Introduction
The prevalence of umbilical hernias in the adult population of Western countries is as high as 2% [1]. Still the most frequently performed technique is the open anterior approach, mainly due to the possibility of making only a small incision of the skin and the relatively short time of the surgical procedure [2]. However, a higher risk of hernia recurrence may be related to a lack of reinforcement of a defect with a synthetic material. In the case of the smallest umbilical hernias (1–2 cm) this risk is three times higher compared to techniques involving mesh implantation [3]. The risk of recurrence increases with the diameter of the hernia orifice and the body mass index [4]. The group of overweight and obese patients is constantly growing; therefore, these patients will increasingly require umbilical hernia treatment [5]. These patients are also at much higher risk of a diastasis recti, which is a recognized risk factor for midline hernia recurrence [6]. Confirmation of the presence of a recti divarication should prompt the surgeon to reinforce the defect with a synthetic mesh. Moreover, in the group of overweight and obese people, an increased incidence of complications is observed, mainly surgical site infections (SSI) [7]. This risk also increases in the case of an anterior approach with use of a mesh [8]. Hence, laparoscopic hernia repair may be used to reduce the risk of infection, while preventing recurrence. Currently, the most popular technique is still a laparoscopic intraperitoneal onlay mesh placement (IPOM), but this procedure has some limitations. The main drawback of the use of IPOM is the possible development of intraperitoneal adhesions, poor integration of some meshes into the abdominal wall, and pain associated with mesh fixation [9]. An alternative solution is a laparoendoscopic mesh placement in the retromuscular space (enhanced totally extraperitoneal Rives Stoppa repair – eTEP-RS) [10]. It is a recently developed technique of ventral and incisional hernia repairs, gaining recognition and interest among surgeons worldwide [9]. However, in this method, it is necessary to sacrifice the posterior lamina of the rectus abdominis sheath, which must be transected on both sides to obtain a large retromuscular space [11]. This concomitant collateral damage may have some impact on the future stability of the trunk, so in the case of small and medium-sized umbilical hernias, the use of eTEP-RS may be controversial [12]. According to the European Hernia Society (EHS) classification of abdominal hernias, a defect between 2 and 4 cm is defined as a medium-size hernia [13]. Contradictory indications and contraindications to the use of various surgical access techniques and synthetic materials may be reconciled by one of the newest umbilical hernia repair techniques. The transfer of the transabdominal preperitoneal repair (TAPP) concept from the inguinal region to the periumbilical area allowed for the development of a laparoscopic umbilical TAPP technique [11]. This technique benefits from laparoscopic minimally invasive access, the benefits of hernia orifice closure as in the IPOM plus method, and posterior enhancement of the abdominal wall defect, but without the use of the retromuscular or intraperitoneal space, and easy placement of a large mesh despite the relatively narrow hernia orifice [14]. However, the lack of popularization of this technique so far may be related to the poor ergonomics of this procedure, the need to suture both the defect of the abdominal wall and the peritoneum “on the ceiling”, and an extended operation time, especially compared to other available open techniques.
Aim
Currently, there are scarce studies in the literature analyzing the use of transabdominal preperitoneal mesh repair of umbilical hernias, especially in the group of overweight and obese patients; therefore in this study we aimed to compare the feasibility, safety and efficacy of the umbilical TAPP technique (u-TAPP) with the commonly used ventral patch repair (VPR) technique.
Material and methods
Patients
The retrospective cohort analysis included patients undergoing elective surgery for primary umbilical hernia. Only patients operated on using the TAPP laparoscopic method and the open ventral patch were included. Patients with body mass index below (BMI) 25 kg/m2 were excluded. Patients with hernia strangulation or incarceration were excluded. Patients who had previously undergone umbilical hernia repair were not included in the study. Patients who underwent other abdominal interventions after umbilical hernia surgery were not eligible. Patients who did not agree to participate in the study or were lost to follow-up (no contact, etc.) were excluded. Only operations in patients with a hernia orifice diameter of 2 to 4 cm were analyzed.
