Introduction
Pancreatic necrosis caused by infection is a serious and potentially fatal consequence of acute pancreatitis. Pancreatic tissue necrosis and subsequent infection result in systemic inflammation and subsequent organ failure. Managing infected pancreatic necrosis presents considerable difficulties since it frequently necessitates invasive interventions to manage the infection and avert additional problems [1, 2].
Historically, the predominant method for managing infected pancreatic necrosis has been open surgical surgery, characterized by a substantial abdominal incision and extensive tissue dissection [2]. Nevertheless, this methodology is linked to significant rates of illness and death, along with extended periods of hospitalization and an increased likelihood of complications [3].
In the past several years, there has been a rise in the utilization of endoscopic intervention and minimally invasive surgery as alternate approaches for the treatment of infected pancreatic necrosis [4, 5]. The execution of endoscopic intervention entails the utilization of flexible endoscopes to gain entry into the necrotic pancreatic tissue and extract the infectious material. The utilization of this method provides the benefit of being less intrusive in comparison to open surgery, leading to decreased illness and expedited recuperation periods [6]. Nevertheless, endoscopic intervention is constrained, particularly when the necrotic tissue is situated beneath the abdominal cavity or encompasses intricate anatomical formations [7].
The utilization of minimally invasive surgery suggests a potentially advantageous strategy for managing infected pancreatic necrosis. The methodology encompasses the utilization of laparoscopic or robotic-assisted methodologies to gain entry to the contaminated tissue and extract it via little incisions [8, 9]. Minimally invasive surgery presents several advantages in comparison to open surgery, including diminished patient trauma, decreased postoperative pain, abbreviated hospital stays, and enhanced cosmetic results [10]. Moreover, it facilitates a more thorough and accurate elimination of the diseased necrotic tissue, hence diminishing the likelihood of recurring infections.
This meta-analysis intended to compare the outcomes of endoscopic intervention and minimally invasive surgery in the management of infected pancreatic necrosis, based on the developing data supporting their usage. Our objective was to conduct a thorough assessment of the effectiveness, safety, and clinical results of minimally invasive surgery in comparison to endoscopic intervention for the treatment of infected pancreatic necrosis, by integrating the existing data from pertinent research.
It is imperative to comprehend the benefits and constraints associated with both methodologies in order to enhance patient outcomes and facilitate informed clinical decision-making. The objective of this meta-analysis was to fill the existing knowledge gap and provide a valuable contribution to the expanding body of evidence regarding the most effective approach to managing infected pancreatic necrosis.
Aim
A comparison of the results of endoscopic and minimally invasive surgical treatment for infected necrotizing pancreatitis is the goal of this study, which is based on the findings of randomized controlled trials.
Material and methods
Study design
Meta-analyses of clinical trials that are now being conducted were incorporated into the epidemiological declaration and had a predetermined process for the study. For the purpose of data gathering and analysis, a wide range of databases were searched. These databases included OVID, PubMed, Embase, Cochrane Library, and Google Scholar.
Data pooling
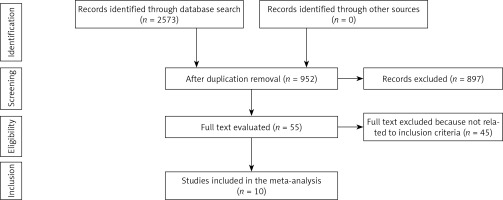
For the purpose of analyzing the effects of various clinical outcomes, prospective clinical trials were utilized with the objective of evaluating the influence of endoscopic and minimally invasive surgical treatment for infected necrotizing pancreatitis. For the purpose of this study, only prospective trials including human participants were included. The number of participants in the studies that were recruited was not limited in any way. Review articles, editorials, and letters were not included in the current meta-analysis since they were considered to be non-interventional studies. A visual representation of the entire process of study identification can be found in Figure 1.
Eligibility and inclusion
Analyzing the impact of endoscopic and minimally invasive surgical treatment for infected necrotizing pancreatitis was the main topic for studies to be eligible for inclusion in the meta-analysis.
Sensitivity analysis comprised only papers reporting the impact of interventions on mortality rate, complications, organ failure, pancreatic fistula, organ perforation during the surgical procedure, hernia, bleeding, and hospital stay. A range of parameters were compared between the studied groups for subclass and sensitivity analysis.
