A 54-year-old patient was admitted to the Hospital Emergency Department with suspected acute ST-segment elevated coronary syndrome. The patient had a medical history of hypertension and obesity and complained of severe chest pain of sudden onset and intensity. The physical examination showed decreased systemic pressure of 80/40 mm Hg and no pulse in the right radial artery. The heart sounded clear, with no pathological murmurs. Following the ECG imaging, which showed ST segment elevation in leads II, III, and aVF – ST-elevation myocardial infarction (STEMI) type (Figure 1 A), myocardial infarction was diagnosed. Prior to admission some antiplatelet drugs were given: acetylsalicylic acid and ticagrelor. During hospitalization, unfractionated heparin was also administered i.v. An urgent coronary angiography from the left radial approach was performed. Using the Judkins Left 3.5 6F diagnostic catheter, the left main coronary artery was catheterized – the morphology of the vessel showed no significant changes (Figure 1 B). There was an unsuccessful attempt to catheterize the right coronary artery opening using Judkins Right 4.0 6F and Amplatz Right 2.0 6F catheters.
Figure 1
A – ECG, B – angiogram of left coronary artery, C – the presence of contrast in the aortic wall, D–F – dilatation of the lumen of the ascending aorta due to dissection, the pseudolumen of the initial segment of the brachial-cephalic trunk is clotted
FL – false lumen, TL – lumen, BCT – brachial-cephalic trunk, Ao – aorta.
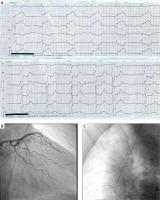
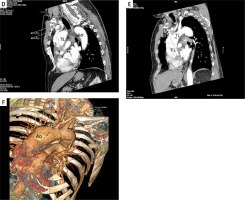
During administration of the contrast agent its persistence within the aorta was observed and regarding this feature the presence of a pseudocanal was suspected (Figure 1 C). Due to the suspicion of an acute aortic dissection, urgent transthoracic echocardiography was also performed. The examination showed an ambiguous image of the aorta without an aortic valve dysfunction and with normal myocardial contractility of 60% ejection fraction. Thus an urgent angio-computed tomography (angio-CT) scan of the aorta was performed, which confirmed an acute aortic Stanford A-type dissection (Figures 1 D–F).
The consulting cardiac surgeon recommended that the patient undergo an urgent surgical procedure. Therefore valve-saving surgery using David’s procedure was performed. After a period of convalescence, the patient was discharged in a good general condition to the Department of Cardiac Rehabilitation for further treatment.
Despite its relatively rare occurrence, it is very important to distinguish between an aortic dissection and acute coronary syndromes. It is very important to remember that despite many clinical similarities, both disease entities must be treated in a different way [1].
Acute aortic dissection should also be distinguished from iatrogenic aortic dissection associated with coronary angiography. Iatrogenic aortic dissections are statistically significantly more common in myocardial infarction and affect the right coronary artery [2].
Echocardiography should be performed in every patient with STEMI in cardiogenic shock, as it may facilitate earlier diagnosis. Delay in surgery and the use of antiplatelet and anticoagulant drug agents may worsen the patient’s prognosis [3].
Withholding dual antiplatelet therapy until the anatomy of coronary lesions is known reduces the risk of bleeding in the event of life-saving cardiac surgery. The characteristics that may ease the diagnosis include the nature of the pain, symptoms of hypotensive shock, pulse deficit, neurological symptoms, diastolic murmur or signs of tamponade. When there is significant doubt, the desire to obtain rapid reperfusion should not hinder further diagnostics. In the case of the present patient, an earlier diagnosis could have been obtained on the basis of the nature of the pain: acute onset, hypotension, or pulse asymmetry with no pulse on the right radial artery. The gold standard is to perform CT angiography of the aorta, and if this test is not possible, to perform transesophageal echocardiography [4].