All patients operated on between January 1, 2020 and May 31, 2021 were taken into account. The follow-up period was set at 1 month after the surgery. During the analyzed period, the function of the surgery department was suspended three times (for a total of 6 months) due to the COVID-19 pandemic and subsequent waves of disease, which in some way has influenced the total number of procedures.
Qualification for the study
All patients operated on in this period by one surgeon with the greatest experience in laparoscopic operations in the team were qualified for the TAPP laparoscopic surgery (u-TAPP). The remaining surgeons in the department performed VPR in the analyzed period. All patients gave informed consent for the procedure according to the protocol of the National Surgical Society. All patients included in the analysis agreed to participate in the study.
Procedure
All operations were performed under general anesthesia. Thirty minutes before the operation, each patient received antibiotic prophylaxis. Each patient received thromboprophylaxis 12 h before surgery, in accordance with the applicable standard. No drains were used during the operation. After the operation, an oily dressing was placed in the hollow of the reconstructed umbilicus skin with the addition of lanolin and paraffin, and a tamponade of the umbilicus was performed from the outside to maintain its concave shape. The use of abdominal binders was not routinely recommended.
Umbilical TAPP
The patient is lying on his back with no torso flexion. After a pneumoperitoneum of 12 mm Hg is obtained with a Veress needle inserted at Palmer’s point, the operating table is tilted to the right about 30° and three trocars are inserted in the anterior axillary line on the left side of the patient. The first 10 mm optical trocar is inserted at the umbilicus level, and the next two 5 mm, about 4–5 cm in cephalic and caudal directions from the first. The assistant and the operator stand on the left side of the patient, the same as in an IPOM procedure, and the monitor is positioned on the opposite side. After releasing any adhesions with the hernia ring, the surgeon marks the incision line of the peritoneum with electrocautery at a distance of 7–8 cm from the linea alba to the left, parallel to the midline (Photo 1 A). Then a thin lamina of the peritoneum is grasped, and the peritoneum is incised, paying attention to sparing the posterior lamina of the rectus abdominis sheath. The peritoneum is transected longitudinally over a length of about 12–15 cm, and a peritoneal flap is gradually dissected towards the linea alba. Dissection is easier at this stage due to the appearance of fatty tissue beneath the peritoneum. After reaching the linea alba, the separation of the peritoneum also continues on the contralateral right side, below and above the level of the umbilicus. At this stage, it is important to leave the hernia sac in place. Only after the peritoneal flap has been dissected nearly completely around the hernia orifice (about 270°) is the peritoneum leading to the hernia clearly visualized (‘volcano sign’) (Photo 1 C). Then the hernia sac is completely reduced, avoiding thermal damage to the skin covering the hernia sac. After dissecting the hernia orifice, dissection of the peritoneal flap on the right side needs to be completed, approximately 7–8 cm from the linea alba. Then the hernia orifice is sutured transversely laparoscopically with a continuous non-absorbable self-locking suture (V-loc 0, Medtronic) (Photo 1 G). A self-anchoring mesh (ProGrip; Medtronic) is inserted and placed evenly around the hernia defect. A primary peritoneal incision is sutured with a continuous absorbable suture (Photo 1 I). The operation ends with desufflation of the preperitoneal space and then the peritoneal cavity. There were no sutures placed in trocar sites. A video presenting the details of this technique is available at the #Herniacademia channel in YouTube (https://youtu.be/AbR5YTJJkBA).
