Introduction
Acne vulgaris is one of the most common chronic dermatological conditions [1]. Acne lesions, such as comedones, inflammatory papules, or pustules, typically appear on exposed and visible areas of the body: the face, back, and shoulders [2]. The severity of acne lesions can vary widely, ranging from a few barely noticeable comedones to severe skin lesions in the form of inflammatory nodules and cysts that leave scars and discoloration. This condition can affect individuals of any age but is most common among teenagers and young adults [3]. Skin lesions on the face negatively impact how individuals are perceived by others and diminish their self-esteem [4, 5]. As a result, acne vulgaris significantly affects psychological well-being, and the formation of interpersonal relationships, leading to a decreased quality of life [6–12]. Evidence suggests that greater acceptance of illness-related limitations leads to better adaptation, reduced mental discomfort, lower stress levels, and higher self-esteem [13–15]. In the process of adapting to life with a chronic disease, it is crucial to gradually learn to accept it. By focusing on the emotional and psychological state of patients with acne vulgaris, researchers can gain a deeper understanding of their needs. This can offer greater therapeutic opportunities through the application of targeted psychological support methods, as has been demonstrated in other chronic diseases [16].
Aim
The aim of this study is to investigate the level of acne vulgaris acceptance among young patients and its correlation with disease severity, quality of life, and the feeling of stigmatization.
Material and methods
The study was carried out among university medical students. From 350 screened individuals, 213 were diagnosed with acne and were invited to participate based on specific criteria. Participants needed to be at least 18 years old, have a history of acne lasting at least 1 year, and be proficient in Polish or English. Subjects with serious chronic diseases, other chronic skin conditions or those requiring prolonged therapy, were excluded. Participation was entirely anonymous and voluntary.
A dermatology-trained doctor examined a sample of university students to identify acne vulgaris. After the study’s purpose was explained, demographic and clinical data were collected using a specially designed form, followed by study questionnaires. Informed consent was obtained from all participants. The study received approval from the local Ethics Committee of Wroclaw Medical University (KB-234/2023).
Assessment of acne severity
Clinical acne severity was evaluated using the Global Evaluation Acne (GEA) Scale [17]. This validated instrument categorizes acne patients into a 6-grade scale from 0 to 5 with 0 indicating “no lesions or residual pigmentation and erythema” and 5 indicating very severe acne: “highly inflammatory acne covering the face with the presence of nodules” [17].
Assessment of acceptance of illness
The Acceptance of Illness Scale (AIS), developed by Felton et al. [18] in 1984 and subsequently adapted for Polish conditions by Juczyński [19], comprises eight statements that assess how respondents cope with their illness. These statements explore feelings of being unwanted, invaluable, self-sufficient, and limited by the illness, as well as the ability to enjoy life, perceptions of others’ embarrassment due to their condition, and feelings of dependence or being a burden to family and friends. Respondents assess their current state for each statement on a 5-point scale: 1 point for “strongly agree”, 2 points for “agree”, 3 points for “I don’t know”, 4 points for “disagree” and 5 points for “strongly disagree”. The overall acceptance of illness is measured by the total score, which ranges from 8 to 40 points. Scores below 20 points indicate poor acceptance and adjustment to the illness, as well as significant emotional challenges. Scores between 20 and 30 points reflect moderate acceptance, while scores above 30 points indicate high or complete acceptance.
Quality of life assessments
The quality of life (QoL) in acne patients was assessed using the Dermatology Life Quality Index (DLQI) and the Cardiff Acne Disability Index (CADI). The DLQI, developed by Finlay and Khan [20] and adapted to Polish conditions by Szepietowski et al. [21], measures the impact of skin disease on a participant’s quality of life over the past week. It consists of 10 questions, with responses scored as follows: 0 points for “not at all” and “not relevant”, 1 point for “a little”, 2 points for “very much” and 3 points for “a lot”. The maximum total score is 30 points. Higher scores indicate greater impairment in QoL. The proposed cut-off points for DLQI are as follows: no impairment (0–1 point), mild impairment (2–5 points), moderate impairment (6–10 points), severe impairment (11–20 points), and very severe impairment (21–30 points).
