Summary
This study found that flow-mediated dilation (FMD) reduced the number of punctures required for radial cannulation and significantly increased the radial artery diameter during transradial coronary angiography. Additionally, FMD was found to reduce complications during transradial coronary angiography.
Introduction
Transradial coronary angiography is known to be the standard vascular access method for percutaneous coronary procedures, recommended as the primary diagnostic and therapeutic tool for both stable coronary artery disease and acute coronary syndrome, regardless of the patient’s clinical presentation [1–3]. In addition, the results of randomised controlled studies and meta-analyses have consistently demonstrated lower rates of access site bleeding and vascular complications with the transradial approach (TRA) [2, 3]. However, it is acknowledged that radial artery (RA) spasm remains one of the most common complications of TRA, potentially complicating sheath or catheter placement and extending procedure times, alongside the risk of RA occlusion and loss of pulsation [4]. To mitigate RA spasm during coronary angiography, various strategies have been proposed in the literature. One of them is the flow-mediated dilatation (FMD) method, which is created by pressure application to the brachial artery [5]. Reports suggest that the presence of FMD correlates with reduced TRA-related complications and improved success rates in puncture attempts [6].
Aim
Our study hypothesises that FMD may augment the RA diameter and reduce RA puncture attempts during transradial coronary angiography. Therefore, we conducted this investigation to compare radial angiography procedures in patients with and without FMD.
Material and methods
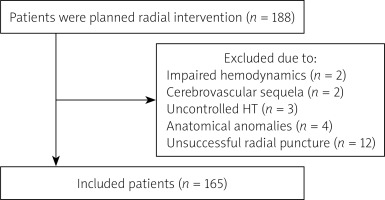
The study was conducted with approval from the Ethics Committee of our institution. This prospective, randomised, single-centre study aimed to evaluate the effect of FMD on radial artery RA diameter during TRA. The study encompassed consecutive patients admitted to the Cardiology Department between May 2021 and December 2021, who underwent transradial coronary angiography for stable coronary artery disease. Exclusion criteria comprised patients with impaired haemodynamics, a history of radial area intervention within the last year, cerebrovascular or other sequelae impacting the extremity intended for transradial intervention, and uncontrolled hypertension or arrhythmia. Patients with anatomical anomalies (tortuosity, cubital loops, bends, etc.) of the radial and brachial arteries were also excluded (Figure 1).
Procedure
Right RA was used for all procedures. All diagnostic and percutaneous coronary intervention (PCI) procedures were performed with 6F catheters. Comprehensive medical histories of enrolled patients were documented from the hospital registry system. Data regarding procedure duration and the number of attempted entries for successful RA cannulation were collected from nurse observation forms and coronary angiography recordings. The study protocol was approved by the local Ethics Committee of our institution.
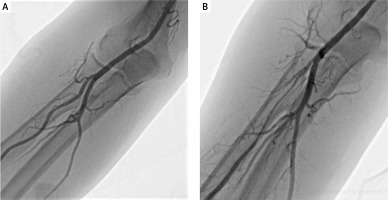
The patients were divided into 2 groups: those with and without FMD. Before coronary angiography, the modified Allen test was applied to the patients and the status of palmar collateral flow was evaluated. A blood pressure cuff was placed on the upper part of the antecubital region of the patients in the FMD group and inflated for 10 min, allowing the cuff pressure to rise to 30 mm Hg above the systolic blood pressure. In patients who did not undergo FMD, the blood pressure cuff was attached to the specified area but was not inflated. The cuffs of patients in the FMD group were rapidly deflated after 10 min, and RA cannulation was applied quickly. After appropriate local anaesthesia with 1–2 ml of 2% lidocaine solution injection, puncture was performed with a 21G needle, and a 6F regular radial sheath (Shun Guider, Shunmei Medical, Guangdong, China) was introduced in the RA. After the radial sheath was placed, a mixture of 200 µg nitroglycerin, 5 mg diltiazem, and 2000 IU unfractionated heparin was administered intraarterially, then radial angiography was performed within 1 min using 2–5 ml of contrast in both groups (Figure 2). RA diameters of the patients were measured by Siemens Artis Q Pure Angio (Germany) via quantitive coronary angiography method before transradial coronary angiography.
