Cardiac arrest is a critical event associated with high morbidity and mortality rates. Prompt and effective resuscitation measures, including cardiopulmonary resuscitation (CPR) and advanced cardiac life support (ACLS), are essential for achieving a return of spontaneous circulation (ROSC) and improving patient outcomes [1]. However, the restoration of circulation can be accompanied by complications, including chest wall injuries such as sternum and rib fractures. The reported occurrence of rib fractures following CPR ranges widely, with documented rates spanning from 13% to 97% [2]. These injuries, resulting from the forceful compressions and defibrillation procedures involved in resuscitation, can significantly impact respiratory function and contribute to prolonged ventilation, hospitalization, and increased morbidity [1, 2]. Multiple rib fractures are considered to be an independent risk factor associated with the development of pneumonia after resuscitation [3].
While the management of chest wall injuries after cardiac arrest has been addressed in the existing literature, there is a paucity of cases describing chest wall stabilization specifically in the context of patients undergoing cardiac surgery. The combination of cardiac surgery and chest wall trauma presents a unique challenge because the surgical procedure itself further compromises the stability of the thoracic cage. Despite the potential clinical significance, there is limited literature available on the management of chest wall injuries and subsequent stabilization required in this specific subset of patients [4–6].
The occurrence of chest wall injuries during cardiac surgery is a rare but important issue that deserves special attention. The consequences of such injuries can be significant, potentially leading to impaired respiratory mechanics, increased pain, prolonged mechanical ventilation, and delayed recovery [2]. Therefore, timely recognition and appropriate management of these injuries, including chest wall stabilization, are crucial to optimize patient outcomes and facilitate a smooth postoperative recovery.
This case report aims to shed light on the challenges and management strategies related to chest wall stabilization in patients who have undergone cardiac surgery following resuscitation. By highlighting the unique aspects of these cases and emphasizing the scarcity of literature in this area, we aim to contribute to the existing knowledge and promote further research into this important aspect of post-resuscitation care. A 73-year-old patient experienced an episode of sudden cardiac arrest at home, prompting the intervention of family members, who initiated lay resuscitation. Subsequently, the rescue team arrived after approximately 7 min and promptly intubated the patient, continuing resuscitative efforts for an additional 15 min. Following 2 defibrillations, spontaneous circulation, denoted as return of spontaneous circulation (ROSC), was successfully achieved. The patient was then transported to the local hospital where coronary angiography revealed the presence of severe 2-vessel coronary artery disease, characterized by high-grade stenosis in the medial region of the left main artery and further significant stenoses of the left anterior descending artery (LAD) and circumflex coronary artery (RCx). Based on these findings, the decision was made to transfer the patient to our hospital for cardiac surgery.
Emergency triple coronary artery bypass grafting (CABG) surgery was performed, involving anastomosis of the left mammary artery (LIMA) to the left ascending artery (LAD). Sequential revascularization of the obtuse marginal (OM) and first diagonal arteries was achieved using a saphenous vein graft. During the surgical procedure, the presence of a sternum fracture in the sternal body region and an unstable thorax due to multiple bilateral rib fractures was noted. Due to a notable bleeding tendency, simultaneous rib stabilization was deferred to avoid potential chest wall haematomas. The sternal fracture was stabilized using sternal wires in a figure-of-eight configuration. Postoperatively, the patient maintained stable cardiopulmonary status. However, due to persistent bleeding, the patient underwent revision surgery on the same day to achieve haemostasis and evacuate the haematoma.
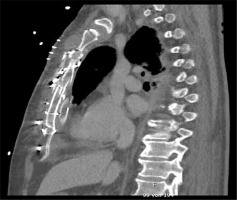
After successful weaning from mechanical ventilation, the patient was extubated on the 4th postoperative day. Nonetheless, flail chest with paradoxical respiratory movements persisted. Computed tomography (CT) imaging revealed bilateral rib fractures involving the 1st to 7th ribs on the right side and the 4th to 7th ribs on the left side. It also showed adequate stabilization of the sternum by the sternal wires (Figure 1). Despite non-invasive ventilation attempts utilizing a continuous positive airway pressure (CPAP) mask and high-flow nasal ventilation, the patient required reintubation on the 16th postoperative day due to respiratory insufficiency. Subsequently, the decision was made to proceed with osteosynthetic stabilization of the thorax, performed on the 19th postoperative day utilizing the Strasbourg Thoracic Osteosynthesis System (STRATOS, MedXpert GmbH, Heitersheim, Germany). The surgical intervention involved reopening the wound and identifying the ribs requiring stabilization. Small skin incisions were made to adequately expose the targeted ribs, allowing for the attachment and fixation of the rib clips. Subcutaneous tunnels were created to accommodate the placement of the connecting bars, which were subsequently connected midline. In this technique, a total of 3 ribs (3rd, 5th, and 6th) were stabilized, leading to the achievement of thoracic stability and normalization of respiratory mechanics (Figures 2, 3).