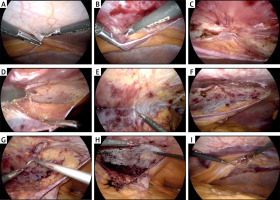
Photo 1
Laparoscopic umbilical TAPP procedure. A – Incision of proximal peritoneum on the left side of the patient approx. 7 cm away from the linea alba. B – Dissection of proximal peritoneal flap. C – Volcano sign. D – Dissection of fatty tissue beneath intact linea alba. E – Dissection of distal peritoneal flap up to 7 cm away from the linea alba. F – Complete development of preperitoneal pocket for mesh insertion. G – Closure of hernia defect (non-absorbable suture). H – Mesh placement. I – Complete peritoneal closure
Ventral patch
An arcuate incision is made at the lower edge of the umbilicus approximately 3–4 cm long. After dissection of the hernial sac, separation of possible preperitoneal lipomas, the sac is opened, the contents checked, and the excess sac cut off. After the hernia defect is visualized, the inner surface of the peritoneum is inspected for any adhesions. Adhesions surrounding the defect are removed. If enlarged fatty folds (thick falciform or umbilical ligaments) are found, they are separated from the linea alba approximately 4 cm away from the hernia defect. The ventral patch, folded in half, is then inserted into the peritoneum and placed inside the peritoneal cavity, keeping its circular shape around the hernia orifice. The size of the mesh used depends on the size of the hernia defect and the possibility of a flat placement of the mesh in the peritoneum. Ready-made meshes with a size of 6.3 or 8.3 cm are used (Parietene Ventral Patch, Medtronic). On the side of the intestines, the mesh is coated with an anti-adhesive layer, which allows direct contact with the intestines. The mesh is equipped with two rigid semicircular rings that facilitate its unfolding and positioning. The four mesh poles are then attached to the fascia around the hernia defect with a single non-absorbable suture (Optilene 0; B.Braun). The hernia ring is then sutured with a continuous suture with prolonged absorption (MonoMax 0; B.Braun). A video presenting the details of ventral patch technique is available at the #Herniacademia channel in YouTube (https://youtu.be/TFP7mxQxD8M).
Outcomes
Among the patients, demographic data and medical history information (gender, BMI, smoking, diabetes, hypertension, immunosuppression) were collected. Data from operating protocols and the course of hospitalization were analyzed (diameter of the hernia gates, area of the implanted mesh, duration of the operation, hospitalization time, number of peritoneal defects during a laparoscopic procedure, pain on the first day after surgery, presence of early complications). Thirty days after discharge, all patients operated on provided information on the results of treatment via a telephone questionnaire. The primary outcome of treatment was the presence of a recurrence. Patients who suspected a recurrence or felt a thickening in the wound were additionally subjected to physical examination by a doctor and sonographic examination. Additionally, the presence of pain was assessed as secondary treatment outcome, using a numerical scale (NRS; no pain 0, pain maximum 10). Additionally, the return to daily activity was assessed (0 – no activity limitations, 10 – full activity limitation), cosmetic effect (0 – very favorable appearance of the navel, 10 – completely unfavorable appearance of the umbilicus) and satisfaction with the treatment (0 – full satisfaction, 10 – complete dissatisfaction).
Statistical analysis
Continuous numerical data are expressed as mean ± standard deviation (SD) and range. Data were analyzed using Statistica 11.0 (StatSoft). Continuous values were analyzed with the t test, and categorized values with the Pearson χ2 test. P-values < 0.05 were considered statistically significant.
Results
The study included 45 patients who met the inclusion criteria, 40 men and 5 women. Two patients were lost to follow-up. Eventually, 43 patients were included in the case-control study, 22 in the VPR group (control group) and 21 in the u-TAPP group (case group). The groups were comparable with respect to age, BMI, and recurrence risk factors, with no statistically significant differences (Table I).
Table I
Demographic and surgery variables
There were no differences between the groups in the size of the hernia defect. The mean width of the orifice was 26 mm in the VPR group and 30 mm in the u-TAPP group (p = 0.185).
In the u-TAPP group, there was no need to convert to the open method. There were no intraoperative complications in the u-TAPP group, although minor peritoneal lesions were not classified as complications because they were sutured during surgery.
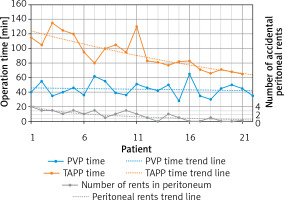
The operation time was significantly shorter (p < 0.001) in the VPR group (43.1 ±11.6 min) than in the u-TAPP group (93.2 ±22.3 min) (Figure 1). However, in the VPR group it was possible to place a much smaller area of the synthetic mesh than in the u-TAPP group (34.3 vs. 164.2 cm2; p < 0.001) (Table I).