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics version 24.0 (IBM, Chicago, IL, USA). The normality of distribution of the data was assessed using a Kolmogorov-Smirnov test. Categorical data were presented as percentages, while continuous variables were presented as either mean ± standard deviation or as median and interquartile range depending on the normality of the variables. Continuous variables between study groups were compared using Student’s t-test. A p-value less than 0.05 was deemed statistically significant. Univariate linear regression analysis and a multiple linear regression model were utilised to identify factors contributing to RA diameter. Conventional clinical variables such as age and gender, along with other parameters showing significant correlations, were included in the regression model.
Results
A total of 165 patients were included in the study, of whom 64 (38.8%) were women. The mean age of the patients was 55.6 ±10.2 years. The FMD group included 80 (48.5%) patients. Comparison of demographic information, physical examination findings, coronary angiography procedure parameters and laboratory values of both groups are given in Table I. Except for diabetes mellitus, there were no notable distinctions in basal demographic characteristics including age, gender, cardiovascular risk factors, medical history, clinical presentation, or medications between the 2 groups. Accordingly, patients in the group without FMD exhibited a slightly higher prevalence of diabetes (p = 0.035). Regarding coronary angiography procedure parameters, the number of punctures required for successful transradial cannulation was significantly higher in the group without FMD (1.55 ±0.68 vs. 1.20 ±0.43; p < 0.001). Additionally, ulnar and brachial artery diameters were measured before the procedure, with values presented in Table II. Ulnar and brachial artery diameters were observed to be larger in the FMD group compared to the control group (4.58 ±0.51 vs. 4.35 ±0.56, 6.13 ±0.67 vs. 5.83 ±0.78, respectively; p = 0.007 for both comparisons).
Table I
Demographic information, physical examination findings, procedure parameters, and laboratory values
[i] Continuous variables are presented as mean ± SD or median (IQR); categorical variables are presented as frequency (%). ALT – alanine aminotransferase, AST – aspartate aminotransferase, BMI – body mass index, DBP – diastolic blood pressure, Hb – haemoglobin, HDL – high density lipoprotein, K – potassium, LDL – low-density lipoprotein, Na – sodium, SBP – systolic blood pressure, TSH – thyroid stimulating hormone.
Table II
The radial, ulnar, and brachial artery diameters of the patients in FMD and control groups
Linear regression analysis provided predictors of RA diameter. Clinically significant and laboratory variables were included in the analysis. In backward linear regression analysis, a history of diabetes and undergoing FMD were identified as significant predictors for RA diameter (Table III). Furthermore, RA diameter was re-evaluated in the diabetic subgroup, revealing that the radial artery diameter remained larger in the FMD group (3.00 ±0.35 vs. 2.78 ±0.26, p = 0.036). Radial puncture attempts were also compared between both groups, with significantly higher attempts observed in the control group compared to the FMD group (1.55 ±0.7 vs. 1.20 ±0.64; p < 0.001).
Table III
Linear regression analysis for the independent predictors of radial artery diameter
Discussion
Current studies demonstrate that FMD facilitates radial access and is an effective, noninvasive, and nonpharmacological approach in reducing RA spasm. Repeated unsuccessful puncture attempts, in particular, significantly contribute to the occurrence of RA spasm [7]. In our study, it was observed that the FMD created by pressure application significantly increased the RA diameter even in diabetic patients during transradial coronary angiography. Secondly, the number of punctures required for successful transradial cannulation was found to be significantly lower in patients who underwent FMD. These results show that FMD is an effective, non-invasive, and non-pharmacological method with a high success rate in reducing RA puncture attempt.
Compared to the transfemoral approach, TRA increases patient comfort and is preferred by patients over the femoral route, while reducing the complications that may be associated with the procedure itself and the risk of bleeding [8], as well as the duration of hospitalisation and related costs [8, 9]. Although it is widely used due to all these advantages, this benefit may disappear due to radial spasm in some patients. RA spasm presents a significant challenge during puncture for coronary angiography or PCI, impacting the success of the TRA and potentially necessitating a change in the access site [10].
It is well-documented that cannulation of the arterial system with a sheath during coronary angiography induces temporary endothelial dysfunction [11]. This endothelial dysfunction leads to arterial spasm due to reduced release of nitric oxide, an endothelium-related vasodilator, and decreased levels of endothelium-related hyperpolarising factor. Furthermore, catecholamines released in response to guidewire, sheath, or catheter manipulation in the vessel contribute to constriction via alpha1 receptors [12].
