Introduction
Corrosive substances continue to have an impact on the morbidity of children and adolescents in developing countries, despite the intensive and extensive education programs directed at susceptible groups, legislations controlling the strength and handling of these substances, and preventive measures of labelling and packaging. Upper endoscopy is the cornerstone of the evaluation of the extent of the gastrointestinal injury. Upper endoscopy intervention, including early evaluation, stent insertion, and stricture dilatation, is subject to discussion and debate [1].
The ingestion of caustic substances into the upper gastrointestinal tract in adults is an unusual but potentially life-threatening problem [2, 3]. In contrast to mostly accidental ingestions in children, the ingestion of corrosive solutions in adults is predominantly performed with suicidal intent or due to psychiatric disorders [3, 4].
The severity of tissue lesions caused by corrosive substances depends on the type, quantity, concentration, and contact time. Acids usually cause coagulation necrosis with denaturation of superficial proteins. In contrast, alkaline solutions may lead to liquefactive necrosis and subsequent deep tissue injuries, depending on the exposure time. Prolonged contact with alkaline substances also increases the risk of stricture formation [3, 5].
Endoscopy plays a major role in diagnosing and assessing the severity of caustic injury as well as guiding an appropriate treatment. Recently, computerized tomography (CT) scan of the chest and abdomen has been increasingly used as a complementary tool in the evaluation of caustic injury. Despite advances in emerging technologies and treatments, severe morbidities and even death following the ingestion of caustic agents are evident in clinical practices, suggesting the complexity of this condition [6].
Aim
The aim of the present study was to evaluate the most commonly ingested corrosive substances, and the endoscopic findings, complications, and final outcomes of caustic intake.
Material and methods
This cross-sectional study included 220 inpatient participants with corrosive poisonings during a 3-year period (2017–2019). Corrosive poisoning is a poisoning with strong acids or alkalis capable of causing rapid tissue destruction and shrinkage. Survivors often suffer severe narrowing (strictures) or obstruction of the gullet. Data from the National patient electronic system “My term” and from the “Poisoning information centre” at the University Clinic for Toxicology, Skopje, were used. University Clinic for Toxicology is part of the biggest national tertiary care centre, the Clinical Campus “Mother Teresa” in Skopje, Republic of North Macedonia. Demographic characteristics, type of corrosive substance, endoscopic findings by Kikendall classification, emerging complications, fatal outcome, and hospitalization were analysed. This study was in accordance the ethical protocol for use of electronic data from the national electronic medical system provided to the University Clinic for Toxicology.
The main outcome was based on the endoscopic findings and fatal outcomes. Grading of the gastrointestinal lesions was based on the Kikendall classification: grade I (oedema and erythema of the mucosa), grade IIA (haemorrhage, erosions, blisters, superficial ulcers), grade IIB (circumferential lesions), grade III (deep grey or brownish-black ulcers), and grade IV (perforation). Grades 1 and 2a were defined as low-grade injuries, whereas grades 2b and 3 were defined as high-grade injuries. In all patients, diagnostic oesophagogastroduodenoscopy was done with previous written consent in the first 24–72 h after caustic ingestion, and control oesophagogastroduodenoscopy 15–25 days after ingestion. Patients were divided into 4 groups: 1, acids; 2, alkalis; 3, bleaches; and 4, other household products.
Statistical analysis
The data obtained were analysed with the SPSS software package, version 22.0 for Windows, and are presented in tables and figures. The qualitative series were processed by determining the coefficient of relations, proportions, and rates, and are shown as absolute and relative numbers. Quantitative series were analysed with measures of central tendency as mean, median (Me), interquartile range (IQR), minimum values, and maximum values, as well as by dispersion measures (standard deviation). The Shapiro-Wilk W test was used to determine the normality of frequency distribution of investigated variables. The Pearson χ2 test and Fisher-Freeman-Halton exact test were used to determine the association between certain variables in the groups of subjects. T. The Difference test was used to compare the proportions. The Kruskal-Wallis H test was used to determine if there were statistically significant differences between 2 or more groups of independent variables. The Spearman rank-order correlation coefficient was used to measure the strength and direction of association that existed between 2 variables. A 2-sided analysis with a significance level of p < 0.05 was used to determine the statistical significance.
