Introduction
Tyrosinaemia type I (TT1) MIM 276700 is a rare hereditary metabolic disease caused by deficiency of the enzyme fumarylacetoacetate hydrolase (FAH), which is involved in the breakdown of tyrosine. This results in the production of alternative metabolites: 4-maleylacetoacetate, fumarylacetoacetate, and their derivatives: succinylacetoacetate and succinylacetone, compounds that damage the liver, kidneys, and peripheral nervous system.
Undiagnosed/untreated, it inevitably results in damage to the above organs/systems and premature death.
The prognosis for TT1 patients has improved significantly since 1992 with the approval of nitisinone. Nitisinone prevents the formation of toxic metabolites, but because it blocks the breakdown of tyrosine at an earlier stage, treatment causes tyrosine and phenylalanine serum levels to rise, making it necessary to maintain a low phenylalanine and tyrosine diet.
As with any chronic disease, one of the key questions in TT1 is how it affects the psychosocial functioning of patients. The number of publications on the topic has been on the rise in recent years [1–5]. Given that knowledge about rare diseases expands, among other things, through individual case studies and case study summaries of disease course in relatively small groups, we decided to present a summary of cases observed at a single treatment centre.
The aim of this paper is to assess the relationship between variations in serum tyrosine and phenylalanine levels and measures of socio-emotional functioning.
Material and methods
The study included 12 patients of the Department of Paediatrics, Nutritional and Metabolic Diseases at the Children’s Memorial Health Institute born between 1994 and 2012; 8 girls and 4 boys.
Detailed patient characteristics are provided in Table I.
Table I
Patients’ clinical characteristics
All cases were diagnosed by detection of succinylacetone in urine (by GC-MS method).
With the diagnosis established, all patients were started on nitisinone and a low-protein diet. Following health stabilisation, they came back to our centre every 3 to 4 months for clinical evaluation, laboratory and imaging tests, and to check compliance with dietary restrictions. During these routine follow-ups the patients’ psychosocial function was assessed. The evaluation was performed by a clinical psychologist. Participation was voluntary.
The psychological evaluation was performed using the parent form of the Child Behaviour Checklist (CBCL)/4–18. The Child Behaviour Checklist CBCL/4–18 is an established diagnostic instrument used, among other applications, in the assessment of TT1 patients. Developed by Thomas M. Achenbach, it is a component of the Achenbach System of Empirically Based Assessment (ASEBA) battery of tests. CBCL/4–18 is a screening test detecting the presence of emotional and behavioural problems in children 4 to 18 years of age. The issues evaluated in the checklist make up 8 scales related to problem behaviour: withdrawal, somatic complaints, anxiety and depression, social problems, thought problems, attention problems, rule-breaking behaviour, and aggressive behaviour.
Additionally, the patients’ IQ was measured using the Stanford-Binet 5 (SB5) Intelligence Scale developed by G.H. Roid. The scale comprises 10 subscales measuring the 5 main aspects of intelligence: fluid reasoning, knowledge, quantitative reasoning, visual-spatial processing, and working memory. Complete test results include the total IQ score, verbal IQ, and nonverbal IQ, with a mean score of 100 and standard deviation of 15 points.
Serum tyrosine and phenylalanine levels were measured at each follow-up visit for TT1. Patients differed in terms of treatment duration and age, which means that the numbers of tyrosine and phenylalanine measurements were also different. This is why the main index of tyrosine and phenylalanine variability adopted in the study was their fit to a linear trend. We adopted R2 as the coefficient of variation, with higher R2 values indicating better fit to a linear trend, and lower R2 worse fit to a linear trend, which translated to greater variability of tyrosine and phenylalanine levels over time. Standard deviation (SD) is the widely accepted measure of variation; however, SD fails to account for the sequence of measurements, unlike time (linear) trends. R2 values for tyrosine and phenylalanine were correlated using Spearman’s rho with the values of CBCL variables.
Statistical analyses were performed using the PASW software suite version 26.
Ethical standards
Parents provided informed consent for their children to participate. Additionally, pursuant to regulations in Poland, patients aged 16 years and older were also asked to provide assent for participation in the study. The design of the study was approved by the local Ethics Committee.