For an article to be considered for inclusion in the meta-analysis, it was required to fulfill all of the inclusion criteria listed below:
the studies should be prospective clinical trials,
the target intervention subjects consisted of patients with infected pancreatic necrosis receiving two or more different interventions including minimally invasive surgery and endoscopic procedures.
The exclusion criteria were:
Identification
According to the PICOS principle, a protocol of search strategies was developed and defined as follows: P (population) infected pancreatic necrosis patients; I (intervention/exposure): invasive technique treatment whether endoscopy or minimally invasive surgery, C (comparison): endoscopy versus minimally invasive surgery. O (outcome): mortality rate, number of complications, organ failure rate, incision hernia, pancreatic fistula, hospital stay, endocrine function, and organ perforation, S (study design): prospective clinical studies.
Following a review of the titles and abstracts of all the articles that had been compiled in reference management software, any research that did not relate to the various intrusive techniques for controlling infected pancreatic necrosis was excluded after being reviewed by two authors independently. This review was carried out.
Screening
The data were refined based on specific criteria, which encompassed various aspects. These included the standard format of the study and subject-related features, the first author’s name, the study period, the year of publication, the country of study, the study design, the population type recruited, the total number of subjects, the qualitative and quantitative evaluation methods, demographic data, clinical and treatment characteristics, information source, outcome evaluation, and statistical analysis. The bias of each study was analyzed, and the methodological rigor of the selected studies was appraised by two authors in a blinded manner.
Statistical analysis
Within the context of the present meta-analysis, a random-effect model was utilized to compute the mean difference (MD) along with a confidence interval (CI) of 95%. The random model was used to assess all of the groups since some of the groups had a high degree of heterogeneity, and other groups had methodology that had inconsistencies. A percentage was used to calculate the I2 index, which is a numeric value that can range from 0 to 100. Indicating the absence of heterogeneity were percentages that ranged from 0% to 25% to 50% to 75%. Additionally, percentages indicating low, moderate, and high heterogeneity were also included in this description. According to what was mentioned earlier, the initial evaluation was stratified into several result categories, and then subcategory analysis was carried out. Begg’s test was used to conduct a quantitative investigation of publication bias, and publication bias was determined to be present if the p-value was greater than 0.05. An analysis with two tails was carried out in order to obtain the p-values. Jamovi was the program that was utilized in order to make the graphs and statistical analysis visible.
Results
Findings of systemic research resulted in the recruitment of ten trials [5, 11–19] published between 2012 and 2024 investigating the impact of endoscopic intervention compared with a minimally invasive technique for managing infected pancreatic necrosis. Characteristics of included trials are presented in Table I and findings of analysis are presented in Table II and Figures 2 and 3.
Table I
Characteristics of analyzed studies
Table II
Results of analysis of heterogeneity and publication bias
Figure 2
Forest plot showing the impact of endoscopic intervention compared with minimally invasive surgery for infect pancreatic necrosis patients regarding mortality rate (A), complication (B), new-onset organ failure (C), pancreatic fistula (D), postoperative bleeding (E), and perforation of a visceral organ (F)

Figure 3
Forest plot showing the impact of endoscopic intervention compared with minimally invasive surgery for infected pancreatic necrosis patients regarding endocrine insufficiency (A), incisional hernia (B), and hospital stay (C)

Mortality
The dichotomous analysis model includes nine studies comparing the impact of different interventions (minimally invasive surgery versus endoscopy) on the mortality rate of patients with infected necrotizing pancreatitis. The findings of the analysis revealed no significant (p = 0.35) difference between groups regarding the number of deaths. Study outcomes appear to be heterogeneous (I² = 54.45%), MD = –-0.40, 95% CI [–1.24, 0.44] (Figure 2 A). Publication bias analysis showed a non-significant p-value according to Begg’s and Egger’s tests.
Complications
The dichotomous analysis model includes nine studies comparing the impact of different interventions (minimally invasive surgery versus endoscopy) on the number of major complications expressed by patients with infected necrotizing pancreatitis. The findings of the analysis revealed a significant (p = 0.006) difference between groups regarding the number of complications. The complication rate for endoscopic intervention was significantly lower than that of minimally invasive surgery. MD = –1.01, 95% CI [–1.74, –0.28] (Figure 2 B). Publication bias analysis showed a non-significant p-value according to Begg’s test while Egger’s test showed significant publication bias (0.002); hence the overall publication bias for this model is considered significant.