Results
During the period 2017–2019, out of 220 hospitalized cases with corrosive substance intake, N = 132 (60%) were with ingestion of acids, N = 19 (8.6%) with bases, N = 32 (14.6%) with bleaches, and N = 37 (16.8%) with other household products (p = 0.3469). The number of female patients was significantly higher than that of males: 132 (60%) versus 88 (40%), respectively (Difference test: p = 0.0001). The female/male ratio was 1.16 : 1 in acid poisonings, 1.71 : 1 in bases, 4.3 : 1 in bleaches, and 1.64 : 1 in other poisonings (p = 0.0403).
The mean age of patients was 49.89 ±19.86 years with an age range of 19–94 years, and 50% were younger than 47 years – median (IQR) = 47 (33–64.5). Patients that took acids/bases (Me = 50.5/61 years) were significantly older than those who ingested bleaches/other (Me = 45/35 years) (p = 0.0009).
Upper gastrointestinal endoscopy was rejected by 22 (10%) of the patients, and 22 (10%) were with fatal outcome; most of them 21 (95.4%) took acids. Endoscopy was not significantly associated with the type of the corrosive substance intake (p = 0.7898).
The mean hospital stay was 9.86 ±9.84 days, with diapason of 1/48 days, and in 50% with hospital stay less than 5 days – median IQR = 5 (2–18). Hospitalization was significantly longer in patients who had ingested bases (15.32 ±12.6) and acids (11.5 ±10.1) compared to bleaches (3.6 ±4.3) and other corrosive substances (6.4 ±7.3) (p = 0.0005) (Table I).
Table I
Patient selective features by type of corrosive substance intake
Endoscopy was performed in 176 patients with corrosive substance intake. The most severe endoscopy findings (high-grade injury) were significantly associated with acid and base ingestion in all 3 endoscopy sites (Table II; Figures 1–3).
Table II
Endoscopic findings by type of corrosive substance intake and endoscopic location
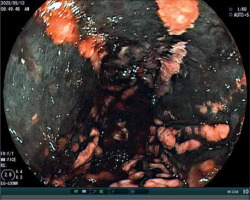
Figure 2
Endoscopic finding of stomach in female after ingestion of hydrochloric acid ingestion (grade III)
We registered 28 (15.9%) oesophageal complications (strictures) – 21 (75%) incomplete and 7 (25%) complete, and 22 (12.5%) stomach complications – 10 (45.5%) incomplete and 12 (54.5%) complete. Out of total strictures, 25 (64.1%) were on one location (either oesophagus or stomach), and 12 (30.8%) were on 2 locations (Figure 4).
Figure 4
Endoscopic finding of pyloric incomplete stricture in female, 21 days after of hydrochloric acid

There was a significant linear positive mild correlation between severity of injury and patient’s age in all 3 endoscopy locations (oesophagus – R(176) = 0.345; p = 0.00001, stomach – R(176) = 0.343; p = 0.00003, and duodenum – R(176) = 0.245; p = 0.0011). No significant correlation was found regarding gender (oesophagus – R(176) = –0.051; p = 0.503, stomach – R(176) = –0.066; p = 0.383, duodenum – R(176) = –0.128; p = 0.091) (Figure 5).
Discussion
Caustic ingestion in adults is a rare but potentially life-threatening problem. Several diagnostic and therapeutic recommendations have been implicated over the last years [3, 7, 8]. Nevertheless, a comparison of acidic and alkaline agent ingestion in adults with regard to clinical management, outcome, and survival has not been performed. Hollenbach et al. retrospectively analysed all adults with caustic ingestion in a tertiary medical centre during the period between 2005 and 2016. They consecutively identified 31 patients (10 with acidic agents and 21 with alkaline agents). Ingestion of alkaline agents was more frequent and revealed higher grades of mucosal injury to the oesophagus and stomach along with a heightened suicidal intent [3].
Our results showed that the most frequent corrosive poisonings were caused by acids (N = 132), and the most common was ingestion of hydrochloric acid (N = 89, 67.4%) followed by ingestion of concentrated acetic acid (N = 13, 9.8%). The most frequently used alkali (N = 19) was sodium hydroxide (N = 11, 57.9%).
The authors of one study found no differences between acid and alkali ingestion in the development of oesophageal strictures. Neither age nor gender could be identified as independent risk factors for oesophageal strictures. In addition, univariate and multivariate analyses failed to show an association of gender, type of ingested agent, or the grade of mucosal injury with mortality in this study, as was demonstrated in our cohort [3].
The study by Hollenbach et al. discussed the possibility that a larger number of patients ingested a greater volume in a suicidal attempt than patients who accidentally took these liquids. So, it can be speculated that the suicidal intent was the reason for more severe mucosal damage in the alkali group, and not the agent [3].