The CADI, developed in 1992 by Motley and Finlay [22] and updated by Abdelrazik et al. [23] in 2021, is a questionnaire designed for teenagers and young adults with acne to measure acne-specific QoL impairment. It consists of five items, each reflecting the impact on QoL over the previous month. Questions 1 and 2 assess psychological and social consequences, question 3 focuses on truncal acne, question 4 addresses the patient’s psychological state, and question 5 asks for the patient’s assessment of their acne severity. Scoring is as follows: 3 points for “very much indeed”, 2 points for “a lot”, 1 point for “a little” and 0 points for “not at all”. The total score ranges from 0 to 15 points, with higher scores indicating greater QoL impairment.
Assessment of stigmatization
The 6-Item Stigmatization Scale (6-ISS) was used to measure the level of stigmatization experienced over the past 2 weeks. Developed by Lu et al. [24] in 2003 and adapted to Polish conditions by Hrehorów et al. [25], this self-report measure consists of six single-choice statements with four possible responses: “not at all” (0 points), “sometimes” (1 point), “very often” (2 points), and “always” (3 points). The total score, ranging from 0 to 18 points, is the sum of the responses, with higher scores indicating a higher level of stigmatization associated with a dermatological disease.
Statistical analysis
The statistical analysis of the obtained results was performed using IBM SPSS Statistics v. 26 (SPSS INC., Chicago, USA) software. All data were assessed for normal distribution with the use of Shapiro-Wilk test. The minimum, maximum, mean, and standard deviation numbers were calculated. Depending on the normality, analysed quantitative variables were evaluated using T-student test for normally distributed data and Mann-Whitney U test for non-normal distribution. Depending on the distribution, Spearman and Pearson tests were used to assess correlations. For the qualitative data, χ2 test was used. For differences between more than 2 groups, ANOVA or Kruskal-Wallis 1-way analysis of variance on ranks were implemented. A 2-sided p-value ≤ 0.05 was considered to be statistically significant.
Results
From the 213 patients invited to participate in the study, 202 completed the questionnaires, resulting in a 94.8% response rate. The sample included 127 (62.9%) females and 75 (37.1%) males. The average age of the participants was 22.7 ±1.6 years, with an age range of 20 to 35 years and a median age of 22 years. Specifically, the average age for females was 22.8 ±1.8 years and for males was 22.5 ±1.2 years. The mean age at the onset of acne for the entire cohort was 13.6 years, with a standard deviation (SD) of 1.9 years. In the gender-specific analysis, females had a mean onset age of 12.9 ±3.5 years, while males had a mean onset age of 13.4 ±2.7 years. Over half of the participants (56.4%) were in informal relationships, while almost the entire remainder were single (39.1%), with only one-fifth (19.8%) of the entire study group stating that they lived alone. The majority of the group were non-smokers (89.6%). Table 1 provides the detailed demographic characteristics of the study group.
Table 1
Group characteristics
Based on the GEA, 91 (45%) of participants were diagnosed with mild acne, 31.7% with minimal acne (almost clear), and 23.3% with moderate acne. No participants were diagnosed with severe or very severe acne. A significant difference in acne severity between genders was observed, with a higher prevalence of mild acne in males compared to females (54.7% vs. 39.4%; p = 0.035) (Table 2).
Table 2
Acne severity among the group of subjects according to the Global Evaluation Acne (GEA) scale
AIS scores ranged from 13 to 40 points, with a mean score of 37.0 ±5.2 points. Notably, a significant gender-based difference in illness acceptance was identified. Males demonstrated a higher mean acceptance level, scoring 37.7 ±4.6 points, compared to females who had a mean score of 36.5 ±5.6 (p = 0.027). Considering the threshold values for AIS scores, it was determined that the majority of respondents (n = 177, 87.6%) exhibited a high level of illness acceptance. A moderate level of acceptance was observed in 10.4% of participants (n = 21), while a small group exhibited low acceptance (2.0%; n = 4) without a significant difference between the genders (Table 3).
