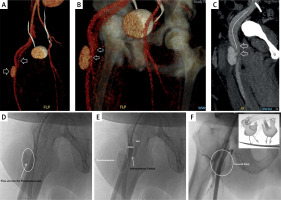
A 47-year-old male patient with known diagnoses of diabetes mellitus, morbid obese, and persistent atrial fibrillation (AF) was admitted to our clinic with a complaint of palpitation. His physical examination and laboratory tests were unremarkable. He underwent radiofrequency ablation for AF under general anesthesia. Two 8F sheaths were placed in the right femoral vein (with 2 separate punctures), and 6F sheaths were placed in the left femoral artery and vein. The procedure was successfully performed and a figure-of-eight suture was performed for right sided venous sheaths just after the ablation procedure. The suture was taken out the day after the procedure. There was no hematoma, but a severe continuous murmur was detected on auscultation of the right inguinal region. Doppler ultrasonography revealed a pseudoaneurysm (48 × 20 × 20 mm) and a low-flow arteriovenous fistula (AVF) below the right femoral artery bifurcation level. The vascular complications persisted after ultrasonography-guided manual compression. Lower extremity computed tomography angiography was performed to delineate the relation of both complications. A pseudoaneurysm with a neck of 4.5 mm and a low-flow AVF were detected at the proximal right superficial femoral artery (Figures 1 A–C). A percutaneous management strategy was planned. Peripheral angiography was performed via left femoral artery puncture and both the pseudoaneurysm and AVF were viewed (Figures 1 D, E). An 8.0 × 26 mm graft-covered stent (LifeStream Balloon Expandable Vascular Covered Stent, BD Interventional, USA) was implanted at the level of the left superficial femoral artery, which covered both complications. No residual contrast filling at the level of the pseudoaneurysm and AVF was observed in follow-up angiography (Figure 1 F). No murmur was detected on auscultation in both inguinal regions the day after the peripheral intervention and he was discharged uneventfully. In recent years, as a result of increasing experience and procedure diversity, femoral intervention has increased and the same number of complications can be observed. In the literature, percutaneous intervention and management of pseudofistula and fistula with graft-covered stent are rarely presented [1, 2]. Our patient was young and could have been treated surgically, but he refused such treatment. In addition, studies have shown that percutaneous treatment strategies are effective and safe in endovascular iatrogenic injuries and may be an alternative to surgical treatment [3]. There are insufficient studies comparing balloon-expandable graft stents with self-expandable stents in the endovascular management of iatrogenic femoral artery pseudoaneurysm and fistula complications. However, in our experience, we chose a balloon expandable graft-covered stent in pseudoaneurysm/fistula closure cases, as there is a need for postdilatation in cases with residual flow after stent implantation and at the same time the radial force is high. Although surgical and endovascular treatment options have improved, the best complication management is to prevent complications from occurring. One of the most important points is that ultrasound-guided intervention in transfemoral approaches has been shown to reduce complications [4].
Figure 1
Lower extremity computed tomography angiography 3D reformatting (A, B) and 2D coronal section (C) and peripheral angiography (D, E) showing both pseudoaneurysm and arteriovenous fistula at the level of the right proximal superficial femoral artery. Arrows indicate the pseudoaneurysm neck and filling of the femoral vein from the superficial femoral artery. Both vascular complications were successfully treated via covered stent implantation (F)