New-onset organ failure
The analysis model includes seven studies using random dichotomous analysis, comparing the impact of minimally invasive surgery versus endoscopy on the number of new-onset organ failures expressed by patients with infected necrotizing pancreatitis. The findings of the analysis revealed a significant (p < 0.001) difference between groups. The number of new-onset organ failures for endoscopic intervention was significantly lower than that of minimally invasive surgery. MD = –1.00, 95% CI [–1.50, –0.50] (Figure 2 C). Publication bias analysis showed a non-significant p-value according to Begg’s and Egger’s (Table II) but with low values.
Pancreatic fistula
The analysis model includes seven studies using random dichotomous analysis, comparing the impact of minimally invasive surgery versus endoscopy on the onset of postoperative pancreatic fistula expressed by patients with infected necrotizing pancreatitis. The findings of the analysis revealed a significant (p < 0.001) difference between groups. The incidence of new-onset organ failures for endoscopic intervention was significantly lower than that of minimally invasive surgery. MD = –2.21, 95% CI [–2.99, –1.42] (Figure 2 D). Publication bias analysis showed a non-significant p-value according to Begg’s and Egger’s (Table II) but with low values.
Postoperative bleeding
This model includes six studies comparing the clinical influence of minimally invasive surgery versus endoscopy on postoperative bleeding for patients with infected necrotizing pancreatitis. The findings of the analysis revealed no significant (p = 0.59) difference between groups regarding the incidence of postoperative bleeding that required medical intervention. Study outcomes appear to be non-heterogeneous (I² = 0%), MD = –0.16, 95% CI [–0.73, 0.41] (Figure 2 E). Publication bias analysis showed a low, non-significant p-value according to Begg’s and Egger’s tests.
Perforation of a visceral organ
Eight studies that compared the clinical influence of minimally invasive surgery versus endoscopy on the perforation of a visceral organ for patients with infected necrotizing pancreatitis were analyzed in this random model. The findings of the analysis reflected no significant (p = 0.057) difference between groups regarding the incidence of perforation of a visceral organ. Study outcomes appear to be non-heterogeneous (I² = 0%), MD = –0.61, 95% CI [–1.23, 0.02] (Figure 2 F). Publication bias analysis showed a low, non-significant p-value according to Begg’s and Egger’s tests.
Endocrine insufficiency
Six studies that compared the clinical influence of minimally invasive surgery versus endoscopy on endocrine insufficiency for patients with infected necrotizing pancreatitis were analyzed in this random model. The findings of the analysis revealed no significant (p = 0.53) difference between groups regarding the occurrence of endocrine insufficiency. Study outcomes were expressed as MD = –0.40, 95% CI [–1.63, 0.84] (Figure 3 A). Publication bias analysis showed a low, non-significant p-value according to Begg’s and Egger’s tests.
Incisional hernia
Four studies that compared the clinical influence of minimally invasive surgery versus endoscopy on incisional hernia for patients with infected necrotizing pancreatitis were analyzed in this random model. The findings of the analysis revealed no significant (p = 0.14) difference between groups regarding the occurrence of incisional hernia. Study outcomes were expressed as MD = –1.04, 95% CI [–2.43, 0.35] (Figure 3 B). Publication bias analysis showed a low, non-significant p-value according to Begg’s and Egger’s tests.
Hospital stay
Six studies investigating the clinical influence of minimally invasive surgery versus endoscopy on hospital stay for patients with infected necrotizing pancreatitis were analyzed in this continuous random model. The findings of the analysis revealed no significant (p = 0.42) difference between groups regarding hospital stay. Study outcomes were expressed as MD = –0.52, 95% CI [–1.79, 0.75] (Figure 3 C). One of the six studies, Angadi et al., indicated a significant impact of surgery on decreasing hospital stay compared with endoscopy, while Kumar et al. reported that hospital stay was lower with endoscopy. Publication bias analysis showed a low, non-significant p-value according to Begg’s and Egger’s tests.
Discussion
Ten studies have been included in the current investigation (published between 2012 and 2024). Endoscopic procedures demonstrated considerable beneficial outcomes in comparison to minimally invasive surgery, particularly in terms of the number of complications that occurred after the operation (p = 0.006), the occurrence of new-onset organ failure (p < 0.001), and the presence of pancreatic fistula (p < 0.001). On the other hand, there was no discernible difference between the two procedures in terms of the average length of stay in the hospital, postoperative hemorrhage, incisional hernia, endocrine insufficiency, or perforation of a visceral organ.
