Summary
Satisfactory long-term results characterize surgical revascularization in the off-pump technique (OPCAB). Our study showed similar long-term survival in patients with left main and multivessel coronary artery disease treated with OPCAB. The female sex and diabetes mellitus were found as possible risk factors for 10-year mortality risk in multivariable analysis.
Introduction
Left main (LM) coronary disease is believed to represent a complex, advanced, and potentially life-threatening atherosclerotic syndrome as the artery supplies over 75% of left ventricular myocardium. Isolated LM stenosis occurs only in 5% of patients [1] and this location requires nonelective intervention in up to 60% of patients [2].
Surgical intervention was shown to improve survival in clinically significant unprotected left main coronary artery disease [3]. Remarkable advances in the management of coronary artery disease have enhanced the percutaneous interventional approach to LM disease in addition to the traditional role of coronary artery bypass graft surgery [4–6]. Ten-year survival after percutaneous coronary intervention (PCI) has been reported as comparable to surgical revascularization but related to over 40% of major adverse cardiovascular events (MACE) and presenting inferior results to non-LM lesions’ treatment. Patients in whom coronary artery bypass grafting (CABG) is claimed to be favored include age above 72 years, with co-existence of kidney disease or decreased left ventricular ejection fraction (LVEF) [7]. Carvalho et al. [8], in their meta-analysis present comparison between percutaneous and surgical revascularization, indicating no significant differences in all-cause mortality or cardiovascular death but increased risk of any repeated revascularization in the PCI group. In the pooled analysis by Head et al. [9], there was a significant difference between PCI and CABG groups regarding 5-year all-cause mortality, regardless of Syntax score and co-existence of diabetes mellitus. In the systematic review of Feng et al., there was no significant difference in 10-year all-cause mortality between both groups. On the contrary, Sweden’s registry results presented a higher incidence of major adverse cardiovascular and cerebrovascular events in the PCI group within 3.6 years following revascularization [10].
Several trials and observational studies have analyzed the efficacy and safety of CABG and PCI in ischemic heart disease. Regenerative treatment strategies have also been studied, and cardiosurgical access enables direct delivery to the desirable part of the myocardium [11]. Moreover, clinical and procedural early and long-term survival predictors have been investigated. In our previous report, the PREDICT-OPCAB score was developed for 5-year mortality risk in patients with multivessel disease referred for surgical intervention based on the following factors: decreased LVEF <45%, chronic obstructive pulmonary disease (COPD), stroke history and neutrophil-lymphocyte ratio (NLR) above 2.42 [12]. Despite the paucity of data on choosing the optimal revascularization mode for different populations of patients, the long-term results of CABG outcomes related to characteristics of coronary artery disease are lacking. Considering this gap, we conducted a retrospective analysis to analyze long-term results in multivessel and LM groups that underwent off-pump coronary artery bypass grafting.
Aim
The aim of the study was to compare 10-year survival in left main and multivessel off-pump coronary artery bypass grafting. The possible predictive factors for 10-year overall survival were estimated in the patients who underwent off-pump surgery followed by transit time bypass measurements.
Material and methods
Patients
There were 159 patients (128 (81%) men and 31 (19%) women) with a median age of 66 (60–70) years. There were 51 (32%) patients operated on due to left main disease and 108 (68%) more due to complex coronary disease. Inclusion criteria were limited to the study group of patients who were operated in an off-pump technique, and intraoperative transit graft blood flow measurements were performed intraoperatively. The study group was followed up for 10 years survival analysis. The co-morbidities included arterial hypertension in 105 (66%), dyslipidemia in 50 (31%), diabetes mellitus in 43 (27%), and peripheral artery disease in 20 (13%) patients, as presented in Table I. Only patients with preserved left ventricular ejection fraction and with no oncological history were enrolled in the study.
