Introduction
Gastric cancer is one of the main causes of death worldwide. In terms of cancer-related mortality, it is the fourth most common oncological disease. Gastric cancer requires healthcare expenses from society [1].
The main risk factors for gastric cancer are Helicobacter pylori (H. pylori) and Epstein-Barr virus (EBV) infection, smoking, the consumption of certain types of food (such as broiled, smoked, and salt-preserved food), and family history (familial gastric cancer incidence is higher in people with far-east Asian ethnicities, such as those from China and Japan) [1].
There are various, diverse forms of gastric cancer. They are classified and systematized in the International Classification of Diseases for Oncology (ICD-O-3, first revision) and the International Classification of Diseases (ICD), 11th edition [2, 3]. Aetiological, pathomorphological, and diagnostical characteristics are described in the WHO Classification of Digestive Systems Tumours (the latest edition refers to ICD-10) [4].
It was recently shown that the incidence of gastric cancer has been constantly dropping in most of the world [5].
The phenomenon of this decrease is rather difficult to understand. It includes several factors to be considered, such as health lifestyle trends, possibilities of diagnosis and prevention, identification of the genetic markers that are associated with a higher risk of gastric cancer, successful eradication of H. pylori, and updated understanding mechanisms of its persistent infection of the gastric epithelium [1, 5].
Adenocarcinoma not otherwise specified (adenocarcinoma NOS) is one of the most common types of gastric cancer in the world. It is a polyaetiological disease, and only 10% of cases have familial origin [4]. Authors often refer to gastric adenocarcinoma as adenocarcinoma NOS [2, 4].
Analysis of the nosological structure of gastric cancer epidemiological data is helpful to understand the dynamics of the incidence rate and understand what measures should be taken for further effective disease prevention.
Aim
The main aim is to analyse the nosological structure of the epidemiological data regarding gastric cancer in Ukraine from 2003 to 2020.
Material and methods
Epidemiological data were requested and obtained from the National Cancer Registry of Ukraine [6]. The request contained the codes of oncological units according to ICD-O-3 [2, 4]. Only cases with “stomach” as the primary site of “cancer” localization were selected for the study; the primary diagnosis according to ICD-10 was gastric cancer. The incidence rate was calculated per 100,000 people-year, part for each nosological form of the total number of cases, and the median was presented with 95% CI. R2 (coefficient of determination) was calculated to assess the trends with regression analysis using exponential regression. The data were analysed by use of MedCalc® Statistical Software version 22.009 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2023).
Results
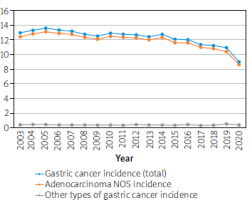
The highest incidence rate was noted in 2005, and the lowest rate was in 2020 (Tables I, II). The decrease in the incidence rate was 30.63% in 2020 compared to 2003, which is the beginning of the time frame (p < 0.0001), and 33.70% compared to 2005 (p < 0.0001). The lowest drop was observed between 2019 and 2020, when it reached 17.97% (p < 0.0001) (Figure 1).
Table I
Incidence rates of stomach cancers in Ukraine from 2003 to 2008 per 100000 people-year
Table II
Incidence rates of stomach cancers in Ukraine from 2009 to 2014 100000 people-year
A total of 30 different forms of primary gastric cancer were identified in Ukraine from 2003 to 2020. In the tables shown, only the forms of gastric cancer that were diagnosed over this specific time frame have been listed. The following 8 permanently occurring forms of gastric cancer were identified: adenocarcinoma NOS (8140), adenocarcinoma scirrhous (8141), intestinal type adenocarcinoma (8144), diffuse type adenocarcinoma (8145), adenocarcinoma tubular (8211), solid adenocarcinoma (8230), neuroendocrine tumour (8240), and papillary adenocarcinoma (8260) (Tables I–III). These forms were diagnosed every year from 2003 to 2020 in Ukraine.
Table III
Incidence rates of stomach cancers in Ukraine from 2015 to 2020 100000 people-year
The following 4 forms of gastric cancer were not diagnosed in some years: adenomatous polyp (8210) (no cases in 2018), neuroendocrine carcinoma (8246) (no cases in 2003–2009), adenocarcinoma in tubulovillous adenoma (8263) (no cases in 2014 and 2020), and clear cell adenocarcinoma (8310) (no cases in 2019) (Tables I–III).
Among those 4 cases, the most interesting is neuroendocrine carcinoma. It was not diagnosed from 2003 to 2009, both years inclusive, but the incidence rate in 2010 was 0.01. This figure increased over time to over 9-fold higher in 2019 (p < 0.0001). The increasing trend is reliable over the indicated time frame (R2 = 0.82; p < 0.0001) (Tables II, III).
Most cases were of adenocarcinoma NOS (Tables I–III). Adenocarcinomas NOS reduced insignificantly from 96.03% of the total cases in 2003 to 95.20% of the total in 2020. The highest incidence rate was noted in 2005 and the lowest in 2020. The lowest decrease in incidence rate was between 2019 and 2020 with a 17.85% drop (p < 0.0001) (Tables I–III). The decreasing trend is reliable over the indicated time frame (R2 = 0.66; p < 0.0001). This trend was similar to that of the total incidence rate of gastric cancer in Ukraine from 2003 to 2020 (Figure 1).
The collective incidence rate of all the gastric cancer types, other than adenocarcinoma NOS, was not higher than 0.55 and not lower than 0.34 in 2019 and 2017, respectively. The incidence rates of these types were largely stable without notable variability (Table III).