A previous study by Szeliga et al., comparing the impact of three different types of minimally invasive procedures, showed that the hospitalization time ranged from 10 to 192 days. The type 1 (classic necrosectomy with repeated peritoneal flushing) procedures exhibited the highest mortality rate. No statistically significant differences were seen in the absolute number of postoperative complications across the three interventional groups (classic necrosectomy with repeated peritoneal flushing, laparotomy with active drainage, and video-assisted retroperitoneal debridement). However, there was variation in the quality of these complications. Traditional techniques were employed in patients with more severe general and local conditions [20]. Another study investigating the impact of endoscopic interventions for management of acute biliary pancreatitis showed that the utilization of endoscopic retrograde cholangiopancreatography for the management of acute biliary pancreatitis was linked to the alleviation of abdominal pain, expedited intestinal expulsion and recovery of serum amylase levels, as well as significant improvements in serum biochemical parameters and inflammatory factor levels [21].
Over the past 10 years, minimally invasive procedures have largely supplanted conventional open necrosectomy in an effort to diminish the negative health outcomes and death rates linked to open necrosectomy. In addition to percutaneous drainage and minimally invasive surgery, other studies have documented endoscopic transgastric drainage and necrosectomy as viable alternatives to open surgery [22–25]. Despite the growing prevalence of endoscopic intervention for pancreatic necrosis, there is still insufficient evidence to support the advantage of ETA over SA. Endoscopy has been shown to have clinical superiority in only a few observational studies [24, 26] and a modest randomized controlled trial [19]. Additionally, a total of three single-arm systematic studies [26, 27] have demonstrated that endoscopic transgastric necrosectomy is a secure and efficient minimally invasive intervention for necrotizing pancreatitis. The paper did not provide evidence supporting the advantage of the endoscopic step-up method in terms of lowering significant mortality in patients with infected necrotic pancreatitis. However, it did recommend that further investigations be carried out to validate the findings of the completed trials. In order to demonstrate the superiority of endoscopy, we conducted the initial meta-analysis to assess and evaluate the efficacy and safety of the two methods. The pooled proportion of effective resolution of pancreatic necrosis by endoscopic transgastric necrosectomy in previous single-arm systematic reviews was approximately 80%. Consistent with prior comprehensive reviews [16, 17], the endoscopic group had a significant clinical resolution rate in our systematic review. In the interim, the minimally invasive surgery exhibited a comparable rate of clinical resolution. Furthermore, as indicated by this systematic review, the observed decrease in the incidence of significant complications following endoscopic compared to the surgery group aligns with findings from prior research [16–18]. Endoscopic trans-gastric procedures have the potential to minimize surgical trauma and decrease the occurrence of problems such as new-onset organ failure, pancreatic fistula, and incisional hernia by avoiding laparotomy and general anesthesia [15]. Moreover, it is widely recognized that general anesthesia has the potential to elicit or extend systemic inflammation in patients who are critically ill.
Although the meta-analysis did not reveal any significant differences in death rates between the two groups, this might have been because there have only been a limited number of studies that have investigated the differences between these two approaches. In addition, it has been demonstrated that patients with infected necrotic pancreatitis who have new onset single organ failure have a significantly higher death rate than patients who do not have new organ failure. When compared to individuals who do not have new organ failure, the differences related to higher rates of new-onset multiple organ failure are particularly significant [28].
There is a significant probability that this is also the case with multiple organ failure. It is possible that the increased inflammatory stress response that the surgical treatment induces in patients is the underlying cause of this probably higher rate of organ failure in individuals who have undergone surgical treatment. This additional inflammatory response has the potential to either exacerbate organ failure that is already present or give rise to new organ failure in patients who are already in a critical condition [29]. In addition, the surgical group experienced a significantly higher number of cases of perforations of visceral organs or enterocutaneous fistulae, whereas the endoscopic group experienced a shorter length of stay in the hospital.
Conclusions
When it comes to complications, new-onset organ failure, and pancreatic fistula, endoscopic therapy appears to have the potential to offer advantages over minimally invasive surgery. On the other hand, there is no difference between the two therapies with regard to the remaining clinical criteria. However, future clinical multicenter randomized trials are needed.