Table 3
The level of illness acceptance in the studied group of patients
| Level | Whole group n (%) | Females n (%) | Males n (%) | P-value |
|---|---|---|---|---|
| Low | 4 (2.0) | 2 (2.4) | 1 (1.3) | NS |
| Moderate | 21 (10.4) | 16 (12.6) | 5 (6.7) | |
| High | 177 (87.6) | 108 (85.7) | 69 (92.0) |
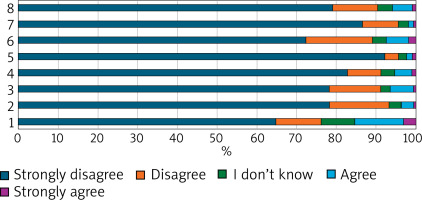
Upon analysing individual statements in the AIS, it became evident that the greatest challenge for respondents was adjusting to the limitations imposed by the disease (statement 1), which had a mean score of 4.24 ±1.20 points. This statement garnered the highest levels of agreement, with 12% of respondents agreeing and 3% strongly agreeing. Following this, the feeling of being invaluable (statement 6) had a mean score of 4.52 ±0.94 points, with 5% agreeing and 2% strongly agreeing. In contrast, being a burden to family and friends (statement 5) and feeling dependent on others (statement 7) received the lowest levels of agreement (2% and 1%, respectively) and the highest average scores (4.84 ±0.62 and 4.80 ±0.60 points, respectively). The remaining aspects of illness acceptance were less critical for our group with acne (Tables 4 and 5, Figure 1).
Table 4
Acne vulgaris acceptance score according to the Acceptance of Illness Scale
Table 5
Percentage of Respondents’ Answers in the Acceptance of Illness Scale
| Answer | S1 | S2 | S3 | S4 | S5 | S6 | S7 | S8 |
|---|---|---|---|---|---|---|---|---|
| Strongly agree | 3% | 0% | 0% | 1% | 1% | 2% | 0% | 1% |
| Agree | 12% | 3% | 6% | 4% | 1% | 5% | 1% | 5% |
| I don’t know | 8% | 3% | 2% | 3% | 2% | 3% | 2% | 3% |
| Disagree | 11% | 15% | 13% | 8% | 3% | 17% | 9% | 11% |
| Strongly disagree | 65% | 80% | 78% | 83% | 92% | 72% | 87% | 78% |
Examining the relationship between acne severity and its acceptance, we found a statistically significant negative correlation (r = –0.277; p < 0.001). Moreover, a statistically significant negative correlation between the AIS score and QoL impairment in acne patients was documented, as measured by both the DLQI and CADI (r = –0.499, p < 0.001, and r = –0.583, p < 0.001, respectively). Additionally AIS scores significantly negatively correlates with the stigmatization level (r = –0.621, p < 0.001).
Discussion
de Ridder et al. [26] conducted a literature review on adaptation to chronic illness, identifying key elements of successful adaptation. According to their findings, there are elements of successful adaptation to chronic illness, and among the models explaining how patients can achieve these outcomes is the cognitive adaptation model, which emphasizes illness acceptance and a sense of control over the illness. Illness acceptance involves effectively managing the unpredictable and negative effects of a chronic condition. Patients employing psychological adjustment strategies have the best chance of successfully adapting to these challenges [27].
Acne vulgaris is a chronic and recurrent skin condition with a significant impact on psychological well-being and quality of life, as demonstrated by numerous studies [13–16]. However, reports describing the degree of acceptance of acne vulgaris are limited [28]. Rolka et al. [28] assessed acne acceptance in 78 adolescents aged 15–17, primarily from rural areas. The mean AIS score in their group was lower than in our patient group, at 24.7 ±2.61 points, indicating moderate illness acceptance. Adolescents in very difficult socio-economic conditions scored 19.7 ±1.43 points, reflecting low acceptance. Although the socio-economic status was not assessed in our group, all participants were young adults studying in one of the largest towns in Poland, Wrocław, and their level of acne acceptance was rather high (37.0 ±5.2 points). The ability to obtain higher education and residing in urban areas are associated with an enhanced socio-economic status [29, 30]. The opportunities provided by larger agglomerations, such as easier access to healthcare, psychological support, and employment opportunities, may enhance the ability to cope with the disease, thereby improving its acceptance.
