Very elderly patients with advanced coronary artery disease are at high risk of complications and poor prognosis [1]. Given their multimorbidity and coexisting frailty syndrome, these patients are often not candidates for surgical treatment. Age has been shown to be associated with the amount of coronary artery calcification [2], which can lead to poorer prognosis and an increase in-stent failure due to the risk of stent underexpansion [3]. Novel techniques of calcified plaque modification, such as orbital atherectomy, reduce the volume of calcified plaque and increase the vulnerability of the plaque to predilatation with balloon catheters [4]. Despite good initial safety data, results of left main (LM) treatment with orbital atherectomy and the elderly patient remain scarce [5]. The clinical case we present here confirms the safety of orbital atherectomy in patients with frailty syndrome.
An 82-year-old woman with a history of ischaemic heart disease underwent percutaneous coronary intervention (PCI) of the left anterior descending artery (LAD) with 2 drug-eluting stents (DES) in 2010, complicated by vessel perforation and the need for stent grafting. The patient also had a medical history of hypertension, hyperlipidaemia, asthma bronchiale, pemphigoid, depressive disorder, right hip replacement, L4/L5 spinal surgery, and frailty syndrome (Edmonton Frail Scale – 11 points; Clinical Frailty Scale – 6). The patient was admitted to the cardiology department with symptoms of unstable angina. On admission, the electrocardiography showed sinus rhythm and negative T waves in the aVL and I leads. Echocardiography showed hypokinesis of the apical segment of the anterior wall with an ejection fraction of 50%. Coronary angiography showed a significant, highly calcified stenosis in the distal LM extending to the LAD ostium (60% stenosis) and circumflex artery (Cx) (80% stenosis); previously implanted LAD stents were without restenosis (Figures 1 A, B). The right coronary artery (RCA) was significantly stenosed proximally and distally with aneurysmal dilatation in the medial segment. The calculated SYNTAX score was 18 points. Due to the patient’s frailty, she was eligible for staged PCI. RCA angioplasty was performed via radial access in the first stage using a 6.5F sheathless catheter. The lesions were predilated with a non-compliant (NC) Emerge 2.75 catheter, a DES Resolute 3.0 × 15 mm coronary stent was implanted in the distal stenosis, and a DES Resolute Onyx 3.5 × 18 mm coronary stent was implanted in the proximal stenosis. An NC Pipit 4.0 × 8 mm catheter was used for post-dilatation. In the next deferred stage, LM/LAD/Cx angioplasty was performed via a 7F right femoral access using orbital atherectomy. Four low and high speed (80,000 and 120,000 rpm) burr passes were performed from the LAD/LM (Figure 1 C) and four passes from the Cx/LM (Figure 1 D), followed by predilatation with a 3.5 ×15 mm NC catheter. The two-stent double-kissing (DK) Culotte technique was used to treat the LM/LAD/Cx bifurcation: a Resolute Onyx 4.0 × 30 mm to LM/LAD and a Resolute Onyx 4.0 × 15 mm to LM/Cx were implanted. The first and second KB were performed with NC 3.5 balloon catheters and the final POT with an NC 5.5 × 8 mm catheter (20 atm) (Figure 1 E). Final optical coherence tomography (OCT) evaluation showed full stent expansion, good stent apposition and visible modified calcified plaque (Figure 1 F). The hospital stay was complicated by a drop in haemoglobin levels (4 g/dl) requiring a transfusion of 2 units of blood with no overt bleeding and mildly symptomatic SARS-CoV-2 infection. The patient was discharged home after 14 days of hospital stay on a dual antiplatelet therapy regimen consisting of aspirin 75 mg/day and clopidogrel 75 mg/day (de-escalation from ticagrelor). The 8-month follow-up period was uneventful.
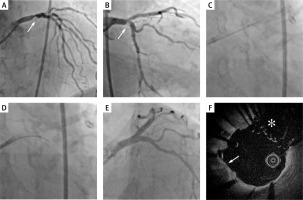
Figure 1
A, B – Initial left coronary artery angiogram. The white arrow indicates calcified lesion. C – Orbital atherectomy burr passage from LAD towards LM. D – Orbital atherectomy burr passage from Cx towards LM. E – Final result of LM/LAD/Cx bifurcation stenting with DK-Culotte technique. F – Final OCT run. The white arrow indicates calcified plaque. The white star indicates the place of the neo-carina