Unfortunately, in our study it was not possible to link accurately the amount of ingested corrosive substance with the grade of corrosive injury, because in many cases it was impossible to provide accurate data on the consumed amount, and some of the patients did not provide data at all.
In a study by Quingking et al., oral burn, abdominal pain, haematemesis, and dysphagia were significantly associated with a high-grade GI injury [9].
In our study almost all patients complained of sore throat and abdominal pain; of the patients with acid and alkali poisoning (N = 151) 87 patients were with haematemesis and 58 patients were with dysphagia. Patients who ingested bleaches and other household products were with less severe clinical symptoms.
The primary reason for ingestion of corrosive substances in the patient population examined by Cheng et al. was suicidal intent (71%) [10].
In our study, 74.7% of patients had suicidal intent and the others were accidental poisonings. Out of all the patients (N = 220), 11.6% were mixed corrosive poisonings with medicines.
The results of one study confirmed Zargar’s endoscopic classification of mucosal injuries post caustic ingestion in relation to clinical outcome. Grade 3b mucosal injury assessed by oesophagogastroduodenoscopy (EGD) was a predictor of prolonged duration of hospital stay, intensive care unit (ICU) admittance, and gastrointestinal (GI) and systematic complications [10].
In our study prolonged duration of hospital stay was significantly longer in patients with base and acid ingestion with endoscopic findings by Kikendall classification grade IIB and III.
Cheng et al. showed that over 80% of patients with grade 3 burns develop stricture formation, while one-third of those with grade 2 develop pyloric stenosis, acid regurgitation, and perforation. This study suggests that patients with mucosal damage exceeding grade 2a are at a higher risk of developing serious complications, while patients with mild mucosal damage have a significantly reduced mortality and morbidity [10]. In a study by Quingking et al., the majority of patients who ingested hydrochloric acid had high-grade injuries [9]. In another study, significantly more high-grade (according to Zargar’s score) lesions in the oesophagus (≥ grade III: 56% vs. 24%, p = 0.01) and in the stomach (≥ grade III: 43% vs. 13%, p = 0.05) were observed in the alkali group. The severity of the mucosal lesions in the duodenum, however, did not differ significantly between both groups (≥ grade III: 6% vs. 0%, p = 0.09). The authors identified only one perforation in index endoscopy in the alkali group. No iatrogenic perforations occurred during endoscopic examinations, although this complication is mentioned in the literature [3, 11, 12]. This finding might be explained by the careful examination with small diameter endoscopes [3].
Our study showed that the most severe endoscopy findings (high-grade injury) were significantly more often associated with acid and base ingestion in all 3 endoscopy locations (p = 0.00001). Out of all the strictures, 25 (64.1%) were on one location (either oesophagus or stomach) and 12 (30.8%) were on 2 locations. Other complications were acute renal failure in patients with ingestion of concentrated acetic acid (N = 7), stomach perforation (N = 9), mediastinitis (N = 3), and hypovolaemic shock (N = 4).
Hollenbach et al. in their study presented that mortality and gastrointestinal complications were higher after ingestion of alkali, but without statistical significance [3].
In this study, of the total of 220 patients, 22 (10%) were with fatal outcome, and most of them (21 (95.45%)) ingested acids; one patient was with alkali poisoning.
Our study has some limitations. Endoscopy was not performed in all patients, because this procedure was rejected by 10% of patients. We also had no insight into the exact cause of death, and we had limited data from autopsy reports. The exact amount of corrosive substance could not be related to the grade of caustic injury. This was the result of inaccurate data regarding corrosive substances, and some patients refused to say the exact amount.
Conclusions
Corrosive substances result in serious injuries to the mucosa of the gastrointestinal tract, which are confirmed by endoscopic findings. The most frequent corrosive poisonings were caused by acids, and the most common was ingestion of hydrochloric acid. Most of the patients with acute corrosive poisonings were with suicidal intent. Hospitalization was significantly longer in poisonings with bases and acids compared to bleaches and other household products. The most severe endoscopy findings (high-grade injury) were significantly more often associated with acid and base ingestion in all 3 endoscopy locations, and they can lead to fatal outcomes as well. Upper gastrointestinal endoscopy is a very important procedure for rapid assessment of the severity of caustic injury, to administer early appropriate therapy, and to identify predictors for overall survival as well as the potential development of strictures. The obtained data are important for the development of a national program in the prevention of corrosive poisoning in our country.













