Pulmonary arteriovenous malformation (PAVM) is an abnormal pulmonary artery to vein connection without a capillary bed [1]. The etiology of pulmonary arteriovenous malformations is not fully known. Although they are generally considered to be congenital, they may rarely arise later due to reasons such as trauma, liver cirrhosis, mitral stenosis, and amyloidosis [2]. Hereditary hemorrhagic telangiectasia (HHT), also known as Rendu-Osler-Weber syndrome, is an autosomal dominant disorder characterized by arteriovenous malformations in the skin, mucous membranes, and visceral organs [3]. Only 80–90% of patients with PAVM have an underlying HHT. On the other hand, PAVM occurs in only 30% of HHT cases [2].
Studies have reported that 13% to 55% of patients with PAVM are asymptomatic. Symptomatic patients exhibit dyspnea, hemoptysis, epistaxis, palpitations, chest pain, and cough. On physical examination, murmurs can be auscultated in the PAVM localization. In addition, clubbing, cyanosis, polycythemia or anemia, and telangiectasias may occur [4]. Contrast-enhanced computed tomography is the gold standard method for diagnosing PAVMs and demonstrating their pre-treatment sizes [5]. There are two treatment methods for PAVMs. These are embolization and surgical (lobectomy, segmentectomy, pneumonectomy, or fistulectomy) resection [6].
In our study, a patient who was operated on for pulmonary arteriovenous malformation in the right middle lobe in our clinic in January 2020 is presented in the light of the literature.
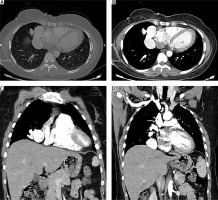
The posteroanterior chest radiograph of a 44-year-old female patient, who had been followed up for rheumatoid arthritis in another center for about ten years, showed a homogeneous density increase in the lower zone of the right lung. The patient’s CT angiography showed an appearance of a lobulated aneurysm, measuring 75 × 25 mm, in the medial part of the middle lobe in the right paracardiac region. It was reported that the arterial supply to the aneurysm was from the middle lobe branch of the right pulmonary artery, and the vein was directly draining into the atrium. A few subhilar cystic lymph nodes and a few mediastinal calcified lymph nodes adjacent to the arteriovenous malformation were visualized (Figure 1).
The patient was evaluated by the Vascular Interventional Radiology department and was not evaluated to be suitable for embolization. Preoperative examinations were performed. Her physical examination and routine laboratory tests were normal. Her echocardiography revealed no pathological finding.
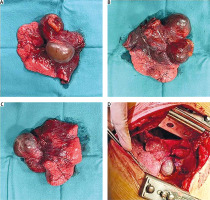
The patient underwent right thoracotomy, and on exploration, a very thin pulsatile mass lesion, 5 × 8 cm in size, was observed in the middle lobe. Enlarged mediastinal lymph nodes, some of which were granulomatous-calcific, were noted. It was observed that the pulmonary artery branch to the middle lobe in the hilum reached a diameter of approximately 1.5 cm. The middle lobe vein was found to drain directly into the left atrium via a venous structure with a diameter of 1 cm adjacent to the inferior pulmonary vein. In the interlobar fissure, a calcified solid lymph node was present between the middle lobe pulmonary artery and the middle lobe bronchus. Right middle lobectomy and mediastinal lymph node dissection were performed on the patient (Figure 2). The postoperative posteroanterior chest radiograph showed no increase in density in the lower right lung. As no problem arose in the follow-up of the patient, she was discharged on postoperative day 5. The patient was referred to the Dermatology and Internal Medicine departments for genetic testing in terms of hereditary hemorrhagic telangiectasia.
The examination of the patient’s pathological specimen of 12.5 × 7.5 × 6.5 cm revealed disorganized vascular structures in cystic structures, measuring 4.5 × 3.5 × 3 cm and 4.5 × 4 × 3.5 cm, and was reported as pulmonary arteriovenous malformation. It was also reported that the subcarinal lymph node was calcified, cystic, and necrotic, while other lymph nodes were reactive. In the postoperative 1-month and 6-month follow-ups, the patient had no clinical or radiological problems.
Embolization and surgical resection are the treatment methods used for PAVMs [6]. Embolization is more advantageous than the surgical technique since it is a less invasive and reproducible technique. Various types of fibrous and non-fibrous coils or amplatzer vascular plugs can be used for embolization. Regardless of the material used, the PAVM is usually localized angiographically and the occlusive material is placed with the help of a catheter.
Surgical treatment is indicated in cases of embolization failure, severe periprocedural bleeding, contrast agent allergy, and when the lesion is not suitable for embolization. In the surgery, the affected part is excised (segment, lobe or hemi-lung). It has the same risk as thoracic surgical procedures. In the postoperative follow-up, recurrence has been shown in 0–12% of the patients treated surgically [7].
There is evidence that untreated PAVMs grow progressively. The morbidity associated with PAVM is around 3% in treated patients and 50% in untreated patients [4]. Treatment of a PAVM is indicated in patients with persistent hypoxemia and for the prevention of neurological sequelae. The vast majority of deaths are due to cerebral complications [7].
In our case, a pulmonary arteriovenous malformation in the right middle lobe was excised by thoracotomy. The absence of postoperative complications and the absence of clinical and radiological evidence of recurrence in the follow-ups show surgical success in pulmonary arteriovenous malformations that are not suitable for embolization.