Figure 2
3D reconstruction illustrating the position of clips and bars in the Strasbourg Thoracic Osteosynthesis System (STRATOS, MedXpert)
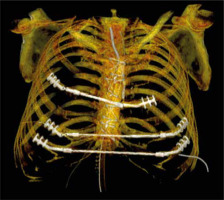
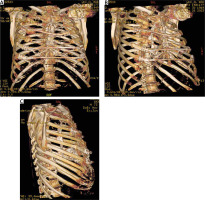
Figure 3
CT 3D reconstruction demonstrates the result of thoracic wall stabilization from various angles
Throughout the patient’s course, intercurrent lung infections were managed with antibiotics guided by the results of an antibiogram. On the 31st postoperative day, a percutaneous tracheostomy was performed, and after a prolonged weaning process, the patient successfully discontinued ventilatory support and gradually progressed in mobilization. However, the patient exhibited a moderately reduced ejection fraction (EF) and experienced frequent ventricular extrasystoles (VES), occasionally presenting as bigeminy with early coupling of the VES, resulting in presyncopal states attributed to a decrease in cardiac output. Furthermore, intermittent self-limiting ventricular tachycardias (VTs) were observed. Following consultation with the cardiology team, a decision was made to implant an implantable cardioverter-defibrillator (ICD), which was successfully performed on the 52nd postoperative day. Subsequently, on the 54th postoperative day, the patient was transferred to the normal ward for ongoing care. Here, further mobilization and physiotherapy interventions were implemented. Finally, on the 68th postoperative day, the patient’s stable general condition allowed for transfer to a rehabilitation clinic to continue the recovery process (Figures 4, 5). Successful cardiopulmonary resuscitation often requires intense efforts, including ACLS measures. However, the restoration of circulation can be accompanied by complications, including chest wall injuries, such as sternum and rib fractures [7]. Hoke and Chamberlain in their study demonstrated that conventional CPR resulted in rib fractures in a minimum of 30% of patients and sternum fractures in about 20% of patients [2]. Over the past few years, there has been a notable rise in the incidence and magnitude of skeletal chest injuries associated with CPR due to the wider and more aggressive application of the measures [4]. Moreover, the wider utilization of mechanical chest compression systems, such as piston devices during resuscitation, is necessary to achieve consistent and uninterrupted chest compressions. Nevertheless, the implementation of this technique carries the potential risk of inducing severe fractures in the thoracic rib cage, thereby posing a threat to the patient’s clinical progression [6].
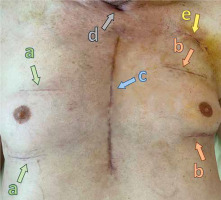
Figure 5
Surgical approaches for the patient’s thorax: a – right-side incisions for rib clip placement, b – left-side incisions for rib clip placement, c – median sternotomy, d – tracheotomy, e – ICD implantation
In this case, the patient experienced a sternum fracture and bilateral rib fractures during the resuscitation process. The subsequent cardiac surgery, specifically coronary artery bypass grafting (CABG), further complicated the patient’s condition. The sternum fracture was stabilized with sternal wires, while the decision to delay rib stabilization was made due to ongoing bleeding tendencies. The patient developed flail chest and respiratory insufficiency postoperatively, necessitating rib stabilization using the STRATOS MedXpert system. The successful intervention resulted in improved thoracic stability and respiratory mechanics, which allowed him to be successfully weaned from mechanical ventilation.
Chest wall stabilization following resuscitation is essential to promote optimal recovery and prevent complications. Rib fractures can lead to respiratory dysfunction, impaired cough, pain, and prolonged mechanical ventilation. Timely rib stabilization is crucial in achieving thoracic stability, reducing pain, facilitating respiratory mechanics, and minimizing the risk of associated complications. Immediate rib fixation has been associated with improved outcomes, and shorter mechanical ventilation duration and reduced intensive care unit (ICU) stay [1, 8, 9].
A thorough literature review reveals several techniques and approaches for chest wall stabilization. Plate fixation, intramedullary devices, absorbable mesh, and combinations thereof have been utilized in clinical practice. Plate fixation, with the application of titanium plates and screws, offers rigid stabilization but may require extensive exposure and dissection. Intramedullary devices, such as intramedullary splints or Kirschner wires, provide stability by connecting fractured ribs. Absorbable mesh offers an alternative approach, providing support during the healing process [10, 11]. Polymer cable cerclages can be employed to augment the plating technique in cases involving longitudinal fractures, rib fractures adjacent to the spine, osteoporotic ribs, and cartilage injuries. Among these, the 3rdto 8thribs are commonly subjected to plating [10]. It is generally recommended to perform surgical stabilization of rib fractures within the initial 7 days following trauma, preferably within the first 3 days [10, 12].