Despite the routine administration of cocktails containing nitrates and nondihydropyridine group calcium channel blockers to increase RA diameter and prevent spasm following sheath insertion during transradial coronary angiography, RA spasm may persist. An increase in the number of puncture attempts for cannulation and prolonged procedure duration exacerbate endothelial dysfunction caused by sheath insertion [13]. FMD emerges as a potential method to mitigate these complications.
In FMD, vasodilation occurs due to increased shear stress secondary to heightened flow. Endothelial nitric oxide synthase activity plays a pivotal role in this process, alongside the release of other endothelium-derived substances. FMD can be categorised into 2 subgroups: endothelium-dependent and endothelium-independent. Endothelium-dependent FMD harnesses the increased flow following the removal of flow restriction in the vessel, while endothelium-independent FMD enhances vasodilator response through substances like nitroglycerin, which contains nitric oxide [14]. As a result of various studies, FMD has been tried during transradial coronary angiograph procedures, and successful results have been obtained. Taniguchi et al., in a randomised controlled study of 54 patients, tested the effect of FMD performed with the extended arm occlusion method on the RA diameter before transradial coronary angiography. As a result of this study, it was observed that the RA diameter after the procedure was larger in patients who underwent FMD compared to the other group. In addition, the change in RA diameter before and after the procedure was compared using Doppler ultrasound, and similarly, the diameter change was found to be significantly higher in the FMD group [15]. Unlike this study, we compared RA diameters with radial angiography instead of arterial Doppler ultrasound, which is a more sensitive method in our study. Furthermore, Taniguchi et al. investigated only RA diameter while we also compared the number of radial puncture attempts, which was significantly lower in the FMD group. In the RADIAL study, the effect of FMD provided by prolonged arm occlusion on transradial coronary angiography complications was evaluated in 1156 patients, and there was a significant decrease in RA pulse loss and cannulation failure rates, and similarly to our study, the number of punctures required for successful cannulation in was also decreased in the FMD group [16]. Based on both our study’s findings and those reported in existing literature, it appears that RA diameter directly influences the number of punctures required for successful cannulation.
To our knowledge, our study is unique in terms of measurement of vessel diameters by angiography after FMD application. In all previous studies with FMD, vessel diameters were measured by Doppler USG, which is less sensitive than the methods used our study. In this sense, our study is unique.
In our study, we explored predictors of RA diameter and assessed the diameters of the ulnar and brachial arteries using angiographic imaging rather than Doppler ultrasound. Linear regression analysis revealed that a history of diabetes was a significant predictor of RA diameter. Consequently, we re-examined the effect of flow-mediated dilatation FMD on RA diameter within the subgroup of patients with diabetes. We believe that our study’s findings in this regard are particularly noteworthy.
The diameter of the RA seems to play a crucial role in determining the number of radial punctures required. Deftereos et al. demonstrated in their study that FMD serves as a predictive factor for RA spasm preceding transradial coronary angiography. They noted a significant reduction in RA spasm in the group experiencing an average 5% increase in RA diameter, as evaluated by ultrasound before and after FMD, compared to the group with a lesser increase (1.8%) [17].
In contrast to the study by Deftereos et al., our investigation did not involve a direct comparison of RA diameter before and after FMD using ultrasound. Instead, we measured RA diameter angiographically in groups with and without FMD. Consistent with previous evidence, our study revealed that the FMD group exhibited a significantly wider RA diameter. The positive impact of this favourable effect on RA puncture intervention was reaffirmed in our findings.
Limitations
The limitations of our study include the relatively small number of patients and the non-randomisation of the groups. In addition, the presence of coronary artery disease in the patients may have affected these results because the relationship between the presence of coronary artery disease and endothelial dysfunction is unknown.
Conclusions
In our study, inducing FMD through arm occlusion resulted in a reduction in the number of punctures needed for radial cannulation and a significant increase in radial artery diameter during transradial coronary angiography. Based on these findings, we believe that this procedure could be considered to mitigate complications before transradial coronary angiography in patients. Notably, it is noninvasive and entails no additional financial cost.