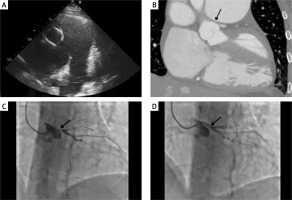
A 45-year-old female with pulmonary arterial hypertension (PAH) secondary to a congenital atrial septum defect was admitted to the cardiology department with diminished exercise tolerance (WHO class III) and chest pain. The patient was treated with sildenafil and ambrisentan. Blood investigations revealed NT-proBNP elevated to 2650 pg/ml (norm: 0–125 pg/ml). Echocardiography disclosed a large atrial septal defect with a bidirectional shunting, enlarged right atrium and ventricle with reduced systolic function, dilated main pulmonary artery (65 mm) and both pulmonary arteries, and mild tricuspid valve regurgitation (Figure 1 A). Right heart catheterisation revealed suprasystemic pulmonary pressures (systolic/diastolic/mean 104/41/62 with systemic blood pressure at 98/71/82 (mm Hg)), mean pulmonary artery pressure 62 mm Hg, pulmonary capillary wedge pressure 11 mm Hg, cardiac index of 1.7 l/min/m2, and pulmonary vascular resistance of 15.87 Wood units. The computed tomography angiography (CTA) showed compression of the left main (LM) coronary artery due to an aneurysm of the pulmonary trunk, resulting in significant stenosis of the LM (Figure 1 B). The Heart Team decided to perform percutaneous coronary intervention (PCI) during which a 5 × 20 mm drug-eluting stent was successfully implanted in the LM artery and in the proximal segment of the left anterior descending artery (Figures 1 C, D). Post-PCI, the patient experienced no recurrence of angina. Upon discharge, the patient was prescribed dual antiplatelet therapy (DAPT), spironolactone, β-blocker, sildenafil, and bosentan. One month later, during a control visit, the patient remained free from angina, but a 5-fold increase in aminotransaminases was observed, leading to the replacement of bosentan with macitentan. The patient declined treprostinil therapy. Despite the increased risk of bleeding in patients with Eisenmenger syndrome [1], no complications of DAPT were observed. The appropriate management of patients with extrinsic LM compression secondary to pulmonary hypertension remains challenging. Among patients with low to moderate risk for coronary artery disease, CTA emerges as a suitable, non-invasive modality for the preliminary assessment. Contemporary evidence indicates that PCI facilitates long-term symptom improvement and is safe especially in cohorts with high surgical risk [2]. Galiè et al. reported that out of 45 patients treated with PCI for extrinsic LM compression, 41 experienced complete symptom relief [3].
Figure 1
A – transthoracic echocardiography, aneurysm of the pulmonary trunk, and dilated pulmonary arteries, B – computed tomography, compression of the left main (LM) coronary artery due to an aneurysm of pulmonary trunk, C – coronary angiogram (CA), compression of the LM accompanied by restricted blood flow to the left anterior descending artery (LAD) and to the circumflex artery (Cx), D – CA, LM after percutaneous coronary intervention
In conclusion, LM compression is a rare complication that should be suspected in Eisenmenger syndrome patients with angina symptoms. PCI and tailored PAH treatment may be a reasonable approach [4].