In the period 2003–2014, the second most common type of gastric cancer diagnosed in Ukraine, after adenocarcinoma NOS, was adenocarcinoma scirrhous (Tables I, II). However, it became the seventh most common type in 2015–2020 (Table III). It decreased from 1.5% of the total number of cases in 2003 to 0.47% of the total in 2020 (p < 0.0001). The lowest percentage of this type of gastric cancer was noted in 2018, when it constituted 0.27% of the total number of cases. The difference between the highest and lowest incidence rate for this type of gastric cancer was 6.33-fold (p < 0.0001) (Tables I, III). This tendency to decrease is reliable (R2 = 0.84; p < 0.0001).
During the time frame 2003–2008, the third most common type of gastric cancer was solid adenocarcinoma, and the fourth most common type was diffuse type adenocarcinoma (Table I). The incidence of rate of solid adenocarcinoma was stable over the period and showed minor fluctuations. In 2009–2020 it became the fourth most common form of gastric cancer, and diffuse type adenocarcinoma became the third most common. This indicated that the incidence rate of diffuse type adenocarcinoma grew insignificantly over this period (Tables II, III).
The incidence rate of adenocarcinoma tubular also grew insignificantly from 2003 to 2020, and it reached its maximum in 2019 (Tables I–III).
The part of intestinal type adenocarcinoma of the total number of cases increased over 18 times by 2020 from the minimum 0.03% seen in 2004 (p < 0.0001) (Tables I–III).
Neuroendocrine tumour (8240) and papillary adenocarcinoma (8260) did not demonstrate significant fluctuation, and their incidence rates remained largely stable from 2003 to 2020 (Tables I–III).
Hepatocellular adenocarcinoma (8170) and linitis plastica (8142) were diagnosed only once each during the 2003–2020 period, in 2005 and 2007, respectively (Table I).
Discussion
In general, the oncologic structure of gastric cancer in Ukraine from 2003 to 2020 resembled that of in the rest of the world at similar timeframes, with adenocarcinoma as the leading form of gastric cancer observed [1, 4, 5].
The other types of gastric cancer that were identified in Ukraine over this time period was not a common diagnosis in other countries. Such diseases are considered to be uncommon forms of gastric cancer [1, 4, 5], and their diagnosis can sometimes be difficult [1, 4]. It requires more advanced identification techniques that should be validated in every diagnostic centre [7]. The European and international healthcare standards for diagnostics and treatment have begun to be consistently implemented in recent decades. One example of consequent improvement in actions is the implementation of methodological recommendations for the pathomorphological departments in Ukrainian hospitals, which leads to continuous updates in the knowledge of how to approach the latest diagnostic tools and methods [8].
An overall decreasing tendency has been observed, especially in recent years. There are several factors that affect this trend [1, 4, 5].
First, there has been an improvement in genetic testing to identify people at risk for familial types of gastric cancer. This opens the possibility for the patients to undergo a gastrectomy. There were several mutations identified in the genes (BRCA2, STK11, ATM, SDHB, PRSS1, MSR1, CTNNA1, and PALB2) that can play a role in gastric cancer pathogenesis [1]. This was proven for patients who were carriers of germline alterations at the CDH1 (E-cadherin) gene [9]. This is most important for populations that are proven to be at a higher risk for the development of familial forms of gastric cancer [1, 9]. It is difficult to conclude whether this is the case for Ukraine. On the one hand, data from the National Cancer Registry of Ukraine has limited capacity regarding the diagnostic and screening tests performed for each case. On the other hand, diagnostic laboratories in Ukraine provide screening tests for genetic variations that are proven to be associated with a higher risk of gastric cancer [10].
Second, the use of proton pump inhibitors (PPIs) is becoming increasingly rational due to the new data on their role in gastric cancer development [11]. The sales of PPIs were seen to increase all over the world, and new medical substances and over-the-counter brands are constantly being introduced. In many countries, monitoring the use of drugs is well established, and healthcare providers are obliged to report all possible adverse drug reactions. The introduction of digital healthcare notes is also helpful to retrospectively identify the role of drugs, as well as other contributing factors, in the development of certain diseases [12]. It has also been demonstrated earlier that the use of PPIs is associated with the risk of gastric cancer, but the causality has not been proven. The propagation mechanism of H. pylori persistent infection by PPIs was proposed [13].
Third, there are practical implementations of the diagnosis and eradication of H. pylori. These methods have been considerably developed over recent years [10, 14]. The mechanisms of persistent infection with H. pylori as well as the mechanisms of carcinogenesis caused by H. pylori were studied. It was shown that H. pylori has several mechanisms to protect itself from the stomach’s aggressive acidic environment. The adhesion properties of H. pylori are medicated by a repertoire of adhesins that the bacterium can turn on and off depending on the environment. Due to a high mutation rate, they can undergo quick adjustments, making H. pylori a unique microorganism in the sense of adaptation [13].
Fourth, a healthier way of life has become more popular all over the world. The trends associated with building a healthy lifestyle include reducing smoking, eating healthier food, controlling weight, and indulging in a higher level of physical activity [1, 5].
Finally, the consumption of widely used drugs is associated with a decrease in the risk of gastric cancer. For example, it has been demonstrated that the COX-2 enzyme plays an important role in the pathogenesis of H. pylori-induced gastric cancer [15]. Statins were shown to be associated with an increased risk of gastric cancer [5]. In experiments, acetylcysteine was shown to protect against H. pylori-associated carcinogenesis [16]. Further studies are required for the drug consumption patterns in the population of Ukraine.
Conclusions
The incidence rate of gastric cancer was seen to decrease over the period 2003–2020. This was mostly due to the decrease of the incidence rate of adenocarcinoma NOS. The epidemiological tendency for gastric cancer to decrease corresponds with international trends of the disease. This tendency can be explained by several factors.