One method of managing atrial fibrillation (AF) and its complications is left atrial appendage closure (LAAC). The method of choice for LAAC is the LARIAT procedure (SentreHEART, Inc., currently Atricure Inc. Redwood City, CA) – epicardial left atrial appendage (LAA) ligation via intracardiac and epicardial catherization – which was performed in over 4500 cases in the United States over the years 2011–2018 [1]. Over the years, hypotheses about LARIAT related outcomes have been confirmed by a decrease in LAA size after a month [2] and the use of anti-inflammatory drugs to minimize adhesions [3].
Here, we aim to provide additional long-term observational evidence of the validity of the model in terms of a lack of adhesions in the pericardial cavity in patients with AF who have undergone LAAC with LARIAT.
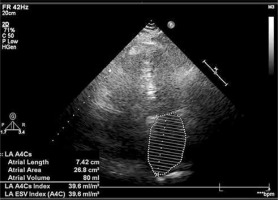
A 75-year-old man with a body mass index of 29.96, a CHA2DS2-VASc of 8 and a short history of severe aortic stenosis (AS) with mild regurgitation (New York Heart Association II/III), permanent AF, after LAAC with LARIAT (in 2014), two pre-LAAC strokes (2001 and 2006), laminectomy of the lumbar spine, transurethral resection of the prostate, hypertension, dyslipidemia and impaired glucose tolerance, was admitted in January 2021 because of dyspnea. Transthoracic echocardiography (TTE) revealed a physiological amount of fluid in the pericardial sac, enlargement of both atria with estimated LA size of 45 mm, right ventricular hypertrophy without signs of pulmonary hypertension, left ventricle (LV) muscle hypertrophy with assessed size of 37 mm and left ventricle ejection fraction up to 60% and severe AS with mild regurgitation with aortic valve area of 0.6–0.7 cm2 and transvalvular mean gradient 42 mmHg. Additionally, mild mitral regurgitation and moderate tricuspid regurgitation were confirmed. The patient was qualified for an isolated aortic valve replacement (AVR) procedure by the Heart Team. In August 2021, the patient was admitted to the Cardiac Surgery Department. A pre-operative follow-up TTE was performed (Figure 1). The procedure was conducted with a complete median sternotomy and standard cardiopulmonary bypass (CPB) technique with ascending aorta and two-stage venous cannulation, epicardial electrode placement, hemodilution, systemic mild hypothermia (32.8°C) and membrane oxygenation, and cold myocardial protection with antegrade crystalloid cardioplegia. There were no adhesions present on the entire surface of the anterior mediastinum and no evidence of any intervention in this region. There were no adhesions in the pericardium. Intraoperative examination revealed the presence of a LARIAT suture that was taut around the LAA and had shrunk and regressed completely after post-procedural necrosis (Figure 2). The aortic valve was replaced with single sutures using a 21 mm SJM MASTERS (Abbott, Abbott Park, IL, USA). After AVR, the patient presented with a postoperative syndrome of low cardiac output, which was resolved by the successful use of inotropic medications. There were no other complications related to the cardiac surgery and the patient was discharged from the hospital within a week after surgery in a stable condition.
Figure 2
A, B – Intraoperative view of the surgery field. Mediastinum was free of iatrogenic adhesions after LAA closure
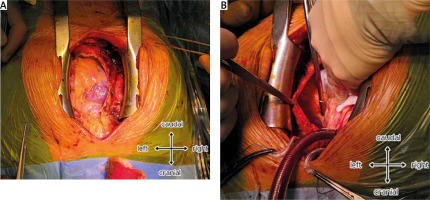
Although 12 years have passed since the first LAAC with a LARIAT device by Bartuś et al. [4], long-term outcome data are limited. The 2018 report by Bartuś et al. [3], which is “the first report of CABG with classic median sternotomy following the LARIAT procedure”, described the expected atrophic changes in the LA 3 years after the procedure, but this time attention was drawn to the absence of intervention traces in the mediastinal region of a patient who had been taking aspirin. Thus we would like to present a case of a patient 7 years after the LARIAT procedure. Considering CHA2DS2-VASc, permanent AF and stroke episodes, the risk of thrombus formation in different parts of the vascular system had to be excluded considering significant morphological changes found in the TTE. Retrograde changes should be given the greatest importance in AS and mild regurgitation. However, it cannot be ruled out that some of the LV and mitral lesions were due to incidental increased LV filling pressure from the LAAC procedure [5]. Notably, the LAA was assessed as present in the TTE, whereas this structure was no longer present. Referral for AVR and prescribing a proper drug regime formed a logical next step. Open surgery was performed without complications, which allowed for accurate assessment of LARIAT outcomes. Potential adhesions might lead to mediastinal compression, a decrease in pericardial cavity volume or an increase in pericardial stiffness. The patient had no iatrogenic marks and the only visible remnant was the suture around the previous LAA, which vanished completely. The fully closed endothelialized orifice and appendage necrosis confirm the successful long-term outcome.
Seven years after LAAC with LARIAT complete LAA closure and LAA atrophy were identified. No visible signs of adhesions in the mediastinal region or inside the pericardium were found. Although this is the first case report of its kind, further descriptions are needed to assess the very long-term effects of LARIAT use in human body structures and functionality.