Table I
Demographic and clinical characteristics
| Parameters | Group 1 MVD N = 108 | Group 2 LM N = 51 | P-value |
|---|---|---|---|
| Demographic: | |||
| Male (%)/female (%) | 87 (81)/21 (19) | 41 (80)/10 (20) | 0.98 |
| Age [years] median (Q1–Q3) | 66 (60–70) | 66 (61–70) | 0.10 |
| BMI, median (Q1–Q3) | 28.7 (25.9–31.0) | 27.6 (25.9–31.0) | 0.82 |
| Clinical, n (%): | |||
| Arterial hypertension | 72 (67) | 33 (65) | 0.82 |
| Dyslipidemia | 33 (31) | 17 (33) | 0.73 |
| Diabetes | 34 (32) | 9 (18) | 0.07 |
| IDDM | 9 (8) | 4 (8) | 0.92 |
| COPD | 6 (6) | 1 (2) | 0.31 |
| PAD | 10 (9) | 5 (10) | 0.92 |
| Stroke | 1 (1) | 4 (8) | 0.02* |
| Kidney dysfunction* | 4 (4) | 2 (4) | 0.95 |
| Nicotine | 22 (20) | 16 (31) | 0.13 |
| Angiographic results: | |||
| LMCA > 50%, n (%) | 0 (0) | 51 (100) | < 0.001 |
| LAD, n (%) | 108 (100) | 43 (84) | < 0.001 |
| Cx, n (%) | 86 (80) | 12 (24) | < 0.001 |
| RCA, n (%) | 94 (87) | 0 (0) | < 0.001 |
| Syntax Score | 57 (47–61) | 23 (19–29) | < 0.001 |
| Echocardiographic results: | |||
| Preoperative | |||
| LVED [cm] median (Q1–Q3) | 4.8 (4.2–5.3) | 4.6 (4.3–4.9) | 0.43 |
| LA [cm] median (Q1–Q3) | 3.6 (3.2–3.9) | 3.7 (3.3–4.1) | 0.26 |
| IVS [cm] median (Q1–Q3) | 1.3 (1.1–1.4) | 1.2 (1.0–1.3) | 0.08 |
| RV [cm] median (Q1–Q3) | 2.8 (2.5–3.1) | 2.9 (2.6–3.2) | 0.64 |
| LVEF (%) median (Q1–Q3) | 58 (53–60) | 60 (55–60) | 0.49 |
| Postoperative | |||
| LVED [cm] median (Q1–Q3) | 4.8 (4.2–5.1) | 4.6 (4.3–4.9) | 0.55 |
| LA [cm] median (Q1–Q3) | 3.5 (3.2–3.9) | 3.7 (3.3–4.0) | 0.12 |
| IVS [cm] median (Q1–Q3) | 1.2 (1.1–1.3) | 1.1 (1.0–1.2) | 0.13 |
| RV [cm] median (Q1–Q3) | 2.8 (2.5–3.1) | 2.8 (2.5–3.2) | 0.64 |
| LVEF (%) median (Q1–Q3) | 60 (60–60) | 60 (59–61) | 0.39 |
Methods
All procedures were performed through median sternotomy. The surgical procedure was performed in an off-pump technique (off-pump coronary artery bypass grafting – OPCAB). The anastomosis was performed after local stabilization by OCTOPUS III (Medtronic, USA) and intraluminal shunt application to obtain a bloodless field. The deep pericardial stitch, to elevate the heart, when required, was used. The surgery was performed after heparinization to obtain activated clotting time (ACT) within the range of 350–450 s. The heparin was reversed after procedures by two doses of sulfate protamine. Following the second dose of protamine, transit time flow measurement (TTFM) was obtained with VeriQ™ (Medistim, Oslo, Norway) [13].
