Introduction
Ingestion of foreign bodies (FBs) is a serious problem that can lead to morbidity and mortality in early childhood [1].
It predominantly occurs in children aged 6 months to 5 years, mainly around the age of 4 years. At this age, kids habitually tend to put small objects in their mouth to explore the surrounding environment; they may lack teeth for grinding up food into tiny pieces for swallowing, tend to play while eating, and do not have the cognitive capacity to differentiate between edible and inedible objects [2]. Recently, reports suggest an increased frequency of cases among children, as in a study from 1995 to 2015 in the USA, which revealed an elevated rate of 0.95% to 1.8% [3].
Oesophageal foreign bodies, either sharp or blunt, can pass through the digestive tract when they reach the stomach, but larger materials are somewhat difficult to pass, so endoscopy is needed to retrieve them [4]. The ingested oesophageal foreign body usually stops in a part of the gastrointestinal tract that is anatomically and physiologically constricted, like the oropharynx, a crossing site between the aorta and the left main bronchus, and the lower oesophageal sphincter [4].
The most common foreign bodies swallowed are coins. It has been reported that foreign bodies are usually passed uneventfully in 80–90% of patients, while 10–20% of patients may require endoscopic intervention to remove them, and 1% may require operative extraction [5, 6].
Complications are not common, but when they occur, erythema, erosion, ulcers, and sometimes even perforation may present. Necrosis was found in a few cases, especially with a button battery lodged in the oesophagus, and endoscopic intervention was delayed [7].
The most common finding in coin ingestion is erosion, followed by erythema or oedema. Regarding sharp object ingestion, perforation occurs in 12.5% of cases and necessitates urgent surgical intervention [8].
Aim
The aim of the study is to estimate the pattern of foreign body ingestion among children and identify the role of management and its outcomes in relation to the type and site of foreign bodies.
Material and methods
Our study was carried out on patients who attended the Emergency Department of the Rapareen Teaching Hospital for Paediatrics in Erbil City and were referred to the Paediatric Gastroenterology Unit between March 2019 and January 2023. Admission complaints, demographic data, radiological findings, foreign body localization, how the foreign body came out, the type of foreign body recorded, and management outcome were recorded. We did not include patients who had been managed by the ENT Department and were in the pharynx or upper airway. Ethical consideration was taken from patients or caregivers after explaining the objectives of the study, and it was approved by the Ethics Committee at Hawler Medical College.
Statistical analysis
Data were subjected to descriptive analysis based on frequency and percentage distribution using SPSS version 25. Crosstabulation was utilized to examine the relationship between foreign body site and type with different variables among research participants. Pearson’s χ2 test and the exact probability test for small frequency distributions were used to test the relationships, while the independent T-test was used for means.
Results
Fifty-four patients visited or were admitted to the Rapareen Hospital Emergency Department with a history of ingestion of foreign bodies, with a median age of 4 years (minimum age of 1 year and maximum age of 12 years, mean age of 4.14 ±2.15 years) and a nearly equal male-to-female ratio (1.16 : 1). Only 19 patients were symptomatic, while others were not, and 61.1% presented within the first 24 h. Most of the foreign bodies were radiopaque and mainly located in the oesophagus at the time of the initial visit, and this made endoscopic intervention successful in most cases, except for 4 cases where the ingested materials extended beyond the duodenum. Complications were reported in 13 cases (Table I). The site of the foreign body at the time of presentation was significantly associated with early presentation (≤ 24 h) and outcome, as assumed with higher-located substances extracted endoscopically rather than surgery or awaiting spontaneous evacuation (Table II). Coins, compared to others, were located significantly higher in the gastrointestinal tract and could be easily withdrawn endoscopically, as shown in Table II.
Table I
Characteristics of patients who presented with foreign body ingestion
Table II
Association between site of foreign body and demographic and clinical data
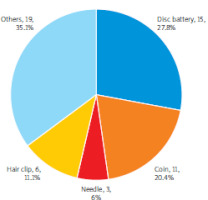
Disc batteries were the commonest foreign body among the studied children (Figure 1), and coins were next, which is surprising as no more Iraqi coins have been introduced since around 25 years ago, but most of them were either foreign or old Iraqi coins. Others include needles, hairclips, AA batteries, magnets, covers, bottle caps, screws, nails, bezoars, stones, toothbrushes, silica gel, praise, rings, and earrings. One patient had food impaction with endoscopic findings of short segment stricture. The method and endoscopic equipment used for extracting materials vary according to site and type, decided according to initial assessment and radiological appearance, as shown in Figure 2. Most of them were extracted either by forceps or Roth net retrieval devices.