Figure 1
Operation time evolution for PVP and TAPP groups with number of accidental peritoneal rents during TAPP procedure
There were no differences in the length of hospitalization and all patients from both groups were discharged on the first postoperative day. There were no re-admissions to the hospital within 30 days of surgery or reoperation among the analyzed patients.
In postoperative complications, one subcutaneous hematoma was found in the umbilical area after TAPP surgery, which resolved after aspiration and evacuation. In the VPR group, one mild superficial thermal burn of the skin was found, which was healed with hydrofiber dressings.
During the follow-up period, there was no recurrence in either group. In the VPR group, 4 patients reported a palpable tumor under the skin of the umbilicus, but no recurrence was confirmed on physical examination (simple soft tissue swelling was found). With regard to pain, no significant differences were observed between the two groups, on either the first or the thirtieth postoperative days (Table II). Both in VPR and u-TAPP groups there was a full return to daily activities after a month (2.2 vs. 1.9; p = 0.129). In the VPR group, patients reported a better cosmetic effect compared to the u-TAPP group (3.8 vs. 2.2; p < 0.05), and among the unfavorable phenomena in the wound, they mainly mentioned the persistent swelling of the umbilical area. In the VPR and u-TAPP groups, patients reported a high degree of satisfaction with the treatment received (1.3 vs. 1.4; p = 0.283).
Table II
Surgical outcomes
[i] PVP – parietene ventral patch. Pain is measured using visual analogical scale from 0 (no pain) to 10 (worst pain imaginable). Activity restriction is graded using a scale of 0 (no restriction) to 10 (completely restricted from daily activities). Cosmesis results (shape of the abdomen and at the site of the hernia) were measured from 0 (very beautiful) to 10 (extremely ugly). Satisfaction with treatments results were measured from 0 (full satisfaction) to 10 (no satisfaction). Data are expressed as mean and standard deviation.
Discussion
Anterior approach umbilical hernia repairs in obese patients are associated with dissection in a relatively deep surgical field due to a thick layer of subcutaneous adipose tissue. Improvement in ergonomics and visibility may occur after the skin incision is widened and the fascia is exposed over a larger area. However, it is associated with an increasing risk of a surgical site infection [2, 7, 15]. At the same time, lack of good visibility does not allow for adequate dissection of the space for placement of a flat mesh. Hence, one solution in this group of patients was to introduce some ready-made products that allow for easy mesh deployment after inserting it into the operating field. In the case of the VPR used in the analysis, a mesh diameter of 6.3 or 8.3 cm is usually used. This size is usually sufficient to treat small hernias (less than 2 cm), but for hernias with defect diameter of 2 to 4 cm, it may not provide a sufficient mesh overlap. Currently, the dogma that the margin of the mesh beyond the hernia defect should be at least 5 cm is increasingly being abandoned [15]. Currently, it is recommended that the mesh surface area needs to be at least 16 times larger than the defect area, which for the circular umbilical hernias usually means the use of a mesh four times larger than the diameter of the defect [16]. For a hernia of 3 cm, the width of the mesh should be at least 12 cm. This is much larger than the augmentation area guaranteed by the ventral patch. However, in the u-TAPP procedure, the required area of an adequate reinforcement with a synthetic implant was obtained in each case. Dissection in the preperitoneal space allows a free choice of the size of the prepared space for the size of the mesh, which is derived from the diameter of the hernia defect. In our material, the dissected space was usually slightly larger than the mesh size, which allowed for easy implant placement and facilitated closure of the peritoneum at the end of the operation.
