INTRODUCTION
In recent years, photo-epilation has gained increasing popularity due to achieving permanent hair removal. For this purpose, different types of lasers are used. In 1996, the Food and Drug Administration (FDA) authorized a ruby laser (694 nm) for body epilation. Since then, aesthetic medicine has utilized ruby lasers (694 nm), alexandrite lasers (755 nm), diode lasers (800-810 nm), and neodymium yttrium–aluminum–garnet (Nd:YAG) lasers (1064 nm). A separate group includes lasers operating in a wide range of waves, from 590 to 1200 nm, termed IPL (intense pulsed light). The higher the wavelength, the deeper is the laser penetration [1-3]. Diode lasers, including the Vectus laser by Palomar, require direct skin contact, which provides deeper penetration. Alexandrite lasers and Nd:YAG lasers do not need skin contact; thus, the operation is shallower.
The operation of laser epilation consists of thermal destruction of the hair bulb (thermolysis), preferably in the anagen phase. Because each hair is at a different growth cycle phase (anagen, catagen, telogen), it is necessary to repeat the procedure every few weeks. Successful thermolysis requires the absorption of the laser energy by an appropriate chromophore. Melanin and oxygenated hemoglobin are chromophores in the skin. Due to the depth of the laser penetration, they are calculated at approx. 3-4 mm [2, 4], the melanin of the hair bulb and the skin absorbs more energy than the oxygenated hemoglobin of superficial vessels. Another application of the epilation laser is for vascular lesions, where acting on oxygenated hemoglobin leads to temporary or permanent coagulation of the dermal blood vessels.
Only a few articles describing complications after photo-epilation exist in the literature; therefore, this paper reports a case concerning the damage of the left eye’s structures after photo-epilation of the upper eyebrow in a 28-year-old woman.
CASE REPORT
A 28-year-old female patient in general good health underwent photo-epilation of the left eyebrow ridge performed by a qualified cosmetician. She had not undergone any previous eye procedures, eye pressure was correct, BCVA was 5/5, and no changes were observed in ophthalmological examination in anterior and posterior segments of her eyes. A Palomar Vectus diode laser, with a wavelength of 810 nm, was used for photo-epilation and operated at an energy density of 26 J/cm2 and a pulse frequency of 2 Hz. The apparatus was equipped with a skin cooling down system to the temperature of 5-7°C, preventing its heating over 40-50°C. The duration of the entire procedure was approx. 20 s, and one impulse lasted 10 ms.
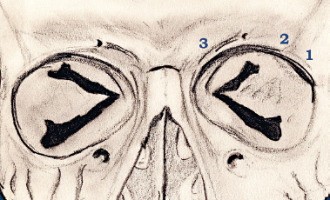
The procedure included completely stretching the eyelid skin over the brow ridge bone and positioning the laser, with internal dimensions of 12 × 12 mm, on the bone, followed by a single laser exposure. The cosmetician began epilation on the temple, in line with the numbering in Figure 1. Metal glasses for eye protection during the laser procedures were placed on the patient’s eyes during the first two applications. Due to the dimensions of the laser, the protective glasses were removed before the third impulse, and the eye was protected with a double layer of cotton pads, which were covered by the patient’s hand, tightly covering the eye. The patient had her eyes closed throughout the procedure. After the third laser application, the patient complained of a stinging sensation in the eye, and she experienced the feeling of mild “pressure” covering the eye. The procedure was stopped immediately, and eye protection was removed. Opening her eyes, the patient could only see a white, blurry image for approx. 5 seconds. The person performing the procedure did not observe any changes in the shape of the pupil. After a while, the shape of the pupil flattened and elongated horizontally. The patient regained correct visual acuity, but there was a sensation of mild restriction in the upper and lower part of the visual field. Even though the procedure was performed only within the left brow ridge, hyperemia of the conjunctivae of both eyes was observed directly following the procedure. A cool compress was placed on the eyes until consulting a doctor. Thirty minutes later, the patient complained of severe headache within the frontal section.
Examination of the eye as an ophthalmologic emergency, 2 hours after the procedure, showed conjunctival hyperemia, no pupil reaction to mydriatics (1% sol. tropicamide, 10% sol. Neo-Synephrine) as well as a change in the shape of the pupil to oval, horizontally. During a thorough ophthalmological examination, no other acuity or intraocular pressure abnormalities were observed, and no diagnosis was made. Anti-inflammatory treatment of steroid eye drops and nonsteroidal anti-inflammatory (NSAID) drops was introduced.
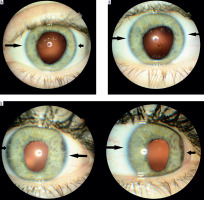
Twelve hours after the laser procedure, the diagnosis was uveitis in the anterior section of the left eye, in the form of minor tyndallization in the anterior chamber and exudative membrane in the pupil as well as posterior synechiae at 8 and 10 o’clock, and 12, 2, and 4 o’clock. The patient complained of intense photophobia and pain in the left eye. Adrenalin was administered subconjunctivally, thus tearing all the synechiae at 1 and 8 o’clock, and Depo-Medrol (methylprednisolone acetal) was administered extraocularly. Moreover, five days following the epilation, transillumination of the iris was observed on the temporal and nasal side (Figure 2), as well as no reaction to pupil-dilating medications from 9 to 2 o’clock.