Statistical analysis
Continuous variables were reported as medians and interquartile ranges (Q1–Q3) since data did not follow a normal distribution. Categorical data were presented as numbers and percentages. The comparison of interval parameters between proximal and non-proximal groups was performed by the Mann-Whitney test. Categorical data were compared using a χ2 test of independence. Cox regression analysis was performed to identify potential predictors of long-term mortality. Both univariate and multivariable models were used. The multivariable model was assessed using the best subset method. The results were presented as hazard ratio (HR) and its 95% confidence intervals (95% CI). The Kaplan-Meyer curve was also determined to predict long-term mortality in multivessel and left main disease groups.
Results
Clinical characteristics
All patients were operated on through median sternotomy with an off-pump technique. There were no interoperative deaths, and 30-day mortality was 0.6% (1 patient). The median number of performed grafts was 2.2 (2.0–2.4). The arterial revascularization with either both internal mammary artery anastomosis or radial artery was performed in 58 (37%) patients. The detailed information is presented in Table II.
Table II
Intra- and postoperative characteristics
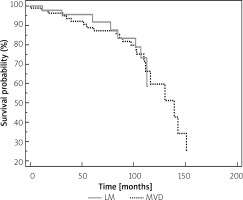
The 5-year mortality risk for left main (LM) and multivessel disease (MVD) were 5% and 9%, respectively. The 10-year mortality risk for LM and MVD treated by OPCAB was not significantly different (36% vs. 37%) (Figure 1).
Transit time graft flow measurement
The results of the transit time graft flow measurements in a left internal mammary artery (LIMA) to the left descending artery (LAD) anastomosis were insignificant between LM and MVD groups with median values of 21 (10-34) ml/min vs 19 (9–38) ml/min, respectively. The median values of the pulsatility index were 3.1 (2.0–4.0) and 3.2 (2.1–3.9) in the LM and MVD groups, respectively. The median values of transit graft flow measurements of the right internal mammary artery (RIMA) to the left descending artery (LAD) were 23 (12–36) ml/min vs. 21 (11–38) ml/min with pulsatility index (PI) of 3.0 (2.1–3.9) and 3.1 (2.2–4.0) in LM and MVD groups, respectively. The comparable results between circumflex artery grafting were observed with median graft flow values of 29 (14-44) ml/min vs. 31 (9–52) ml/min and PI of 2.9 (2.2–4.0) and 3.2 (2.0–4.4), respectively.
Regression analysis for 10-year mortality risk
The univariable analysis followed by multivariable analyses were performed to present possible 10-year mortality risk factors. The demographic and clinical factors followed by transit time flow measurement and perioperative results were taken into consideration and presented in Table III.
Table III
Uni- and multivariable analysis for 10-year mortality prediction
| Parameter | Univariable | P-value | Multivariable | P-value | ||
|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | |||
| Demographic: | ||||||
| Sex (female) | 0.44 | 0.12–0.94 | 0.034* | 1.08 | 1.03–1.14 | 0.001* |
| Age | 1.07 | 1.03–1.13 | 0.002* | |||
| BMI | 1.09 | 1.00–1.20 | 0.053 | |||
| Clinical: | ||||||
| Diabetes | 1.33 | 0.57–3.12 | 0.51 | 6.33 | 1.86–21.52 | 0.003* |
| COPD | 2.97 | 1.03–8.54 | 0.044* | |||
| Dyslipidemia | 1.67 | 0.75–3.72 | 0.21 | |||
| Kidney dysfunction* | 5.65 | 1.68–18.92 | 0.005* | |||
| Arterial hypertension | 2.12 | 1.45–3.09 | 0.051 | |||
| PAD | 4.16 | 0.53–32.81 | 0.17 | |||
| Stroke | 2.55 | 0.40–15.87 | 0.32 | |||
| Nicotine | 1.19 | 0.53–2.84 | 0.69 | |||
| Transit time graft flow measurement: | ||||||
| LIMA flow | 1.01 | 0.99–1.04 | 0.33 | |||
| RIMA flow | 0.95 | 0.84–1.08 | 0.45 | |||
| SVBG flow | 1.01 | 0.98–10.5 | 0.54 | |||
Kaplan-Meyer curve for 10-year mortality risk analysis
There was no significant difference in Kaplan-Meyer 10-year mortality comparison between left main and multivessel disease patients treated by off-pump surgical revascularization (HR = 0.93, 95% CI: 0.40–2.13, p = 0.86) as presented in Figure 1.