TAPP umbilical surgery now commonly involves the use of surgical robots that make this procedure much easier. First, they allow for very good visualization of all prepared layers while maintaining continuous hemostasis, minimizing hand tremors and excessive movements, prevent damage to the thin peritoneal lamina, and after preparing the appropriate space they allow for quick, reliable, and convenient closure of the hernia and peritoneal defects [17]. For these reasons, many surgeons believe that this is an operation that should only be performed in centers equipped with robotic systems [18]. However, the numerous advantages associated with the possibility of minimally invasive placement of the large mesh outside the peritoneal cavity without damaging the structures ensuring the strength of the abdominal wall have attracted interest in this method also among surgeons having only laparoscopic facilities at their disposal. Based on our preliminary experience, we can conclude that this is a laparoscopic operation, its course is logical, and the assumptions are simple, giving the surgeon great satisfaction, due to the possibility of placing a large mesh in a space that has not been commonly used in umbilical hernia repairs so far. It should be emphasized, however, that this is a technically difficult method. The main difficulty stems from the necessity to dissect a very thin layer of the peritoneum, which covers the posterior surface of both posterior rectus sheaths from the rear. In this area, the peritoneum adheres tightly to the sheath, it is delicate and fragile, and just grasping it with an instrument at an acute angle may cause a tear, which in turn will make it difficult to suture it tightly later. Dissection is painstaking, gentle, with very subtle blunt movements, with minimal use of electrocautery. Despite the necessity to make many small movements with laparoscopic instruments, a large space for the mesh is obtained quite quickly. In the medial area, the peritoneum is separated from the linea alba by a layer of adipose tissue; hence dissection in this area is easier, but the hernia sac must be dissected.
Technical difficulties in the dissection of the space are confirmed by the frequency of peritoneal lesions. In our material a total of 2.7 peritoneal lesions with an average defect diameter of 9 mm were observed during the first 10 procedures, while in the next 10 procedures, 0.6 defects with an average size of 4 mm were observed. This may prove that the surgeon quickly acquires experience in this method, while moving in a narrow operating field, with a growing ability to recognize appropriate layers for preparation.
In the case of the ventral patch method, the main disadvantage is the lack of full control of the position of the mesh intraperitoneally after the hernia defect is closed. In this situation, it is possible for the edge of the mesh to fold up or even fold in half. This can expose an uncoated area of the mesh, which promotes the formation of peritoneal adhesions and may lead to recurrence [9, 14]. Additionally, in the case of a ventral patch, there may be no flat placement of the mesh in the presence of a significantly fat sickle or umbilical ligament.
Another aspect confirming the technical difficulty of the TAPP umbilical operation is the duration of the procedure. In our material it was twice as long as the ventral patch operation. However, it should be noted that the ventral patch operation has been performed for many years in our center, and the experience of surgeons in this method is extensive. However, in the case of umbilical TAPP, we present preliminary results from the first procedures of that kind performed in our center. It is worth noting, however, that the operating time of the last ten procedures was over one-third shorter than that of the first 10 procedures (106 vs. 74 min), which also confirms the acquisition of experience in the course of the learning curve. We assume that an average learning curve for experienced surgeons might be similar to another laparoscopic advanced technique, i.e. TEP, as similar dissection between anatomical planes are needed for both methods [19]. The main stages of the operation affecting such a long procedure time are the dissection of the preperitoneal space and the hernial sac itself. Along with the growing experience, the duration of the stage of dissecting and suturing the defect was shortened mainly. However, the extended operation time compared to the ventral patch method did not extend the hospitalization time. We found no statistically significant differences with regard to hospitalization time; all patients from both groups were discharged from the hospital on the first postoperative day. There were also no differences in postoperative pain on the day of surgery, on discharge, and at 30 days postoperatively. We found no early recurrences in either group 1 month after surgery. Therefore, the question arises whether it is worth resorting to the more difficult, longer lasting and ergonomically inferior umbilical TAPP procedure, since the easy, fast and convenient ventral patch method is available. In our subjective opinion, the u-TAPP method gives a sense of a certain, permanent repair without the risk of intraperitoneal reactions between the synthetic material and the intestines. Especially in the case of obese patients, in whom it is difficult to predict the further development of obesity, the u-TAPP method allows the hernia defect to be protected with a larger sheet of flat mesh with reinforcement of the linea alba. Perhaps the long-term results of treatment, several years after the repair was performed, will indicate which of these methods will be more effective in preventing recurrences.