Results
Eleven children were diagnosed on the basis of clinical symptoms: the dominant symptom was liver dysfunction in 7 of them, liver dysfunction and tubulopathy in 2, and tubulopathy in 2. One patient was diagnosed pre-symptomatically by selective screening due to family history. In 5 patients, the onset of symptoms was early, within the first 6 months of life. The median age of diagnosis was 9 months (range 0–34 months). Mean time between symptoms and diagnosis was one month, but in one patient (with chronic tubulopathy) the delay between the onset of symptoms and diagnosis was longer: 21 months.
The SB5 test showed that the total score of intellectual and cognitive function was within the norm for all patients in the study. In 7 of the children, the score was within the range of average intelligence, with a mean value of 101 points. In 5 children the intelligence was below average, with a mean of 80 points (below 1 SD), placing them within the lower limit of normal.
Descriptive statistics for tyrosine, phenylalanine, and CBCL variables are shown in Table II.
Table II
Descriptive statistics
The next step in the analysis was to determine the relationships between emotional-behavioural indices (CBCL) and the measure of tyrosine and phenylalanine variability (Table III).
Table III
Spearman’s rho correlation between tyrosine and phenylalanine variability and emotional-behavioural measures
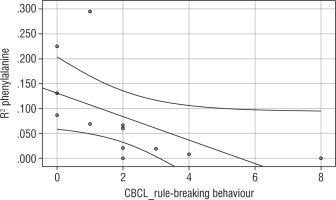
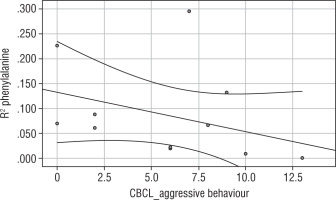
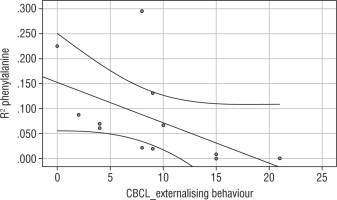
Significant correlations are additionally illustrated with graphs (Table III, Figures 1–3).
Correlation analysis yielded a negative relationship between phenylalanine variability and severity of rule-breaking behaviour (rho = –0.862; Fig. 1), severity of aggressive behaviour (rho = –0.578; Fig. 2), and the category of externalising behaviour (rho = –0.721; Fig. 3).
This suggests that higher variability (lower phenylalanine R2) means greater severity of rule-breaking, and aggressive and externalising behaviour.
Discussion
Initially, following the discovery of the effectiveness of nitisinone in TT1, papers on the outcomes of treatment in affected children focused mainly on metabolic control [6–8]. However, as the survival rates increased significantly, and so did the follow-up of patients on treatment, attention began to be drawn to problems emerging in everyday life. Consequently, the number of published papers on intellectual, attention, motor, and socio-emotional development in patients with TT1 treated with nitisinone and a diet has been increasing each year [1–5]. These studies have followed a variety of designs.
In 2022, van Vliet [9] published a comparison between neurocognitive outcomes and mental health in children with phenylketonuria (PKU) and TT1, and healthy controls. In her research she found that cognitive and behavioural difficulties in TT1 patients were more pronounced than in those suffering from PKU. The most commonly reported ones included problems in attention and memory processes, and the resulting general intelligence deficits. In addition, TT1 patients often face social problems, which manifest as difficulties with emotional control. These studies are based on statistics examining differences in means in controls vs. TT1 and PKU groups.
In another paradigm, research focuses on investigating the associations between biochemical parameters measured during follow-up evaluations of TT1 patients and indices of cognitive and behavioural function [3, 5]. Because correlation studies examine the relationship between 2 variables, this leaves the problem of choice of measurement, and therefore the value of a given variable to be taken into account. Sometimes authors analyse correlations between mean values of biochemical parameters obtained throughout the follow-up period of an individual patient [5]. In other cases, they examine correlations between values from the beginning of the treatment process or those obtained in the last year [4, 10].