The technique used in our case is mainly applied in cases where stabilisation is needed after extensive resections of the thoracic wall due to primary malignancies or secondary tumour infiltrations [13, 14]. It has also been reported in cases of severe sternal dehiscence, which requires secondary surgical closure [15]. To our knowledge, the case we report is the first in the literature to be treated with the Strasbourg Thoracic Osteosynthesis System (STRATOS, MedXpert) in this setting. A singular case has been documented in which surgical intervention involving the utilization of a pectus bar was employed to treat a patient presenting with flail chest. In this case, the condition was a result of significant segmental rib fractures incurred during cardiopulmonary resuscitation performed to address a massive pulmonary thromboembolism [16].
Studies evaluating chest wall stabilization techniques have reported positive outcomes, including reduced pain, improved respiratory function, decreased complication rates, and shorter hospital stays [1, 9]. However, the optimal technique for rib stabilization remains a topic of debate, and further research is needed to compare outcomes and determine the most effective approach. Factors such as patient characteristics, fracture patterns, surgeon expertise, and institutional resources should be considered when selecting the appropriate method.
The optimal timing for chest wall stabilization following resuscitation, particularly in cases involving concurrent cardiac surgery, remains a subject of debate because data on this issue are scarce [11, 17]. Some may argue for simultaneous stabilization during cardiac surgery, while others may propose a delayed approach. It is generally accepted that early repair of bone fractures is beneficial for the healing process in most cases. Pieracci et al. suggest that the timing of surgical stabilization of rib fractures within 24 h of admission is influenced by specific demographic and physiological factors, and when accounting for potential confounders, early surgical stabilization can result in shorter operative times and is associated with positive outcomes [12]. However, in complex cases requiring additional cardiac surgery, careful consideration should be given to the indication for early repair. Performing chest wall stabilization simultaneously with heart surgery offers the advantage of addressing both the cardiac and chest wall injuries in a single operation, potentially reducing overall hospitalization and avoiding a second surgery. Moreover, performing a standard cardiac procedure involving a median sternotomy on an unstable chest could exacerbate the patient’s condition. This approach has been shown to be feasible and safe in select cases, where simultaneous rib fixation during cardiac surgery resulted in improved respiratory mechanics and reduced hospital stay in patients with sternal fractures and severe chest wall instability [4–6].
However, there are considerations supporting a delayed approach to chest wall stabilization. Postoperative bleeding is a concern, and immediate stabilization may contribute to haematoma formation. Delaying the procedure allows for adequate control of bleeding, optimization of the patient’s general condition, and resolution of coagulopathy. Moreover, in cases where the patient continues to exhibit haemodynamic instability even after weaning from cardiopulmonary bypass, it is crucial to carefully evaluate the benefits of chest wall stabilization against the potential increase in operative time for these individuals. Furthermore, it is important to note that in cases where an urgent resternotomy for revision is required, such as in instances of postoperative pericardial tamponade, the presence of a complex stabilization system, as in our case, may pose a hindrance. The potential delay caused by the removal of the system could have a significant impact on mortality rates.
Ultimately, the decision regarding the timing of chest wall stabilization after resuscitation and cardiac surgery should be made on a case-by-case basis, considering the patient’s condition, associated injuries, and the feasibility of simultaneous procedures. Collaboration between cardiothoracic surgeons and trauma specialists is crucial in determining the optimal management strategy. Further research and larger studies are warranted to establish evidence-based guidelines in this regard.
Moreover, patient management after chest wall stabilization is crucial for a successful recovery. This includes appropriate pain management, respiratory physiotherapy, and early mobilization. Adequate pain control is essential to facilitate coughing, deep breathing, and ambulation [18, 19]. Respiratory physiotherapy, including incentive spirometry, deep breathing exercises, and chest wall mobilization techniques, promotes lung expansion and clearance of secretions [20]. Early mobilization helps prevent complications such as pneumonia, deep vein thrombosis, and muscle deconditioning [21]. This case report highlights the importance of chest wall stabilization following cardiac arrest, resuscitation, and cardiac surgery. Rib fractures and thoracic instability can significantly impact respiratory function and patient outcomes. Prompt recognition of chest wall injuries and timely rib stabilization contribute to improved respiratory mechanics, reduced pain, and enhanced recovery. While various techniques and approaches exist for rib fixation, the choice should be based on patient characteristics, fracture patterns, surgeon experience, and institutional resources. Future research should focus on comparing different stabilization techniques and evaluating long-term outcomes in this patient population.