Improved ergonomics of the umbilical TAPP operation can be achieved with a few simple steps. First of all, the operating table should be tilted about 30° to the opposite side. For this purpose, it is necessary to place an additional rigid support on the patient’s right side with a shock-absorbing foam pad next to the patient’s hip. Additionally, the patient’s left adducted hand should be tilted in the cephalic direction, which will allow for more space for the surgeon and assistant. One should avoid placing the left hand along the torso as this may sometimes interfere with instrument movement when dissecting the proximal peritoneal flap. To avoid uncomfortable bending of the surgeon’s wrists during surgery, it is necessary to raise the table height above the level of the surgeon’s elbows. Port triangulation and the use of 30-degree optics complete the list of actions that allow for relatively comfortable performance of the procedure. An additional aspect that should be considered is the appropriate selection of synthetic materials. It is difficult to tighten stiff, fibrotic, and tense scarred edges of the hernia with an ordinary monofilament suture. The use of self-locking threads allows for a closer approximation of the hernia ring using the shoe-lacing technique, where successive loops are gradually tightened, allowing for even distribution of tension. In addition, the use of a self-anchoring mesh allows additional fixation with sutures to be avoided. However, in the case of using self-anchoring meshes, it is worth paying attention to the use of products that allow them to be easily distributed in a tight space; hence we found it much easier with the use of coated meshes.
We did not close the 10 mm port site in the present group of patients. The trocar site is located as laterally as possible and penetrates through the lateral muscles in an oblique direction; thus the risk of port site hernia is minimized compared to midline sites, while full closure might be troublesome as long as we do not use dedicated devices for the closure of trocar sites. However, this issue should always be considered, especially in obese patients.
The weaknesses of this analysis include the small size of the study groups. However, the authors wanted to present the preliminary results of treating the first group of patients with a new surgical technique. All currently operated patients are still undergoing analysis, and further treatment results are to be presented in the future. Another weak point is the short follow-up time after surgery in terms of risk of recurrence. However, the main aim of the study was to assess the possibility of routine use of an umbilical TAPP technique in comparison to a standard technique. The authors wanted to ascertain whether ergonomics, operation time and technical conditions related to the use of laparoscopy, with the simultaneous lack of a surgical robot, allow introduction of this method into everyday practice. However, it seems that the short time of recurrence observation is less important in the case of umbilical TAPP than in the case of a ventral patch due to the introduction of a larger mesh size in each operation with simultaneous confirmation of its correct position.
Undoubtedly, the umbilical TAPP technique is an interesting alternative to the currently used methods. This technique would be especially beneficial for obese patients. Along with increasing experience with this technique, we have noticed that in this group of patients the dissection is even more feasible mainly due to thicker adipose tissue in the preperitoneal plane. However, in our opinion it is a good technique for surgeons who are experienced in laparoscopic inguinal hernia surgery, where dissection of the peritoneum is still easier. It seems that the previous experience with the IPOM method also allows for faster implementation of the umbilical TAPP technique into one’s armamentarium due to the similar layout of ports and similar operating field. In this analysis we wanted to emphasize that widespread use of this technique would probably be impossible; however, this technique is still very useful in the hands of experienced laparoscopic surgeons, and additional analysis is needed. It seems that this technique should be especially recommended for surgeons who plan to introduce the eTEP-RS method into their armamentarium for abdominal hernia surgery in the future, because many stages of the operations are common.
Conclusions
The TAPP technique in umbilical hernia repair allows for placement of a much larger mesh than in the case of anterior approach surgery, and is closer to the current recommendations, especially for patients with additional risk factors, such as obesity or the coexistence of diastasis recti. The TAPP method allows the mesh to be introduced into the preperitoneal space, which avoids direct contact of the mesh with the intestines. The laparoscopic method of umbilical TAPP is feasible and safe, but the operation time is longer compared to open methods.