An approach in which an attempt is made to capture the dynamics of change of individual parameters within a person is particularly close to us. One of our previous papers tackled this issue, pointing out that individuals with TT1 found to have attention deficits also had greater tyrosine level variability. Additionally, in that study we found a negative correlation between attention deficits and verbal scale scores in WAIS-R. This result may suggest decreased ability for verbal reasoning, comprehension, and verbal expression, as well as school difficulties.
In the present study we focused on assessments with the CBCL as an instrument especially suited to a comprehensive evaluation of adaptive and dysadaptive behaviour. The result of the assessment is a profile of adaptive function and internalising (i.e. causing subjective psychological tension) and externalising (i.e. involving external conflicts) behaviour.
Chronic disease patients require ongoing care, frequently alongside permanent lifestyle and behaviour modifications to help them adapt to the often-unpredictable course of their disease. Psychosocial functioning of children with TT1 and their parents is affected by multiple factors. For example, challenging (externalising) behaviour may occur in response to the disease status, limitations imposed by treatment, parental attitudes, peer relationships, etc. Difficulties in adjusting to the disease may also be caused by problems in maintaining appropriate levels of biochemical parameters during treatment. Volatility of monitored parameters or difficulty stabilising them may cause anxiety and, consequently, adaptation problems manifesting in psychosocial functioning difficulties. We considered drawing attention to this aspect of the disease to be important as a way to reduce the negative effects of TT1 on how patients functioned.
In our research we found that higher variability (lower phenylalanine R2) correlated with greater intensity of rule-breaking, and aggressive and externalising behaviour.
The Anastasoaie et al. [11] study in children with PKU also showed that variability of blood phenylalanine was more closely related to cognitive outcomes than the mean lifetime PHE level. In turn, Villet et al. [10] found that both internalising and externalising behaviour problems were associated with low phenylalanine (and associated lower tyrosine) concentrations during the first year of life, while high tyrosine (and associated higher phenylalanine) concentrations later in life and specifically the last year before testing were associated with more internalising behaviour and/or HR-QoL problems. The fact that the levels of 2 amino acids, phenylalanine and tyrosine, whose concentrations affect the levels of CNS neurotransmitters, at 2 radically different phases of treatment, translate into the magnitude of specific behaviour was another reason to examine the significance of serum phenylalanine and tyrosine variability for social and emotional functioning. The key difference between our and van Vliet’s study is that in the latter specific threshold concentrations of phenylalanine and tyrosine were analysed separately at various phases of treatment, while we approached treatment as a continuous process with its characteristic dynamics.
Given that phenylalanine is an exogenous amino acid, achieving desired (more stable) concentrations may be easier. Still, in a real-life setting, following a restrictive diet is a challenge, especially in the case of older children who are no longer subject to full parental control.
Limitations
Our study has certain limitations that are worth pointing out. The first is the number of subjects. Increasing the sample size in future research would boost the confidence of conclusions regarding the treatment of patients with TT1.
CBCL is one of many instruments used in the assessment of emotional and behavioural functioning. Including other instruments in the study would provide valuable information for professionals working with children suffering from TT1.
Due to unavailability of data, we were unable to analyse correlations with nitisinone serum concentrations, but in a future prospective study it would be a good idea to investigate such correlations. Given how rare TT1 is, a multicentre study seems to be the most promising design.
Conclusions
The SB5 test showed that total score intellectual and cognitive function was within the norm for all patients in the study. In 7 of the children, the score was within the range of average intelligence, with a mean value of 101 points. In 5 children the intelligence was below average, with a mean of 80 points (below 1 SD), placing them within the lower limit of normal.
Phenylalanine variability over time correlates with measures of emotional and behavioural functioning in TT1 patients. This relationship holds true for externalising behaviour, associated with the experience of maladjustment and aggression.
In the treatment of TT1, to maintain better quality of life for patients and their families in terms of emotional and behavioural functioning, it may be important to avoid spikes (significant fluctuations) in phenylalanine levels.
Regular, detailed psychological evaluations are recommended to detect potential problems as soon as possible and implement interventions aimed at achieving the best possible individual development and realise the intellectual and behavioural potential, thereby improving the patient’s and her family’s quality of life.

 ENGLISH
ENGLISH