Discussion
The results of our analysis present satisfactory results of LM surgical revascularization treated by OPCAB surgery. There was no difference in 10-year survival between patients with multivessel and left main disease referred for the surgical intervention. In Watanabe et al. [14] registry, the comparable 5-year mortality and complication risk was presented between patients who underwent percutaneous coronary revascularization for multiple vessels and CABG, except for a higher risk of reintervention in the PCI arm. Thuijs et al. [15], in their 10-year follow-up Syntax trial, presented a comparable mortality risk of 28% and 27% for PCI interventions in three-vessel and left main disease, respectively. Interestingly, the same analysis exploring long-term results for surgical revascularization revealed a mortality rate of 21% and 28% for three-vessel and left main disease, respectively. The surgical arm included patients who were operated on with or without cardiopulmonary bypass and arterial grafts were recommended but not mandatory. The major strength of our study is the fact that we compared patients who were operated on with an off-pump technique, and its novelty is based on the result of comparable 10-year survival between LM and MVD patients.
Though current guidelines for the left main and multivessel disease revascularization are mostly supported by large, randomized trials including SYNTAX, PRECOMBAT, NOBLE, and EXCEL, the surgical approach is characterized by both techniques including cardiopulmonary bypass administration and off-pump technique. Quin et al. [16] analysis presented comparable 10-year results of both techniques in multivessel disease patients.
Recently, the significance of surgeon experience and center volume has gained much interest, including the number of surgical revascularization procedures performed on a beating heart, which is center-dependent [17]. The latter conclusion is in co-ordinance with a previous report presented by Benedetto et al. [18] and may explain the difference with our analysis. Current presentation confirms the trend of satisfactory results in well-trained centers and may indicate the necessity for center specialization into either on- or off-pump technique. Raja et al. [19] proved that off-pump CABG, performed by experienced surgeons, is associated with both low perioperative risk and satisfactory 20-year survival not affected by the surgical technique.
Alzahrani et al. [20] reported a temporal trend of surgical and percutaneous revascularization in patients with ischemic cardiomyopathy and multivessel coronary artery disease over 12 years. In terms of patient outcomes, a 30-day mortality rate was higher after PCI versus CABG, though similarity was gained/it was similar for CABG and PCI groups, which included completeness of revascularization. In fact, the completeness of revascularization was relatively low in PCI procedures, achieving up to 20.8% in the PCI group and over 93% in the CABG group.
In our analysis we focused on possible long-term mortality risk factors. We performed a multivariable analysis, which pointed out the female sex and diabetes mellitus as possible late mortality risk factors.
In Huckaby et al. [21] study based on patients operated on-pump, the female sex was associated with a lower survival at 1 year but not at 5 years. Interestingly, Sotomi et al. [22] meta-analysis pointed out geographical differences in the treatment strategy, indicating coronary artery bypass favoring in Western countries (SYNTAX trial) and neutral approach in Asian women (PRECOMBAT and BEST trials). Comparing the PCI approach to surgical revascularization in the female population with multivessel disease, lower 6-year mortality was presented [23].
Our regression analysis pointed out to diabetes as a possible risk factor for increased long-term mortality. Surgery is preferred over percutaneous intervention in diabetic patients due to lower reintervention risk in LM disease [24]. On the contrary, no difference between drug-eluting stent-based PCI and CABG for all-cause mortality among diabetic patients in observational studies was noticed in d’Entremont et al. meta-analysis [25]. Aeen et al. [26] did not reveal significant differences in mortality or in the complication rates between groups with or without diabetes. Our previous analyses did not find a predictive role of diabetes for long-term survival following off-pump grafting [27, 28].