Figure 2
Seven days following epilation. A) The condition before dilation; B) the condition after dilation. Visible colour deposit on the lens, left after ruptured posterior synechia (white arrow). On the temporal and nasal side the beginning of peripheral part of the iris transillumination, visible as a darker iris (black arrows). No reaction to pupil dilating medications from hour 9 to 2
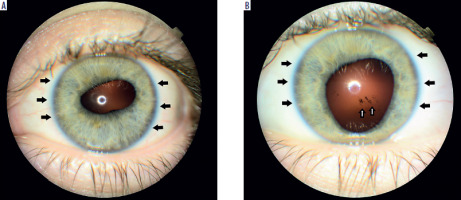
Within two months of the laser procedure, the patient felt a transitional visual disturbance in the form of foggy images and photophobia. The lower section of the iris showed no synechiae, while the upper half still presented some synechiae. The shape of the pupil remained oval horizontally, owing to the increasing iris transillumination as well as lack of pupil reaction to light or pupil dilating or constricting medications (pilocarpine); there was sectional damage to the iris sphincter muscle and iris dilator muscle as well as the nerves of the iris (Figure 3). Moreover, three months after the epilation procedure, there were flashes of light, only in the left eye, lasting for 5 to 20 seconds. The flashes of light appear until today, and they occur particularly at moments of sudden movement (e.g. a sudden tilt of the head) or situations in which the blood pressure rises (e.g. a warm bath, exercises).
Discussion
Although numerous articles have been published concerning laser-related complications in other parts of the body, such as burns to superficial and deep layers of the skin or folliculitis, few articles describe eye complications. One possible explanation is that the lasers are indicated for use on the face while not describing the specific parts of the face. The area of the brow ridge, although beeing part of the face, is difficult to treat due to the upper edge of the orbit, which renders it impossible to position the laser on the skin. Additionally, the square-shaped transducer, with internal side lengths of 12 mm, renders it impossible to position while fully touching the half-round edge of the orbit, resulting in energy being released outside of the application area and being absorbed by the surrounding tissues uncontrollably.
Bell’s phenomenon [1, 5] is the most common mechanism predisposing the eye to damage – it consists of an allied reflex of the eye when closing the eye. The eye positions outwards and upwards, bringing it closer to the epilator. Of note, the skin on the eyelid is the thinnest on the face. The thickness of the skin on the upper eyelid is 0.799 mm, and it is approximately 20% thinner on the nasal side (0.759 mm) compared to the temporal side (1.088 mm). The thickness of the skin in other facial areas ranges from 1.34 mm on the cheek to 2.02 mm in the alae of the lower section of the nose [6]. Considering the depth of laser penetration (3-4 mm) and the fact that women, in whom the skin is thinner than in males, most frequently undergo the procedure, eye protection may prove insufficient, especially if the only barrier is the patient’s fingers or cotton pads. In the eye, the only structure separating the iris from light is the eyelid, which, along with the tarsal plate and the muscular layer, has a thickness of approximately 2-2.5 mm, the next layer being the cornea, which is fully permeable to light. Both Bell’s phenomenon and the fact that the iris contains a large amount of melanin result in the possibility of uncontrolled absorption of laser energy during epilation. The phototoxicity mechanism results in anterior non-granulomatous uveitis, all associated with its clinical features.
In all of the reviewed medical articles, there were cases of a change in the pupil’s shape and displacement of the pupil (corectopia) directly following laser epilation [4]. Moreover, the following have been observed at some point following the procedure: iris atrophy [1, 5], transillumination [1, 5], and uveitis [1, 2, 7]. Every case described included visual disturbance and photophobia after the epilation [1, 2, 4, 5, 7]. Most adverse ophthalmologic incidents were observed using diode lasers with a wavelength of 810 nm [2-4, 8], including the Vectus laser by Palomar. The Vectus laser is a contact laser whose effective operation depends on the degree of application of the tip to the skin, which is impossible at the orbital edge, as described above. A solution to the problem would be the production of transducers with a diameter not exceeding 5 mm, which would enable safe operation within the area around the eyebrow and near the eye.
The general rule that the closer the epilation is to the eye, the more hazardous are the complications, may be adopted. For instance, Herbold et al. [4], as well as Birlakis and Holland [8], described eyelid epilation which resulted in bilateral cataracts, corectopia, and glaucoma.
In the case of eyebrow epilation, the mechanism of complication was almost always related to the temporary removal of eye protection [2, 4, 7, 8], which in turn is a consequence of the inability to reach the hair growing at the edge of the orbit or in the medial canthus near the nasal bridge.
In only one case [1], complications occurred despite the application of protection; however, due to the size of the transducer, it may be assumed that there was an unwanted movement during the procedure or that the eye protection was of insufficient protective quality.
CONCLUSIONS
In summary, over a three-year-long observation, the patient periodically senses intensifying photophobia and moving pigment clumps visible with the naked eye in the mirror. Additionally, she observes flashes of light in the same eye. Ophthalmologic examination revealed increasing iris transillumination and permanent damage to the function of the pupil, observed as the inability to constrict horizontally. More concerning than the permanent change in the shape of the pupil, which may be considered a cosmetic defect, are the possible long-term effects of a diode laser operation, such as previously described by Parver et al. [5], Herbold et al. [4], as well as Birlakis and Holland [8] – early development of cataracts or glaucoma requiring surgery. Disseminating knowledge regarding similar incidents among aesthetic medicine professionals seems advisable so that they may adequately protect the eye. Establishing and propagating knowledge about eye hazards during laser procedures would be logical among professionals (beauticians, cosmeticians, and dermatologists). Applying approved protection shields directly onto the eye or in the eye area will be the next step in bringing the laser procedures to a safer level. It is worth emphasizing that all the cases currently described in the literature on this subject concern women, which may be related to thinner skin and more frequent cosmetic procedures performed among them.

 POLSKI
POLSKI