Introduction
Soft-tissue sarcomas (STS) are rare malignancies, comprising less than 1% of malignant tumours in adults [1]. Liposarcoma is a type of STS deriving from the adipose tissue, and accounts for 15% of all STSs. It is the second most common STS after malignant fibrous histiocytoma (recently renamed as undifferentiated pleomorphic sarcoma) [2]. Liposarcoma has distinct histopathological subtypes; well differentiated, myxoid, pleomorphic, and dedifferentiated, with the first being the most common [3, 4].
Liposarcoma is frequently located in the lower limbs and retroperitoneum, although it can rarely be found in the head and neck region. Less than 1% of primary liposarcomas are located in the head and neck, and less than 0.3% are located in the oral region [3, 5]. A recent systematic review gathered 104 primary liposarcomas of the oral cavity [5–8]. Even fewer reports of metastatic liposarcomas to the head and neck region have been published. A recent literature review comprised 16 reports [9].
The aim of this paper is to present a case of metastatic myxoid liposarcoma to the tongue of a patient with primary scrotal location, recording the first patient with metastasis of liposarcoma to the tongue.
Case report
A 78-year-old patient presented with a firm exophytic mass of the left dorsal surface of the tongue, sized 4 × 4.5 cm (Fig. 1). Mild oedema and light bleeding were his main symptoms. The patient had a history of myxoid liposarcoma of the scrotum with two surgical excisions seven and six years ago and concomitant radiotherapy and chemotherapy with ifosfamide-etoposide-mesna. Two years later the patient had a lung metastasis and received immunotherapy with trabectedin, but due to adverse reactions, he continued treatment with targeted therapy (pazopanib) up to the day of examination in our department.
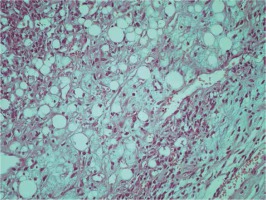
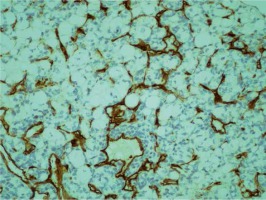
An MRI was performed, describing an exophytic solid mass on the dorsal surface of the tongue sized 4–4.5 cm (Fig. 2). A biopsy was taken, and the histopathology report presented a malignant neoplastic process with morphological features of a myxoid liposarcoma, with uniformly round to oval shaped primitive non-lipogenic mesenchymal cells and signet-ring lipoblasts in a prominent myxoid stroma, with rich “chicken-wire” capillary vasculature (Figs. 3 and 4). The patient was referred to his oncologist for systemic evaluation and therapy.
Fig. 2
MRI, T2-weighted image, axial plane. A lesion sized 4–4.5 cm on the dorsal surface of the tongue is imaged

Discussion
A typical presentation of a liposarcoma is a slow growing, firm, yellowish mass, well circumscribed, most commonly appearing in the fourth to sixth decade of life. Signs of necrosis with haemorrhagic features are not uncommon. Myxoid liposarcoma is the commonest type and is believed to have the mildest biological behaviour because the rate of distant metastasis is considered low. Myxoid liposarcoma has a relatively good prognosis, with a five-year survival rate of 80–90%. In liposarcomas of the oral cavity, survival rates are calculated at 66.4% [8]. There is a high incidence of local recurrence of up to 33% [2, 5]. In general, liposarcomas tend to metastasise to the lungs, whereas the myxoid type can appear with extrapulmonary metastasis [2, 10]. Nodal metastases are rare with primary liposarcomas of the head and neck region, as well as with any type of primary liposarcoma [7, 11]. A systematic review published on primary oral liposarcomas reported a 2% incidence of distal metastases [8].
The subcutaneous tissue of the head and neck is considered the most common site of head and neck liposarcomas. The most common sites of primary intraoral liposarcomas are the tongue, cheek, and buccal mucosa. Reports have been published on cases affecting the floor of the mouth, lip, palate, and gingiva [8, 12].
According to McElderry et al. [9], very few cases of metastatic liposarcomas to the head and neck region have been published. Their case concerns a dedifferentiated liposarcoma of the left shoulder of a 68-year-old male patient metastasising to the gingival mucosa. This seems to be the only intraoral metastatic liposarcoma recorded. The remaining 15 cases recorded concern metastasis to the orbits (five cases), thyroid (four cases), dura mater (three cases), submandibular region (one case), neck (one case), and scalp (one case).
Pathological diagnosis of a liposarcoma in the head and neck region may be challenging for the histopathologist due to the rarity of this location. A wide differential diagnosis can be included; myxoma, myxosarcoma, myxofibrosarcoma, lipoma, or undifferentiated pleomorphic sarcoma [2, 8]. In our case, the pathological specimen had all the typical characteristics of a myxoid liposarcoma, providing a definitive diagnosis for the patient.
Typical therapy of a liposarcoma is a wide surgical excision. As far metastatic sites are concerned, data are very limited. From the aforementioned cases, nine were managed surgically, and one received radiotherapy only. The remaining reports do not define the course of therapy. Our patient could not be managed surgically due to the size of the lesion. Thus, the decision of referring the patient to his oncologist for continuation of systemic therapy was made.
Conclusions
In conclusion, with this report we add a new metastatic location of a myxoid liposarcoma to the literature, recording a patient with metastatic myxoid liposarcoma to the tongue, with primary location to the scrotum. To our knowledge, this is the first reported case of a myxoid liposarcoma metastasis to the tongue, and the second report of any type of liposarcoma metastasis to the oral cavity.