Similarly to our study, Rolka et al. [28] found a statistically significant difference in acne acceptance based on gender. Boys showed slightly better acceptance than girls (24.3 ±3.1 vs. 22.8 ±3.13 points), a finding confirmed by our study. An investigation conducted in another city in Poland, Poznan, among high school adolescents demonstrated that, despite having a more severe course of the disease, boys were less likely to perceive acne as a significant problem [31]. In published data examining disease acceptance in individuals with psoriasis, its relationship with gender varies. Some studies show a strong correlation with higher acceptance in males [32, 33], while others do not find a connection between these variables [34, 35].
Although extensive literature investigates the relationship between acne severity and its psychological impact [36–39], data exploring this relationship in the context of acne acceptance are scarce. In our study group, which consisted of individuals with very mild to moderate acne, the level of illness acceptance was rather high, and a statistically significant negative correlation was found between acne severity and illness acceptance.
It is easy to hypothesize that the greater the severity of skin lesions, the lower the disease acceptance. Contrary to this, a study using multiple regression analysis found that more severe skin lesions in psoriasis patients were correlated with higher disease acceptance, which was linked to better coping strategies, such as higher levels of optimism and less frequent use of emotion-focused coping strategies [34]. It can therefore be assumed that developing coping strategies for the challenges imposed by the skin disease and the ability to accept them can be very important in improving the mental well-being of dermatological patients. This issue requires further research.
In a study conducted among psoriasis patients in Arabic countries [35], no significant relationship was found between disease severity and disease acceptance. The patients were moderately accepting of their disease (median AIS score of 28), with 25.4%, 35.9%, and 38.76% patients reporting a low, moderate, and high level of illness acceptance, respectively. In this study, similar to our group of patients with acne, one of the most frequently experienced difficulties was adjusting to the limitations imposed by the disease (statement 1). This statement garnered the highest levels of agreement, with 12.9% of respondents agreeing and 31.1% strongly agreeing (compared to 12% and 3%, respectively, in our group). In contrast to our study group, the feeling of being invaluable (statement 6) was the least frequently reported problem, with 20.6% agreeing and 6.7% strongly agreeing. In our group, it was the second most common issue, with 5% agreeing and 2% strongly agreeing. Taking into account the QoL assessed in this study, patients with more impaired QoL showed lower levels of disease acceptance and a greater need for education and support. However, no such correlation was observed in patients for whom psoriasis had a minimal impact on their QoL.
In a study conducted on psoriasis patients in Poland [33], participants demonstrated moderate levels of illness acceptance (mean 24 ±7.56 points), stigmatization (mean 8.7 ±4 points), and moderately impaired QoL (17.8 ±5.9) [33]. No correlation was found between the level of disease acceptance and QoL, but a significant negative correlation with the level of stigmatization was observed.
Participants in our study demonstrated a high level of disease acceptance, a low sense of stigmatization, and mildly deteriorated QoL. This high level of acceptance was significantly associated with lower feelings of stigmatization, as measured by the 6-ISS, and a lower impact on the deterioration of QoL, as measured by DLQI and CADI.
The diagnosis of a chronic illness requires individuals to undertake a variety of tasks essential for both physical and psychological adaptation. This process may involve accepting some degree of functional loss. Additionally, it may necessitate learning new skills and altering daily routines to effectively manage the symptoms of the illness or cope with the demands of treatment [40]. Therapeutic coping methods are the subject of research and indicate that developing emotion regulation and adaptation mechanisms can improve the lives of chronically ill patients [16, 18].
We acknowledge the limitations of our study. Firstly, it was a single-centre study with a selected group of acne patients. Acne affects both younger and older individuals, so it would be interesting to examine differences in acne acceptance across different age groups. Secondly, our cross-sectional study did not include individuals with severe or very severe acne. Therefore, it was challenging to fully assess the impact of acne severity on its acceptance. However, it is important to note that even when evaluating patients with milder forms of acne, we were able to demonstrate a significant correlation between the AIS score and acne severity. The strength of the study was to demonstrate significant relationships between illness acceptance and QoL and stigmatization.