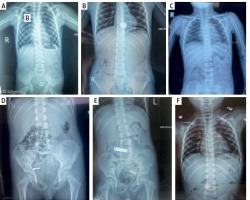
Figure 2
Different radiopaque foreign bodies: A – Screw cap in distal colon. B – Coin in lower oesophagus. C – Ring in lower oesophagus. D – Nail in intestine. E – AA battery in intestine. F – Two needles in intestine
When clinical and demographic data were studied in association with the type of foreign body, as demonstrated in Table III, younger age and male sex were significantly related to disc battery consumption in contrast to coins, which were more frequent among older children and female gender. Coins were again responsible for the majority of cases that presented early (≤ 24 h), followed by button batteries. The fate of objects is associated significantly with the kind of foreign body; blunt objects like disc batteries and coins never underwent surgery, unlike sharp items like needles.
Table III
Association of foreign body type with demographic and clinical data
Discussion
Foreign body ingestion among children is not uncommon, and sometimes symptomatic patients need urgent intervention with endoscopy or even surgery. In this study, 54 patients were included, and there was no significant gender predominance. This is true for most published articles; male patients were slightly more common, at 5–10%, than female patients [2, 5, 9–11]. One study involving 1000 cases found male predominance among toddlers compared to younger infants or older children [12].
As assumed, most children were around 1–5 years old, and a mean or median of 4 years was most frequently reported, as in the present study, because they are unable to predict the risks of swallowing such things [2, 5, 9, 12, 13]. The variations in age group and others may be explained by sample selection, as some studies included only toddlers, while others included respiratory inhalation in older patients.
Most of the swallowed bodies were disc batteries, followed by coins, and then others. This is unlike the majority of studies because coins represent the most frequently ingested bodies in Iran and many other countries [2, 9, 11, 13–15] and may account for more than 60% of registered cases, except for a study in Sri Lanka [10] in 2013 that included 53 patients and resulted in 24.5% of ingested materials being button batteries, while coins were second despite the availability of coins in their currency. In Table III of this article, the younger age group is more prone to button battery consumption, which is contrary to most reports [12, 14] that reveal coins dominating through different age groups. This is probably explained by the absence of coins here in our community for more than 25 years. Most of the reported coins in our work were foreign.
Symptoms like dysphagia, abdominal pain, and vomiting may be reasons for consultation, but these were not frequent among the studied patients, in agreement with other reports [9, 12–14]. A review of the medical reports of 165 children during a period of 5 years in Turkey revealed that only 34 (20.61%) had no symptoms, and they recruited those with ENT and respiratory manifestations [1]. Thirty-three patients presented within 24 h, even when asymptomatic, justified by evolving awareness about the hazards, especially button battery ingestion, and the availability of paediatric endoscopy in the paediatric teaching hospital; most papers share the same quick consultation response [1, 5, 11].
When crosstabulation was done relating the type of ingested body with certain variables, gender, age, and time of initial presentation were significantly associated, although those symptomatic were not. Button batteries or larger-diameter materials usually present earlier because they are dangerous and alarming. Navia-Lopez et al. published data supporting this with a coin diameter of 2 cm or more, mainly located in the oesophagus, and presenting earlier, while their age was younger than other children (below 5 years) [8].
The vast majority of materials were radiopaque and mainly located in the oesophagus, and this is probably true in most studies [1, 12, 14–16] despite differences in methodology and sample inclusion criteria. A study in Saudi Arabia resulted in 36.6% being radiolucent, the highest rate among the reviewed studies [14].
In the recent study, the location of the ingested materials was significantly associated with the time of initial manifestation, as expected, i.e. they were higher located and earlier presented; furthermore, a significant association was established between gender and later clinical consequences and intervention. Disc batteries are responsible for most of the damage when located in the oesophagus, because leakage of its contents and its pressure effect can cause caustic injury and necrosis, respectively [8].
The outcome varies according to the time of presentation, site, and type of ingested body; many would have passed spontaneously without complications or intervention [10–12, 16].
The size, sharpness, and shape of the ingested foreign body are some characteristics that should be taken into consideration when a medical professional has to deal with this condition. The risk also increases when the size of the object is greater than 5 cm or has a pointed shape [17, 18]. Four cases underwent laparoscopy and/or laparotomy due to complications and failure to reach them by endoscope; this is not very different from reports that include a large sample size [9]. In India, 80–90% of foreign bodies were asymptomatic and passed smoothly, while 10–20% were extracted endoscopically, and 1% underwent surgery due to complications [11]. Surgery in this study was done for uncommon foreign bodies like needles or screws, but not for coins or button batteries, and this could be explained by the fact that sharp objects that could not be extracted early and were prone to complications necessitated surgical intervention. The laparoscopic approach before open surgery could be performed safely for the removal of an ingested foreign body. Laparoscopic, minimally invasive surgery should be preferred to open surgery due to its advantages [19].