the impact of gastric tube and post-pyloric feeding on incidence of pulmonary aspiration
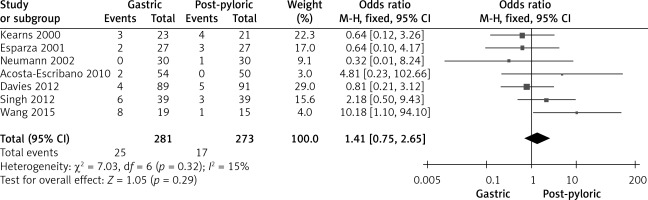
Figure 4
Forest plot illustrating the impact of gastric tube and post-pyloric feeding on the incidence of reflux gastric content
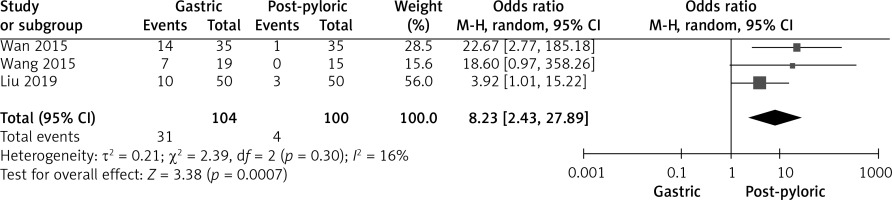
Figure 5
Forest plot illustrating the impact of gastric tube and post-pyloric feeding on incidence of vomiting
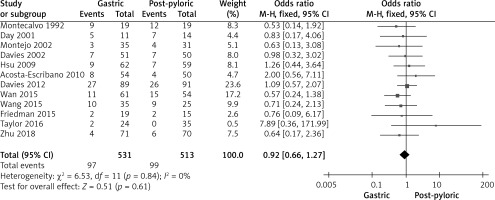
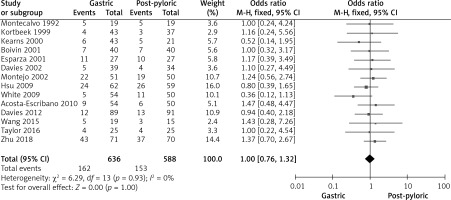
Figure 6
Forest plot illustrating the impact of gastric tube and post-pyloric feeding on mortality rate
We found that no single study had sufficient data in all seven categories. All along the quality spectrum, the included studies’ procedures varied greatly. The quality of the studies used in this meta-analysis ranged widely. The randomized dressings-led trial was determined to have insufficient methodological tools.
Discussion
The current study involved 25 studies [6–30], involving 1984 participants at the start of the study. The aim was to measure and assess the impact of prone compared to supine position besides the safety and tolerability of different enteral feeding techniques in critically ill patients regarding mortality, pneumonia, aspiration, and vomiting. Critically ill patients with severe hypoxemia in the prone position can benefit from enteral feeding, according to research by Saez de la Fuente et al. [29]. Also, Chen et al.’s finding showed that the GRV of preterm newborns was lower in the prone position compared to the supine position when given 50 ml/kg/day and 100 ml/kg/day, respectively [26]. In contrast, Reignier et al. observed that patients receiving invasive mechanical ventilation were more likely to vomit after receiving enteral nutrition while in the prone position [28]. However, there was no significant difference in GRV between the prone and supine positions after 3 and 6 h of enteral feeding according to the findings of Van der Voort et al. [30].
Regarding the type of enteral feeding and in comparison with the post-pyloric nutrition group, gastric feeding had no significant impact on the mortality rate. While the findings showed a significantly higher incidence of pneumonia with gastric feeding compared with post-pyloric nutrition, there was no significant difference regarding pulmonary aspiration and vomiting. Reflux gastric content was significantly higher with gastric nutrition. However, because some of the included studies had a small sample size (only 11 studies had a sample size less than 100 subjects), careful analysis of the results is required, implying the necessity for further trials to confirm the current findings or possibly to have a substantial effect on the assessment of the intervention impact. The heterogeneity was low for all subgroup analyses, indicating the strong power of the final conclusion.
Mortality data from the 14 trials included in the meta-analysis showed that out of a total of 588 patients, 153 died in the post-pyloric feeding group and 162 died in the gastric feeding group from 636 subjects. It was determined that there was no heterogeneity between the investigations. It was found that there was no statistically significant difference in mortality rates between the two feeding methods. The fixed-effects model was employed because of the modest degree of heterogeneity present.
Twelve studies involving 1044 individuals reported the frequency of vomiting. With such a low level of heterogeneity, a fixed-effects model was employed. When comparing the gastric feeding group to the post-pyloric feeding group, we discovered that patients in the latter group experienced less vomiting. The gastric group experienced 97/531 vomiting events compared with 99/513 from the post-pyloric group.
For a total of 204 subjects, the incidence rate of acid reflux in the stomach was reported in three trials. Overall, heterogeneity was found to be quite low among these studies (I2 = 16%), justifying the use of the fixed effects model for combining data. In this analysis, the incidence of reflux of gastric contents was found to be significantly lower in the post-pyloric feeding group (4/100) compared to the gastric-tube feeding group (31/104).
Based on data from 13 trials including 1144 participants, a difference in pneumonia incidence was found between the two feeding methods. It was documented that 98 subjects in the post-pyloric group had pneumonia, while 168 subjects in the gastric tube group had pneumonia. Due to the lack of heterogeneity, we used a fixed-effects model.
Seven studies involving 554 participants reported on the topic of pulmonary aspiration. Data analysis using the fixed-effects model was conducted because of the low heterogeneity among these trials. The current meta-analysis found a lower rate of aspiration with post-pyloric feeding (6.23%) compared to gastric-tube feeding (8.9%).
Limitations: Many publications were left out of the current meta-analysis because they did not meet the inclusion criteria, which introduced a substantial amount of bias into the study. There was also considerable uncertainty regarding how to incorporate factors like gender and race into the analysis. Analyses based on data from previous studies may be flawed due to information gaps. Twenty studies were included in the meta-analysis, eleven of which were very small (under 100 participants). Lost data and unpublished studies may contribute to the problem of influence bias. Studies differed in the average weight of their subjects.
Conclusions
This meta-analysis compared the rates of mortality, pneumonia, aspiration, and vomiting associated with various enteral feeding methods in very ill patients. Feeding using a gastric tube did not significantly reduce mortality. Impacts of prone position compared with supine during enteral feeding varied from fewer gastric events to a significantly higher vomiting rate. Also, it was found that gastric feeding was associated with a considerably increased incidence of pneumonia compared to post-pyloric feeding, but that neither pulmonary aspiration nor vomiting had any bearing on the results. With gastric feeding, reflux of the stomach’s contents was significantly higher. The results of our meta-analysis study also did not show any correlation with demographic variables such as study participants’ race or gender. Additional research is needed to validate these findings or significantly increase confidence in the effect evaluation because of the small sample sizes in several of the studies included in the meta-analysis.