Damage to the vascular structures is an uncommon complication after total hip arthroplasty (THA) [1]. Due to their proximity to the acetabulum, the external iliac, femoral, and obturator vessels are most vulnerable to injury.
The early complications of a major vascular injury are mainly bleeding, ischemia, thromboembolic events, and lacerations while the late complications are arteriovenous fistula and pseudoaneurysms [1, 2]. As far as we know, there are no recent reports of acute iliofemoral deep venous thrombosis (DVT) and external iliac vein (EIV) injury after THA as a complication.
We describe here the first reported case of acute iliofemoral DVT and iatrogenic EIV after THA which was successfully treated with an appropriate endovascular approach.
A 62-year-old female patient underwent THA in the Orthopedic Department due to chronic osteoarthritis. The patient’s comorbid factors included heart failure, chronic obstructive pulmonary disease and obesity. There was no previous history of DVT or thromboembolism. The patient was referred to our clinic because of swelling, pain, redness and increased diameter of the left leg on the 5th postoperative day (Figure 1). The patient was diagnosed with acute iliofemoral DVT based on the present examination findings and color Doppler ultrasonography (CDUS) performed with a prediagnosis of DVT and scheduled for a rheolytic thrombectomy procedure.
The left popliteal vein was punctured with an 18-G needle under ultrasound direction. After insertion of an 8F introducer sheath, intravenous heparin (100 UI/kg) was administered. After ascending phlebography, an occlusion was detected in the iliofemoral segment (Figure 2), after which a 0.035-inch guidewire (Terumo, Boston Scientific) was passed through the occluded vein to the inferior vena cava (IVC) with minimal difficulty. Pulse spray thrombolysis was performed in the occluded iliofemoral vein segments using the Angiojet (Boston Scientific, Marlborough, Mass) device. Alteplase was not administered because of a history of major orthopedic surgery. After the second passage, a venogram was performed and extravasation of the contrast medium into the soft tissue of the pelvis was observed (Figure 3). It was suspected that there was an extravasation in the EIV related to injury by the screw-tip drilled into the pelvic bone to fix the metal back of the cup (Figure 3). Due to the comorbidities of the patient, open surgical repair was considered to be risky. As a result, it was decided that inserting a stent graft across the injured vein would be more appropriate. A 13 × 50-mm Viabahn endoprosthesis (W. L. Gore and Associates) was inserted across the wire and placed in the EIV at the location of contrast extravasation. The endoprosthesis was molded to the vein wall with a 14-mm angioplasty balloon (Boston Scientific). Post-procedure venograms showed normal flow across the EIV and femoral vein without extravasation (Figure 4).
Figure 3
Extravasation of contrast medium detected in the external iliac vein in the venogram (arrow)
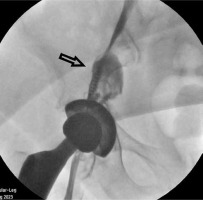
Figure 4
Normal flow without extravasation along the iliofemoral segment in the venogram after endoprosthesis application

Dramatic improvement was observed in the patient’s complaints on the first postoperative day (Figure 5). To reduce extremity edema, micronized purified flavonoid fraction (Daflon 500 mg) was administered twice daily as a venotonic agent. Additionally, to protect the patient from the high risk of bleeding associated with potential open surgical interventions due to possible complications and to provide anticoagulation, enoxaparin sodium was administered at a dose of 80 mg/kg twice daily. The patient was mobilized and discharged from the clinic on the 5th postoperative day with a prescription for rivaroxaban. One month after the procedure, CDUS and CT venography revealed patency of the stent graft without DVT. Clinically, the patient’s complaints of pain, cramps and edema regressed and the diameter difference between the legs disappeared. The patient was followed up under rivaroxaban treatment. The patient’s consent was obtained for publication of this case report.
EIV injury accompanying DVT is a rare complication after THA, specifically the acetabular component. As far as we know, there were no prior reports describing acute iliofemoral DVT as the presenting sign of venous injury after THA surgery. THA necessitates the placement of retractors around the acetabulum where extensive vasculature passes. Therefore, direct vessel injury during THA could occur as a result of placement of supplemental screws for fixation of the acetabular component [3]. In our case, it was suspected that the patient’s left EIV was injured as a result of predrilling holes for the anchoring of screws and pegs, the injury was self-limiting due to hematoma, and then acute iliofemoral DVT developed due to immobilization. Endovascular treatment with a stent graft might be preferable to the time-consuming open surgical procedure for such injuries [4]. In this case, which we initially treated for acute DVT, we decided to place a stent graft during the procedure due to the coincidental detection of the existing injury after clearance of the thrombus and the patient’s current general condition and comorbidities.
Vascular injury as a complication of THA is very rare with an incidence varying between 0.1% and 0.3%. However, when it develops it may cause a catastrophic clinical status. The most commonly affected vessels are the external iliac and femoral artery and vein [1]. Detecting and treating this condition promptly can reduce morbidity and mortality rates [5]. Vessel ligation, primary repair, bypass grafting, and/or embolectomy are varieties of open surgical procedures [6]. Open surgical repairs, on the other hand, are time-consuming and technically challenging procedures. Therefore, endovascular techniques will facilitate the surgeon in the treatment of vascular injury, especially in complex and time-consuming cases, if the patient has high comorbidity.
In previous publications, there was no recommendation as to which type of stent graft performs best in the venous system. However, the stent grafts to be implanted should be flexible and compatible with compression, especially in the iliac vein. Polytetrafluoroethylene may outperform Dacron in preventing early stent-graft thrombosis in the low-flow venous system [4]. In addition, because the diameter of the venous system is larger than that of the arterial system, it is recommended to place stent grafts with a larger diameter. For stenotic or occlusive venous disease in the common iliac vein, EIV, and femoral vein, the suggested stent diameters are 16, 14, and 12 mm, respectively [7]. In this case, in accordance with previous studies in the literature, we successfully implanted a 13 mm stent graft in the injured EIV and simultaneously treated the DVT.
In selected cases of iliac vein injury with severe comorbid factors, endovascular procedures may be performed as an alternative to open repair because they are less invasive. Accurate sizing and determination of venous anatomy are essential for appropriate stent graft selection.









